- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Chronic obstructive pulmonary disease (COPD) is a lung disease characterised by persistent respiratory symptoms and airflow obstruction. COPD is a triad of emphysema, chronic bronchitis and small airway fibrosis. Chronic bronchitis is defined as a productive cough for at least 3 months in 2 consecutive years.1 In the UK, the prevalence of COPD is approximately 3 million, and the mortality rate is 30,000 per year.2 Furthermore, COPD accounts for 1.4 million GP appointments annually and is the second-largest cause of emergency admissions in the UK.3 COPD is a very common and important topic, which doctors in all medical disciplines must be familiar with.
Risk factors
- Tobacco smoking: associated with 80% of COPD cases4
- Indoor air pollution: this usually occurs in the developing world, where biomass is burnt inside homes for cooking and heating
- Alpha-1 antitrypsin deficiency: an autosomal dominant condition which presents in younger patients (aged 20-40). Alpha-1 antitrypsin is a protease inhibitor with one of its actions being to prevent neutrophil elastase from breaking down alveolar structures. Therefore, a deficiency in alpha-1 antitrypsin leads to the increased destruction of alveolar structures, resulting in early-onset emphysema.5 Some cases of alpha-1 antitrypsin deficiency involve impaired secretion of alpha-1 antitrypsin by the liver, resulting in accumulation of it in the liver, and therefore cirrhosis.
Clinical features
History
Presenting complaint
COPD patients present with progressive dyspnoea and chronic productive cough.
History of presenting complaint
- Dyspnoea: initially exertional, but can progress to resting dyspnoea over the course of the condition (months to years). Dyspnoea is graded using the Medical Research Council (MRC) dyspnoea scale (Table 1)
- Chronic productive cough: usually colourless sputum, which may become green during lower respiratory tract infections (LRTIs)
- Recurrent LRTIs
- Fatigue
- Headache (due to CO2 retention)
Table 1. MRC Dyspnoea Scale. Used with the permission of the MRC6
| Grade | Level of Activity |
| 1 | Breathless during strenuous exercise only |
| 2 | Breathless when hurrying or walking up a slight incline |
| 3 | Walks slower than people of the same age due to dyspnoea, or needs to pause for breath when walking at own pace |
| 4 | Pauses for breath after walking 100m/a few minutes on the level |
| 5 | Too breathless to leave the house, or breathless when dressing |
It is also important to assess the impact of the patient’s COPD on their wellbeing and daily life, using the COPD Assessment Test (CAT) (Table 2).
Table 2. The CAT. Scores range from 0-40; higher scores indicate a greater impact of COPD on the patient’s daily life7
| SCORE | |||
| I never cough | 1 2 3 4 5 | I cough all the time | |
| I have no phlegm in my chest at all | 1 2 3 4 5 | My chest is full of phlegm | |
| My chest does not feel tight at all | 1 2 3 4 5 | My chest feels very tight | |
| When I walk up a hill or flight of stairs, I am not out of breath | 1 2 3 4 5 | When I walk up a hill or flight of stairs, I am completely out of breath | |
| I am not limited to doing any activities at home | 1 2 3 4 5 | I am completely limited to doing any activities at home | |
| I am confident leaving my home despite my lung condition | 1 2 3 4 5 | I am not confident leaving my home at all despite my lung condition | |
| I sleep soundly | 1 2 3 4 5 | I do not sleep soundly because of my lung condition | |
| I have lots of energy | 1 2 3 4 5 | I have no energy at all | |
| TOTAL SCORE | /40 | ||
Past medical history
- Previous exacerbations or hospitalisations
- Medical comorbidities, including lung disease (such as asthma)
- Psychiatric comorbidities, including depression and anxiety
- Previous operations
Medication/allergies
- Regular medications (and any recent changes) *ACE-inhibitors can cause a dry cough
- Over-the-counter medications
- Allergies
Family history
- Lung disease
- Liver disease (may suggest alpha-1 antitrypsin deficiency)
Social history
- Smoking history: quantify in pack-years (1 pack-year = smoking 20 cigarettes a day for a year)
- Alcohol history
- Recreational drug use
- Occupation: may be exposed to indoor air pollution
Examination
A full respiratory examination should be performed in suspected cases of COPD. See the Geeky Medics guide here.
Most common findings
- Tachypnoea: due to an increased neural respiratory drive to breathe
- Wheeze on auscultation: due to inflammatory airway oedema and mucous obstructing the airway
- Pursed lips breathing: to increase airway resistance and therefore reduce expiratory flow limitation
Less common findings
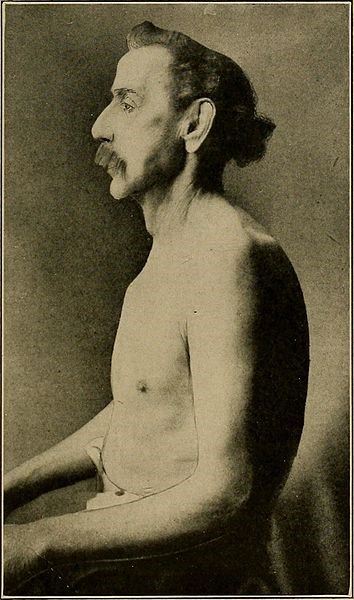
- Barrel chest (Figure 1): due to gas trapping
- Peripheral cyanosis (Figure 2)
- Cor pulmonale (signs of right heart failure, such as peripheral oedema and hepatomegaly): due to pulmonary hypertension, which results from chronic hypoxic pulmonary vasoconstriction
- CO2 retention flap: while the exact mechanism is unknown, some hypothesise that it is due to abnormal function of the diencephalon (which acts as a relay centre for sensory and motor impulses)8

Differential diagnoses
Dyspnoea and productive cough have important differential diagnoses. Table 3 outlines these differential diagnoses, and the features which differentiate them from COPD.
Table 3. Differential diagnoses of COPD
| Differential diagnosis | Features differentiating from COPD |
| Asthma |
*Note that COPD and asthma can co-exist |
| Bronchiectasis |
|
| Congestive cardiac failure |
|
| Lung cancer |
|
| Tuberculosis |
|
Investigations
Bedside investigations
Spirometry
- Typical finding in COPD: FEV1/FVC < 70%
- FEV1 is also used to classify the severity of COPD (Table 4)9
- See the Geeky Medics spirometry interpretation guide for further information
Table 4. Severity grading of COPD
| Severity of COPD | FEV1 |
| Mild | >80% |
| Moderate | 50-80% |
| Severe | 30-50% |
| Very Severe | <30% |
Pulse oximetry
- Aim for SpO2 of 88-92%
- Avoid administering excessive amounts of O2:
- O2 displaces CO2 in haemoglobin, which increases CO2 in the blood
- Increased CO2 in the blood cannot be removed due to failure of alveolar ventilation in emphysema, leading to hypercapnic respiratory failure
Other investigations
- Sputum culture: enables targeted antibiotic therapy during exacerbations of COPD
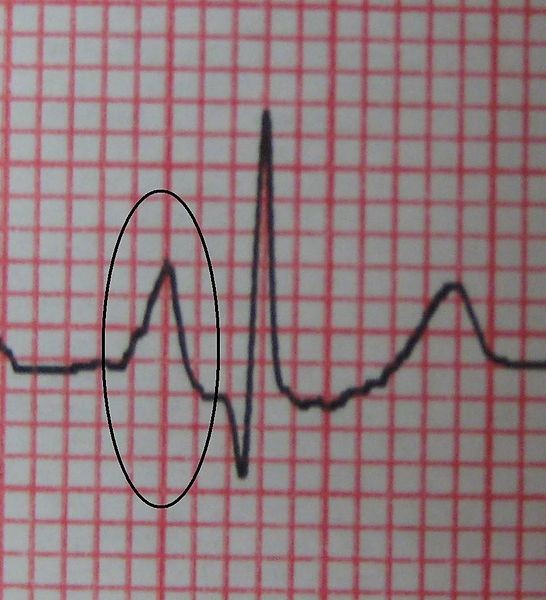
- ECG: cor pulmonale (peaked p waves and right axis deviation) (Figure 3)
Laboratory investigations
- Baseline blood tests: FBC, U&E, LFTs, CRP
- Arterial blood gas (ABG)
- During stable disease: PaCO2 >6.0 and bicarbonate >30 indicates that the patient is a “CO2-retainer”
- During exacerbations: check for respiratory acidosis (PaCO2 >6.0 and pH <7.35)
Imaging
- Chest X-ray: hyperinflation10
- >6 anterior ribs or >10 posterior ribs visible in the mid-clavicular line
- Flattened diaphragm
- Hyperlucent lungs

Management (long-term)
*For further information on the management of acute exacerbations of COPD, see here.
Conservative management
- Smoking cessation: see the Geeky Medics guide on smoking cessation for useful tips
- Pulmonary rehabilitation
- Annual influenza vaccine and one-off pneumococcal vaccine
- Personalised self-management plan
Medical management
Inhalers
Medical management of COPD is largely administered through inhalers, with a step-up process as needed (Figure 4).
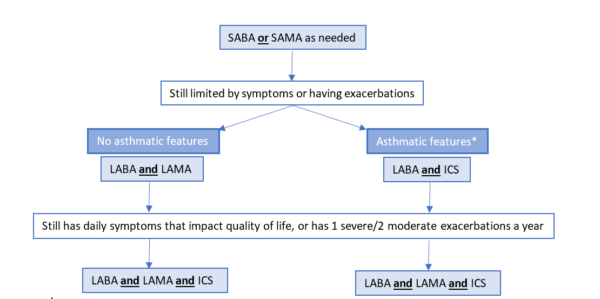
*Note that some clinicians prefer to use the international GOLD guidelines for the management of COPD, so please ensure that you know which guidelines your medical school will use for your examinations.9
Long-term oxygen therapy
- Indications (one of the following):
- SpO2 <88%
- PaO2 <7.3kPa
- Contraindicated in current smokers due to the risk of explosion and/or burns
Surgical management
- Lung volume-reduction surgery: for very severe COPD, which does not respond to optimal medical management
- Lung transplantation: if not suitable for other surgical options
Complications
- Hypercapnic respiratory failure (PaO2 < 8.0 and PaCO2 > 6.0)
- Secondary polycythaemia (raised haemoglobin): due to chronic hypoxaemia
- Cor pulmonale: right heart failure, caused by pulmonary hypertension as a result of chronic hypoxic pulmonary vasoconstriction
- Bronchiectasis: due to chronic and repeated infections
- Anxiety and depression
- Osteoporosis: due to chronic steroid use, smoking, lack of bone-strength exercise and vitamin D deficiency
- Sleep disturbance
Key points
- COPD is a triad of emphysema, chronic bronchitis and small airway fibrosis.
- The main risk factors are tobacco smoking and inhaled pollutants.
- COPD presents with progressive dyspnoea and productive cough.
- Diagnosis is based on clinical features + spirometry (FEV1/FVC <70%).
- Management consists of conservative measures (such as smoking cessation) and inhaled bronchodilators.
- Complications include respiratory failure and cor pulmonale.
References
- National Institute for Health and Care Excellence. Chronic Obstructive Pulmonary Disease in Over 16s: Diagnosis and Management. Published in 2018. Available from: [LINK]
- Health and Safety Executive. Chronic Obstructive Pulmonary Disease (COPD) Statistics in Great Britain. Published in 2019. Available from: [LINK]
- National Institute for Health and Care Excellence. Quality Standards and Indicators: COPD. Published in 2015. Available from: [LINK]
- Rabe KF and Watz H. Chronic Obstructive Pulmonary Disease. Published in 2017. Available from: [LINK]
- Kalfopoulos M et al. Pathophysiology of Alpha-1 Antitrypsin Lung Disease. Methods in Molecular Biology. Published in 2017. Available from: [LINK]
- Medical Research Council. MRC Dyspnoea Scale. Published in 1960. Available from: [LINK]
- Jones PW et al. Development and First Validation of the COPD Assessment Test. European Respiratory Journal. Published in 2009. Available from: [LINK]
- Mendizabal M and Silva MO. Images in Clinical Medicine: Asterixis. Published in 2010. Available from: [LINK]
- Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management and Prevention of COPD. Published in 2020. Available from: [LINK]
- Bickle I. Hyperinflated Lungs. Published in 2018. Available from: [LINK]
- National Institute for Health and Care Excellence. Chronic Obstructive Pulmonary Disease in Over 16s: Diagnosis and Management. Published in 2018. Available from: [LINK]
- Cabot R. Barrel chest. CC BY-SA. Available from: [LINK]
- Fletcher W. Peripheral cyanosis. CC BY-SA. Available from: [LINK]
- Heilman J. P pulmonale. CC BY-SA. Available from: [LINK]
- James Heilman, MD. COPD chest x-ray. Published August 2010. Licence: CC BY-SA. Available from: [LINK]
Reviewer
Dr Neeraj Shah
Respiratory Medicine Registrar
Editor
Hannah Thomas
Feedback!
Please click here to fill out the feedback form, which should take less than 1 minute of your time. Feedback is vital as it allows authors to improve their articles, leading to even better content on Geeky Medics!