- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Rectal (PR) examination frequently appears in OSCEs and you’ll be expected to identify relevant signs using your clinical examination skills. This guide provides a step-by-step approach to performing a rectal examination in an OSCE setting, with an included video demonstration.
Gather equipment
Gather the appropriate equipment:
- Non-sterile gloves
- Apron
- Lubricant
- Paper towels
Introduction
Wash your hands and don PPE if appropriate.
Introduce yourself to the patient including your name and role.
Confirm the patient’s name and date of birth.
Explain what the examination will involve using patient-friendly language: “Today I need to perform a rectal examination. This will involve me inserting a finger into your anus to feel for any abnormalities. It shouldn’t be painful, but it will feel a little uncomfortable. You can ask me to stop at any point.”
Explain the need for a chaperone: “One of the other staff members will be present throughout the examination, acting as a chaperone, would that be ok?”
Gain consent to proceed with the examination: “Do you understand everything I’ve said? Do you have any questions? Are you happy for me to carry out the examination?”
Ask the patient if they have any pain before proceeding with the clinical examination.
Explain to the patient that they’ll need to remove their underwear and lie on the clinical examination couch, covering themselves with the sheet provided. Provide the patient with privacy to undress and check it is ok to re-enter the room before doing so.
Preparation
1. Don an apron and a pair of non-sterile gloves.
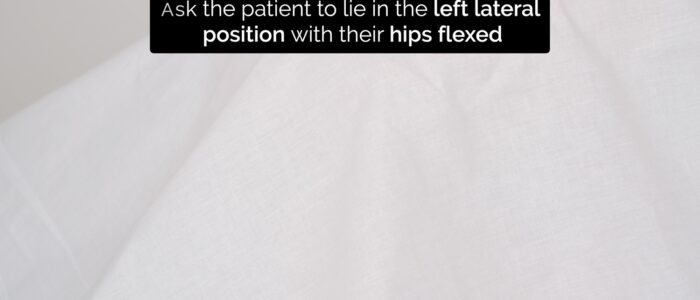
2. With the clinical examination couch flat, ask the patient to lie down in the left lateral position with their knees bent up towards their chest.
3. Then ask the patient if it is ok to remove the sheet to begin the examination.
Inspection
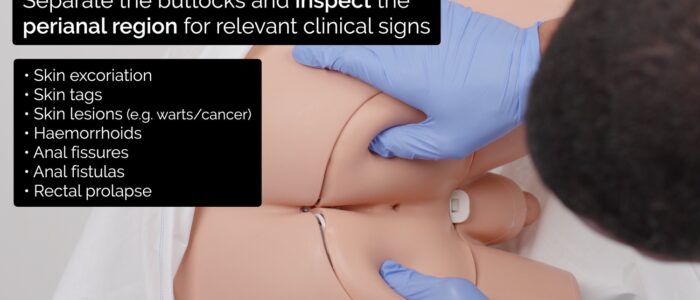
Separate the buttocks and inspect the perianal region for relevant clinical signs:
- Skin excoriation: secondary to anal pruritis which can be caused by haemorrhoids, faecal incontinence or constipation.
- Skin tags: minor projections of skin at the anal verge that are usually benign. Perianal skin tags can, in some cases, be associated with Crohn’s disease.
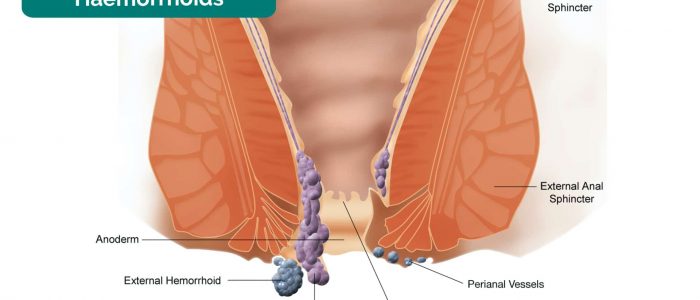
- External haemorrhoids: located below the dentate line and innervated by somatic nerves. On examination, they typically appear as a lump located just inside or outside the anal verge.
- Anal fissure: a tear in the tissue of the anal canal, typically located posteriorly in the midline. Anal fissures most commonly develop secondary to constipation and are very painful (often making rectal examination impossible).
- External bleeding: may be caused by external haemorrhoids, anal cancer or brisk gastrointestinal bleeding.
- Anal fistula: a chronic abnormal communication between the internal anal canal and the perianal skin. Fistulae may discharge pus and have surrounding inflammation. Causes of anal fistulae include perianal Crohn’s disease, chronic anal abscess and diverticulitis.
- Irregular growths: may be due to anal warts or anal cancer.
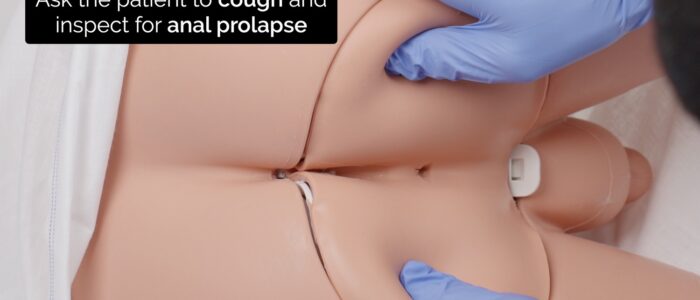
Ask the patient to cough and inspect for:
- Rectal prolapse: on inspection, a mass with concentric rings of mucosa will be visible protruding through the anus.
- Internal haemorrhoids: located above the dentate line and innervated by visceral nerves. On examination, bluish, bulging vessels covered by mucosa may become visible when the patient coughs. Internal haemorrhoids are typically asymptomatic due to their visceral innervation.
Inflammatory bowel disease
Inflammatory bowel disease (IBD) is a general term that is used to describe disorders that involve chronic inflammation of the gastrointestinal tract. Ulcerative colitis and Crohn’s disease are subtypes of IBD and differ in their clinical presentation.
Ulcerative colitis is the most common form of IBD and affects the colon and rectum. Typical findings on rectal examination include loose bloody stool and excess mucous.
Crohn’s disease is another subtype of IBD which can affect any part of the gastrointestinal tract from the mouth to the anus. Typical findings on rectal examination may include rectal bleeding, perianal fistulas, abscesses and multiple skin tags.
Palpation
First steps
1. Lubricate the examining finger.
2. Warn the patient you are about to insert your finger.
3. Insert your finger gently into the anal canal.
Prostate examination
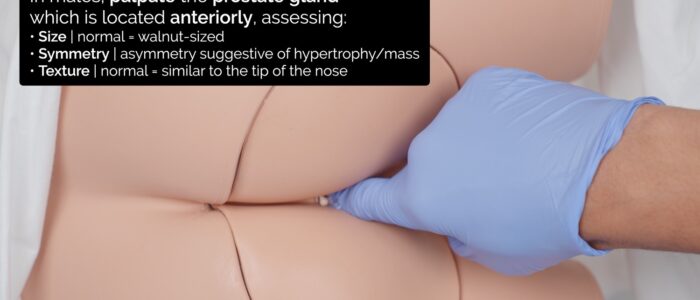
4. In males, palpate the prostate gland anteriorly and assess the size, symmetry and texture of the gland:
- A normal prostate is approximately walnut-sized with a palpable midline sulcus.
- It should be symmetrical and its consistency should be similar to that of the tip of the nose.
Rectal examination
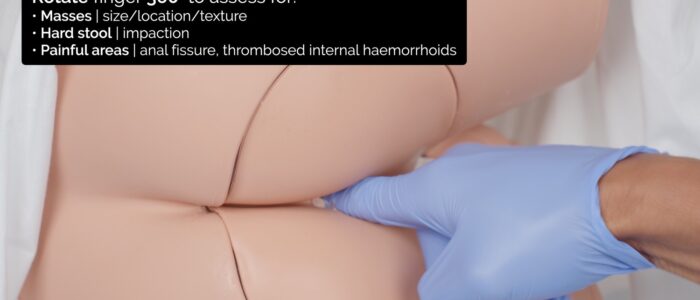
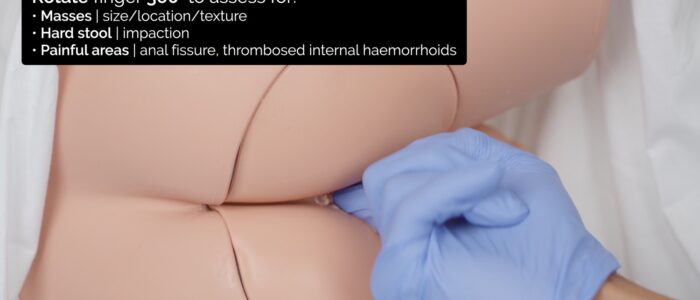
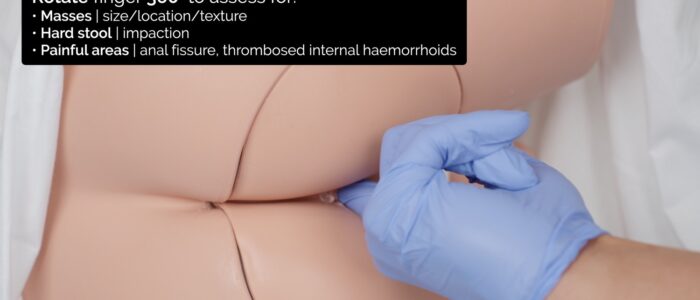
5. Rotate your finger 360 degrees to assess the entire circumference of the rectal wall:
- Note the size, location (e.g. 9 o’clock) and texture (e.g. smooth, irregular) of any rectal lumps (e.g. tumour, polyp, internal haemorrhoid).
- Feel for any hard stool present in the rectum, which may indicate constipation.
- Note the location of any tenderness, which may indicate an anal fissure or thrombosed internal haemorrhoids.
Anal tone assessment
6. Assess anal tone by asking the patient to bear down on your finger. Causes of reduced anal tone include spinal cord pathology (e.g. cauda equina syndrome), inflammatory bowel disease and previous rectal surgery.
Final steps
7. Withdraw your finger and inspect for blood or mucous:
- Dark sticky blood is known as melaena and is associated with upper gastrointestinal bleeding (e.g. peptic ulcer, gastric cancer).
- Fresh red blood is associated with lower gastrointestinal bleeding (e.g. haemorrhoids, anal fissure, angiodysplasia, cancer).
- Excess mucous can be associated with inflammatory bowel disease (e.g. ulcerative colitis) or cancer.
8. Clean the patient using paper towels.
9. Cover the patient with the sheet, explain that the examination is now complete and provide the patient with privacy so they can get dressed.
10. Dispose of the used equipment into a clinical waste bin.
To complete the examination…
Thank the patient for their time.
Dispose of PPE appropriately and wash your hands.
Document the procedure in the medical notes including the details of the chaperone.
Summarise your findings.
Example summary
“Today I examined Mr Smith, a 28-year-old male. On general inspection, the patient appeared comfortable at rest. There were no objects or medical equipment around the bed of relevance.“
“There were no abnormalities noted on inspection of the perianal region, rectal examination revealed a normal-sized prostate and no evidence of hard stool or masses in the rectal canal. No rectal bleeding was noted. “
“In summary, these findings are consistent with a normal rectal examination.”
“For completeness, I would like to perform the following further assessments and investigations.”
Further assessments and investigations
- Abdominal examination: if there were concerns about intraabdominal pathology (e.g. appendicitis).
- Blood tests: including FBC, haematinics and U&Es if there were concerns about gastrointestinal bleeding.
- Faecal immunochemical test (FIT): if there were concerns about lower gastrointestinal malignancy.
- Flexible sigmoidoscopy/colonoscopy: if there were concerns about lower gastrointestinal bleeding or malignancy.
- CT abdomen and pelvis: if there were concerns about lower gastrointestinal malignancy.
Reviewer
Dr Ally Speight
Consultant Gastroenterologist
References
1. Bernardo Gui. Adapted by Geeky Medics. Anal fissure.
2. Απόστολος Σταματιάδης. Adapted by Geeky Medics. External haemorrhoid. Licence: CC BY-SA.
3. WikipedianProlific. Adapted by Geeky Medics. Illustration of haemorrhoids. Licence: CC BY-SA.
4. Internet Archive Book Images. Adapted by Geeky Medics. Anal fistula.