- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Knowing which blood bottles to use for different tests is essential in clinical practice. Knowledge of blood bottles is one of those practical things which is poorly taught, if at all! Even though most hospitals now have printable stickers for bottles that tell you which ones to use, it is still vital to understand which bottles are used and why to prevent mistakes and/or awkward phone calls from the laboratory.
The colours of the vacutainer bottles are standardised. However, depending on which hospital you work in, preferences may vary between individual laboratories, especially regarding tests performed less frequently. It is important to check local guidelines or discuss with the laboratory if you’re not sure.
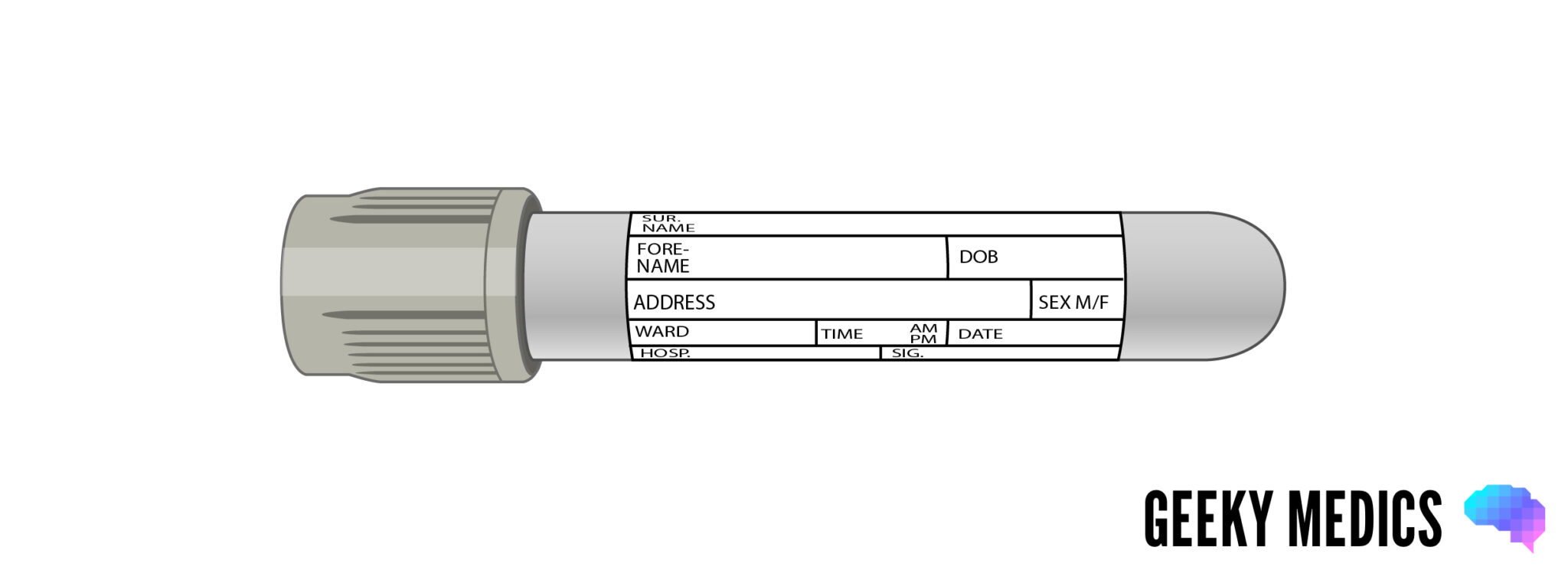
Purple blood bottle (a.k.a. “lavender”)
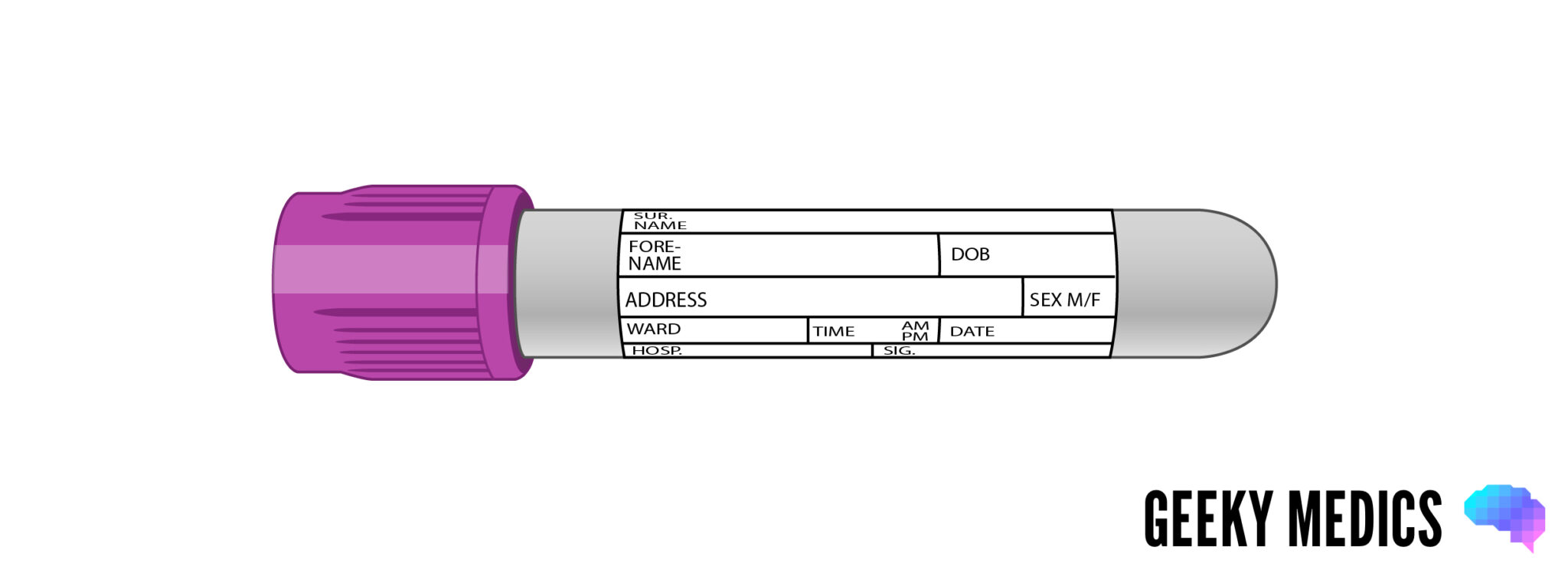
Overview
Purple blood bottles are generally used for haematology tests where whole blood is required for analysis.
Additive
Purple blood bottles contain EDTA (ethylenediaminetetraacetic acid), which acts as a potent anticoagulant by binding to calcium in the blood. EDTA also binds metal ions in the blood and is used in chelation therapy to treat iron, lead or mercury poisoning. Its blood-binding capacity means it can be labelled with radioisotopes and used as an EDTA scan to assess renal glomerular filtration rate.
Tests
Common tests
Common tests performed using the purple blood bottle include:
- Full blood count (FBC)
- Erythrocyte sedimentation rate (ESR)
- Blood film for abnormal cells or malaria parasites
- Reticulocytes
- Red cell folate
- Monospot test for EBV
- HbA1C for diabetic control
- Parathyroid hormone (PTH)*
Less common tests
Less common tests performed using the purple blood bottle include:
- Ciclosporin/tacrolimus levels
- Some viral PCR tests
- G6PD
- ACTH level*
- Porphyria screen*
- Plasma metanephrines*
- Fasting gut hormone screen*
Tips for use
The purple tube needs inverting about 8 times to mix the sample with the EDTA. About 1ml of blood is sufficient to perform a full blood count. However, to get an ESR you will need a full purple bottle.
Pink blood bottle
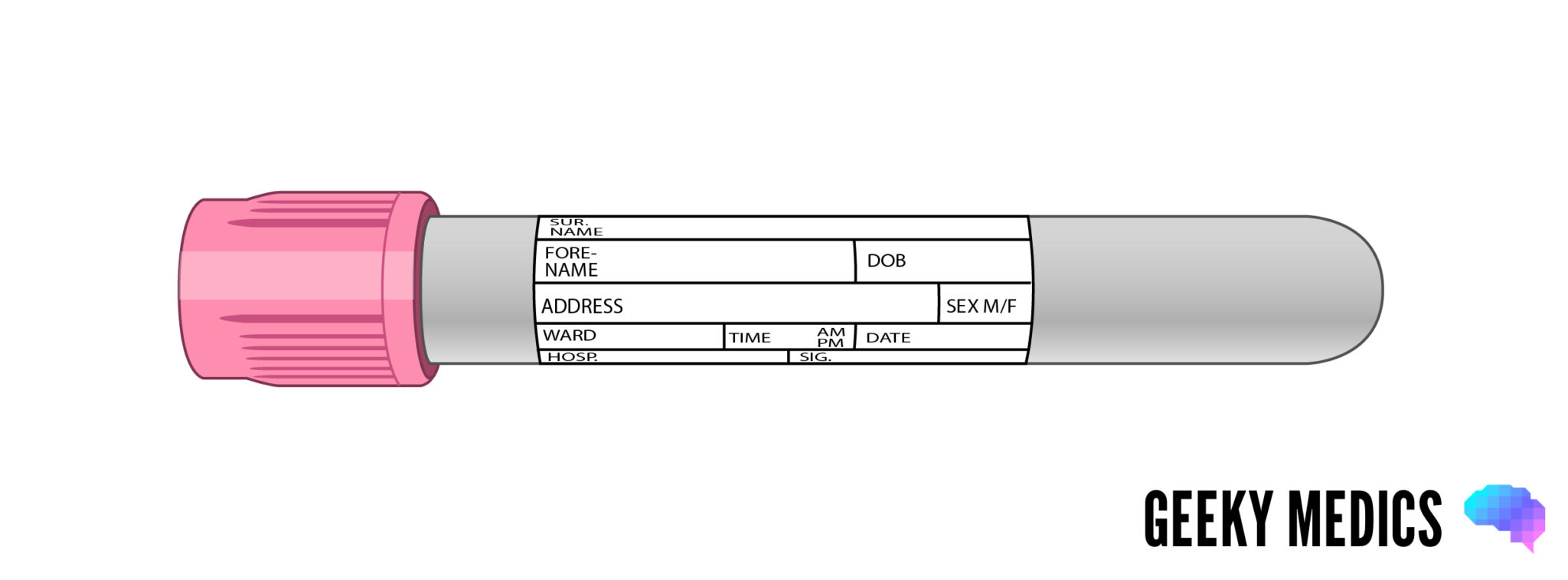
Overview
The pink bottles work in the same way as the purple ones, but are specifically used only for whole blood samples being sent to the transfusion lab.
Additive
Pink blood bottles also contain the anticoagulant EDTA.
Tests
Common tests
Common tests performed using the pink blood bottle include:
- Group and save (G&S): this simply means the patient’s blood is typed and tested for antibodies, then saved in the lab in case it is required; it DOES NOT get you blood products for transfusion. If you need blood products you have to request a crossmatch.
- Crossmatch (XM): this means that the patient’s blood is typed and tested as above, then matched to specific units of blood, platelets or other products for transfusion. You need to specify on the form how many units you need, why you need them and when they are required. A full crossmatch takes about 45-60 minutes in the lab – if you have an unstable bleeding patient and think you’ll need blood products sooner than this, you still need to send a crossmatch sample, but you can ask the lab for units of type-specific blood (which take 10-20 minutes), or in a genuine emergency you can use their stocks of O negative blood from the fridge.
- Direct Coomb’s test (a.k.a. direct antiglobulin test): for autoimmune haemolytic anaemia.
Less common tests
Less common tests performed using the pink blood bottle include:
- Testing for specific red cell antibodies (usually 3 bottles are required).
- Haematology tests such as FBC (if the ward runs out of purple bottles).
Tips for use
The pink tube needs inverting about 8 times to mix the sample with the EDTA. It should contain at least 1ml of blood, but more is preferred by the labs if possible. It has a special label that must be carefully filled in by hand at the bedside to ensure the correct patient details are used, preventing potentially catastrophic mismatched blood transfusions. If you need blood for a patient urgently or have any unusual or complicated requests, you must ring the transfusion lab and let them know.
For more details on performing blood transfusions safely see our OSCE guide.
Blue blood bottle
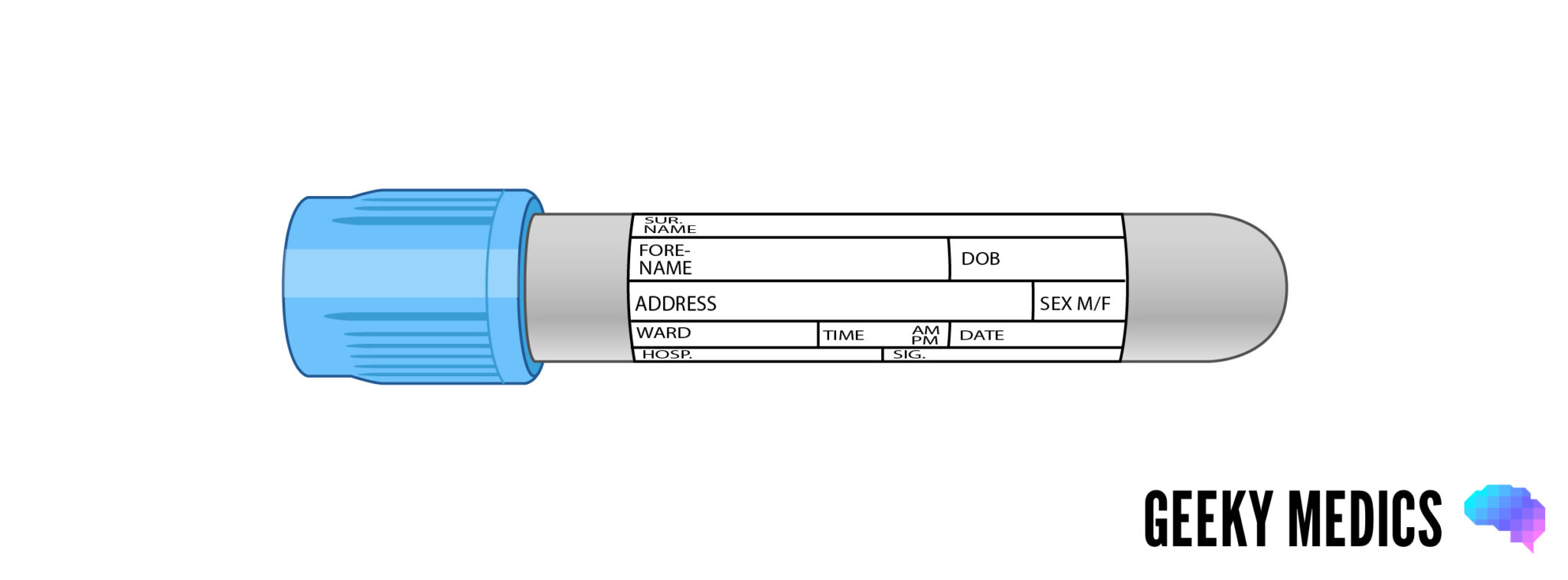
Overview
The blue bottle is used for haematology tests involving the clotting system, which require inactivated whole blood for analysis.
Additive
Blue blood bottles contain buffered sodium citrate, which acts as a reversible anticoagulant by binding to calcium ions in the blood and disrupting the clotting cascade. Sodium citrate is also added to blood products for transfusion and acts as a preservative, stopping them from clotting in the bag.
Tests
Common tests
Common tests performed using the blue blood bottle include:
- Coagulation screen: including bleeding time for platelet function, prothrombin time (PT) for assessment of the extrinsic pathway, activated partial thromboplastin time (APTT) for assessment of the intrinsic pathway, and a thrombin time (TT) or fibrinogen assay for assessment of the final common pathway.
- D-dimer to assist with ruling out thrombosis (e.g. deep vein thrombosis).
- INR for monitoring patients on warfarin (this is calculated from the prothrombin time).
- Activated partial thromboplastin ratio (APTR) for monitoring patients on intravenous heparin infusions (this is calculated from the APTT).
- Anti-Xa assay for monitoring patients on high-dose low molecular weight heparins like tinzaparin.
Less common tests
Less common tests performed using the blue blood bottle include:
- Specific clotting factors (e.g. factor VIII, factor IX, von Willebrand factor)
- Thrombophilia screen
- Lupus anticoagulant
Tips for use
The blue bottle must be inverted 3-4 times to mix the sample with the anticoagulant. The sodium citrate liquid in the bottle dilutes the blood sample, and the machines in the lab are specifically calibrated to interpret results based on a set ratio of blood to anticoagulant. Therefore, the bottle must be filled to the line marked around its edge to ensure the tests are interpreted accurately – otherwise, the samples may be over-anticoagulated.
If your first bottle is light blue and you use a butterfly needle, you will likely need to use two blood bottles to obtain a full sample. This is because attaching the first bottle will draw in air from the tubing, resulting in a sample that cannot fill with enough blood to reach the required level. To avoid this, you can initially attach a light blue blood bottle to remove the air (i.e. fill the tubing with blood), then detach this and fill a second blue blood bottle to the required level.
Some clotting tests must be taken at specific times; INRs should ideally be done in the morning, and anti-Xa assays must be taken 3-4 hours after tinzaparin is given. APTR timings are often indicated on the prescription algorithm.
Yellow blood bottle (a.k.a. gold)

Overview
These bottles are used for a wide range tests requiring separated serum for analysis, including biochemistry, endocrinology, oncology, toxicology, microbiology and immunology.
Additive
This tube is known in the lab as the SST (serum separating tube). It contains two agents; silica particles and a serum separating gel. The silica particles work to activate clotting and cause the blood cells to clump together. The serum separator consists of an inert polymer gel which floats as a layer between the blood cells and plasma to form a physical barrier between them. The sample can be centrifuged (spun) in the lab, and the separated serum easily removed.
Tests
Biochemistry tests
Biochemistry tests are the ones you will encounter most commonly:
- Urea and electrolytes (U&Es): this includes urea, creatinine, sodium and potassium.
- C-reactive protein (CRP)
- Liver function tests(LFTs): this includes bilirubin, ALP, AST/ALT, GGT, total protein and albumin.
- Amylase assay
- Bone profile: this includes calcium, phosphate, ALP and albumin.
- Magnesium assay
- Iron studies: this includes serum iron, ferritin, transferrin saturation and total iron-binding capacity.
- Lipid profile: this includes cholesterol, LDL, HDL and triglycerides.
- Thyroid function tests (TFTs): this includes TSH, free T4 and sometimes free T3.
- Vitamins: including vitamin B12.
- Troponins: this requires 2 samples to be taken at different times to assess the acute trend.
- Creatine kinase (CK)
- Urate
- Serum osmolality: this requires a urine sample to be taken at the same time.
Endocrinology tests
Endocrinology tests that can be performed using a yellow blood bottle include:
- Beta-hCG
- Calcitonin*
- Cortisol
- EPO
- Sex hormones
- Growth hormone
- IGF-1
Tumour marker tests
Tumour marker tests that can be performed using a yellow blood bottle include:
- PSA
- CEA
- CA-125
- CA19-9
- AFP
- Lactate dehydrogenase (LDH)
Toxicology tests
Toxicology tests that can be performed using a yellow blood bottle include:
- Ethanol
- Cannabis
- Opiates
- Benzodiazepines
- Other drugs (e.g. cocaine, amphetamines)
Drug level tests
Drug level tests that can be performed using a yellow blood bottle include:
- Paracetamol
- Salicylates (aspirin)
- Digoxin
- Lithium
- Gentamicin
- Carbamazepine
Microbiology/virology tests
The yellow blood bottle can test for various bacterial, viral, fungal and parasitic infections, including HIV and viral hepatitis.
Immunology tests
Immunology tests that can be performed using a yellow blood bottle include:
- Immunoglobulin levels
- Complement levels
- Autoantibody screen
- Rheumatoid factor
- Thyroid antibodies
- α1AT
- ACE
Tips for use
The yellow bottle must be inverted about 5 times to mix the sample with the silica and separator. Don’t panic if the blood starts to clot or separate in the bottle, it’s supposed to!
The amount of blood required will depend on how many tests you’re doing, but at least 1ml is ideal. You can usually get about 12 tests from one full yellow bottle. Remember that different labs may be located in different areas and technicians don’t like sharing – this means you’ll need to put your biochemistry and microbiology samples in separate yellow bottles to go to their respective laboratories.
Grey blood bottle
Overview
The grey bottle is only used for two tests, so compared to the yellow one, it’s fairly easy to remember! It is used for biochemistry tests requiring whole blood for analysis.
Additive
Contains two main agents. Sodium fluoride acts as an antiglycolytic agent to ensure no further glucose breakdown occurs within the sample after it is taken. Potassium oxalate acts as an anticoagulant. Some variants of the grey bottle use EDTA as the anticoagulant instead.
Tests
Common tests
Common tests performed using the grey blood bottle include:
- Glucose: this can be fasting or non-fasting, or part of a glucose tolerance test (GTT)
- Lactate
Less common tests
Less common tests performed using the grey blood bottle include:
- Blood ethanol (if not for legal purposes)
Tips for use
The grey bottle must be inverted about 8 times to mix the sample with the fluoride and oxalate. Only a tiny amount of blood is required for a glucose test, but to assess lactate levels, the bottle should ideally contain at least 1ml of blood.
Venous glucose results are generally more accurate than finger-prick capillary blood glucose tests, especially in hyperglycaemic patients, but it can take a while to come back from the lab. If you require a blood glucose test urgently, perform a capillary blood glucose.
Samples for venous lactate need to be sent to the lab immediately. Again, the results tend to take a while to come back, so if you need to assess a patient’s lactate level quickly, perform an arterial blood gas as most ABG machines will give a lactate level.
Red blood bottle
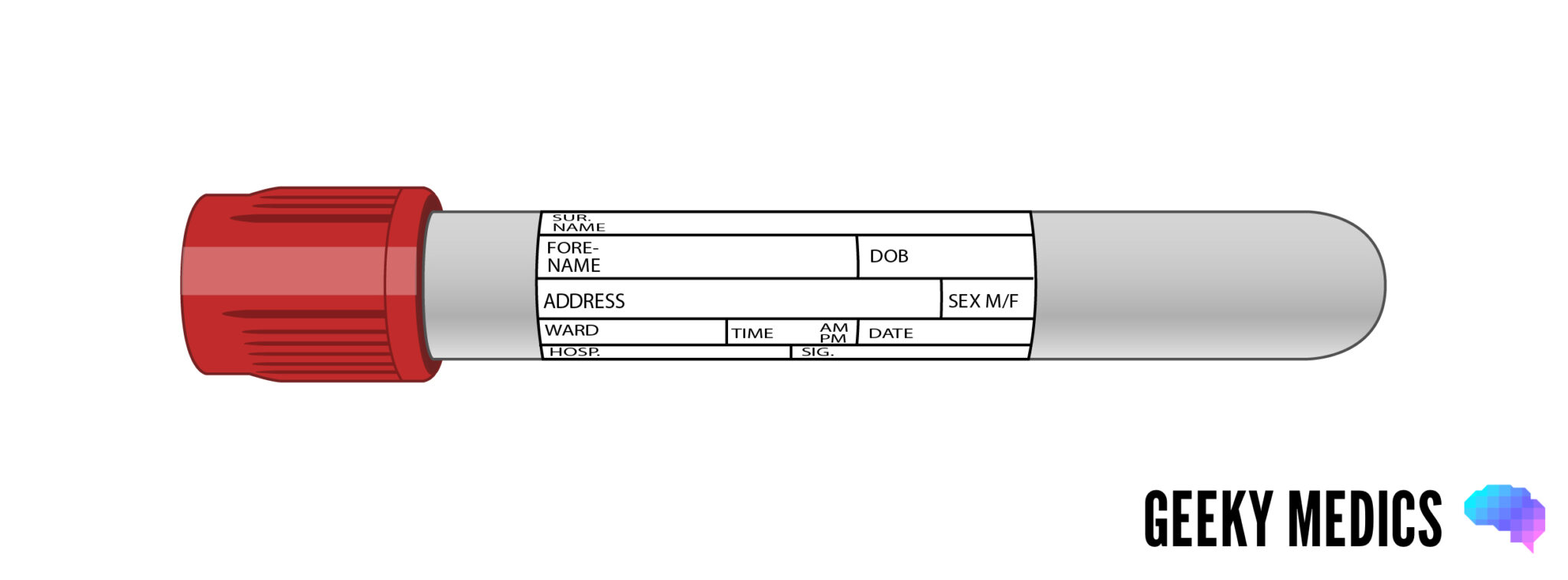
Overview
The red bottle is less common – it is used for biochemistry tests requiring serum which might be adversely affected by the separator gel used in the yellow bottle.
Additive
The additive in red blood bottles contains silica particles which act as clot activators.
Tests
Common tests
The use of this bottle varies greatly. Some hospitals use it for many sensitive tests, including hormones, toxicology, drug levels, bacterial and viral serology and antibodies. In contrast, others only use it for a few very specific purposes (e.g. ionised calcium) and use the yellow bottle for most things.
Less common tests
Less common tests performed using the red blood bottle include:
- Fluoride
- Cryoglobulins
- Cold agglutinins
Tips for use
The red bottle needs inverting 5 times to mix the sample with the clot activator. There is also another version of the red bottle made of glass, which contains no additives.
Dark green blood bottle
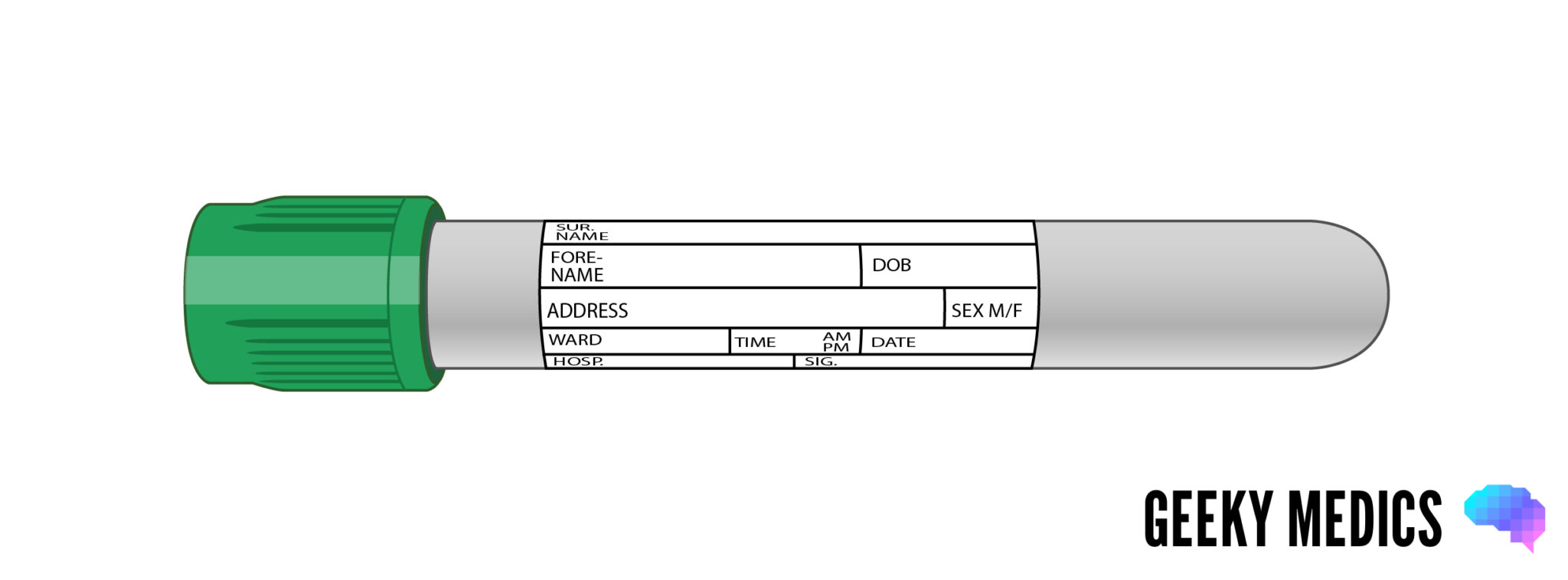
Overview
This less commonly used bottle is for biochemistry tests which require heparinized plasma or whole blood for analysis.
Additive
The additive of dark green blood bottles contains sodium heparin, which acts as an anticoagulant.
Tests
Common tests
Common tests performed using the dark green blood bottle include:
- Ammonia*
- Insulin*
- Renin and aldosterone
Less common tests
Less common tests performed using the dark green blood bottle include:
- Aluminium
- Gut hormones
- Amino acids
- Homocysteine
- Chromosomal tests
Tips for use
The green bottle needs to be inverted about 8 times to mix the sample with the heparin. This bottle cannot be reliably used to assess sodium levels.
Light green blood bottle
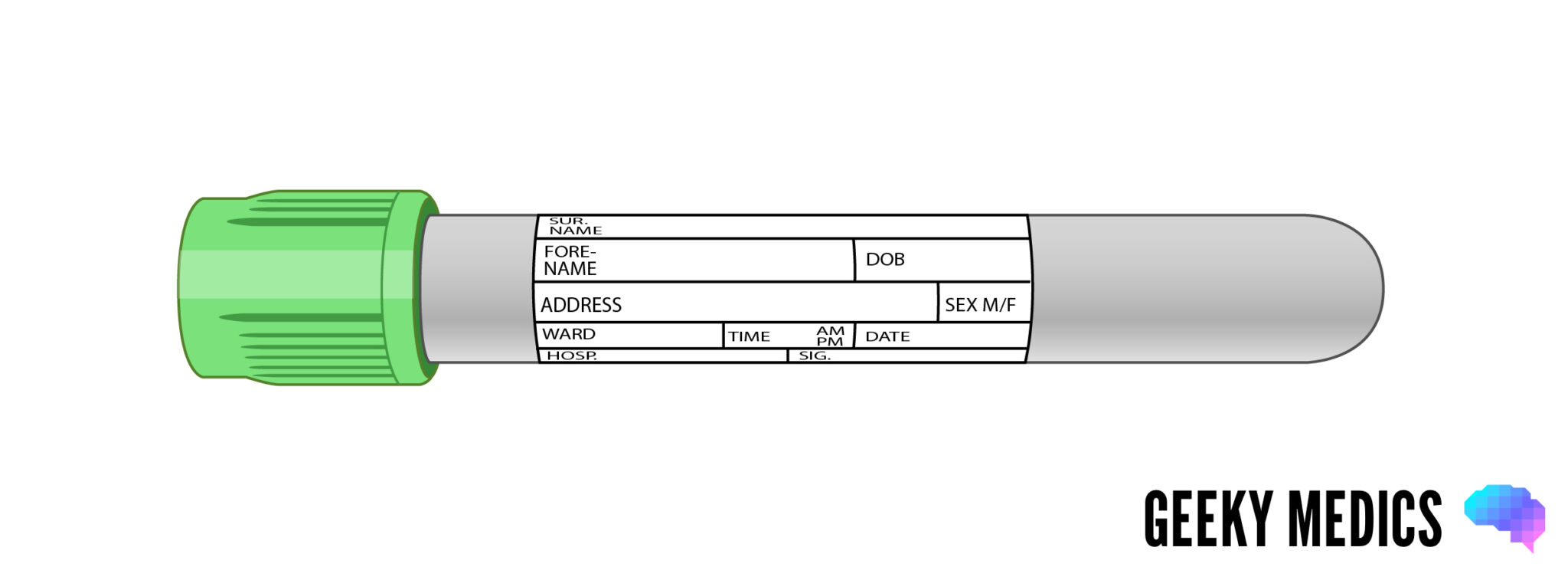
Overview
This rare blood bottle is used for biochemistry tests requiring separated heparinized plasma.
Additive
This bottle is known as the plasma separator tube (PST). It contains lithium heparin, which acts as an anticoagulant, and a plasma separator gel similar to that used in the yellow bottle, which acts to separate the plasma layer.
Tests
It can be used for routine biochemistry, but most hospitals use the yellow bottle. It can also be used for blood ethanol provided the sample is not for legal purposes.
Tips for use
The light green bottle needs inverting about 8 times to mix the sample with the heparin and separator. This bottle cannot be reliably used to assess lithium levels.
Other blood bottles
There is a wide range of other rare blood bottles, which you may occasionally see used in clinical practice. These include:
- Dark blue: used for toxicology and trace elements such as zinc, selenium and copper (however, the ever-versatile yellow bottle can also be used for these).
- Tan: used to test for lead.
- Orange: contains a thrombin-based clot activator which allows stat serum testing.
- Light yellow: used for HLA phenotyping, tissue typing, DNA analysis and paternity testing.
- White: used for molecular diagnostics such as PCR and DNA amplification studies.
- Black: for paediatric ESR.
- Clear lid: used as a discard tube, for example when taking blood from a central line.
Blood culture bottles
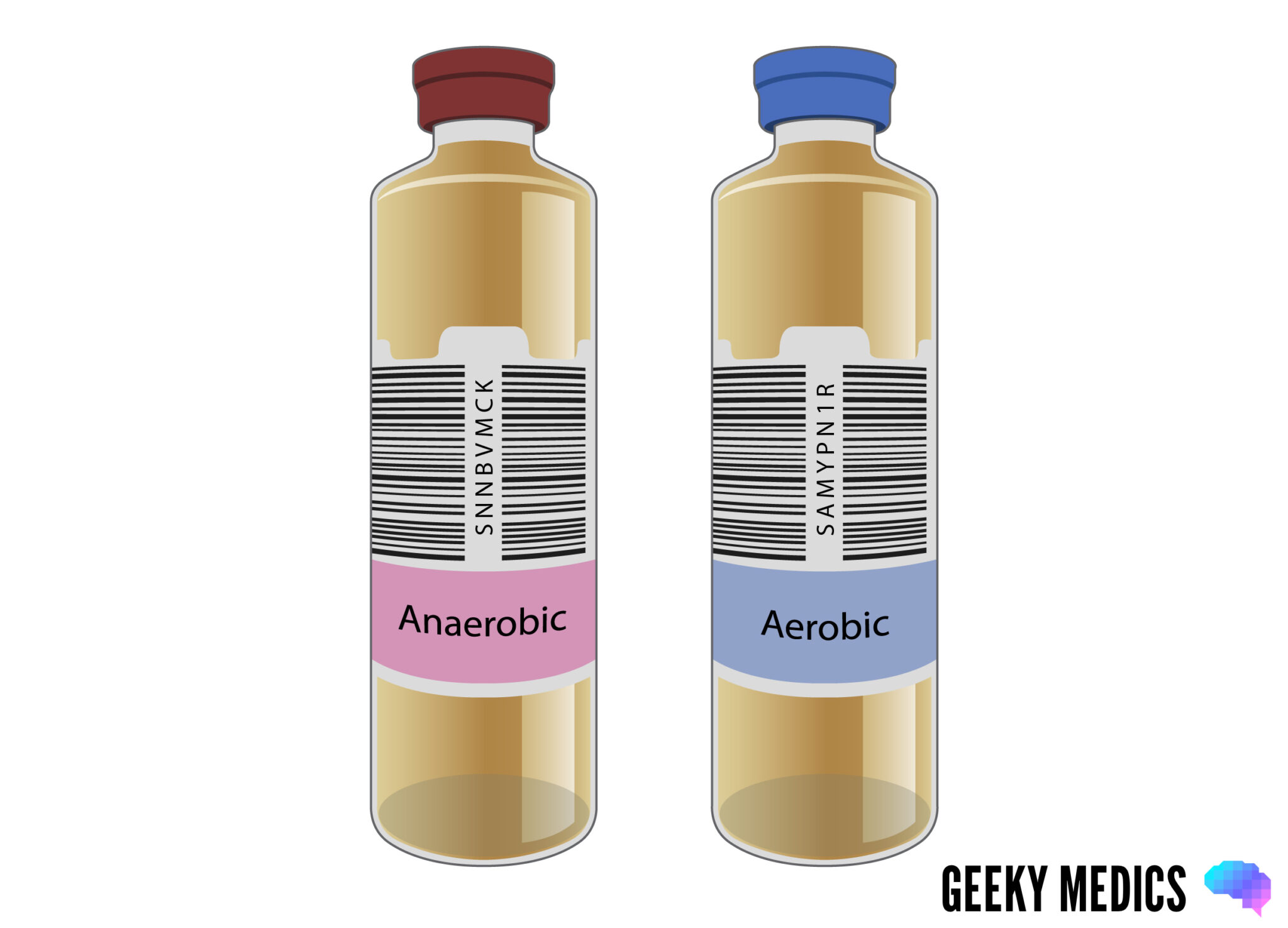
Blood culture bottles contain a culture medium to encourage the growth of any bacteria in the blood sample.
Different bottles are available with culture media for aerobic (blue lid) and anaerobic (purple lid) organisms, alongside a variety of others, including one with a black lid for mycobacterial cultures.
Until recently, many hospitals required both aerobic and anaerobic culture samples from a patient, whilst others were happy with just aerobic samples. However, there is a move towards using the purple top (a.k.a. “burgundy”) anaerobic bottles as the standard receptacle for all blood cultures. Studies have shown that they are more effective. Check local guidelines if you’re not sure.
Tips for use
Blood cultures must be obtained using an aseptic non-touch technique (ANTT) to prevent contamination of the samples with the patient’s skin flora or any bugs lurking on your hands. They should also be taken before any antibiotics are started.
The blood culture bottle should always be the first one you fill, and ideally needs 8-10ml of blood to ensure a good chance of catching any organisms (if using an anaerobic and aerobic bottle, the aerobic bottle should be filled first). In a perfect world, you would also take another culture from a different site to maximise the diagnostic yield. The results take about 5 days to come back, so if your patient is septic, you need to start them on empirical antibiotic treatment whilst awaiting culture results.
For more information on blood cultures, see our OSCE guide to performing blood cultures.
Arterial blood gas syringes
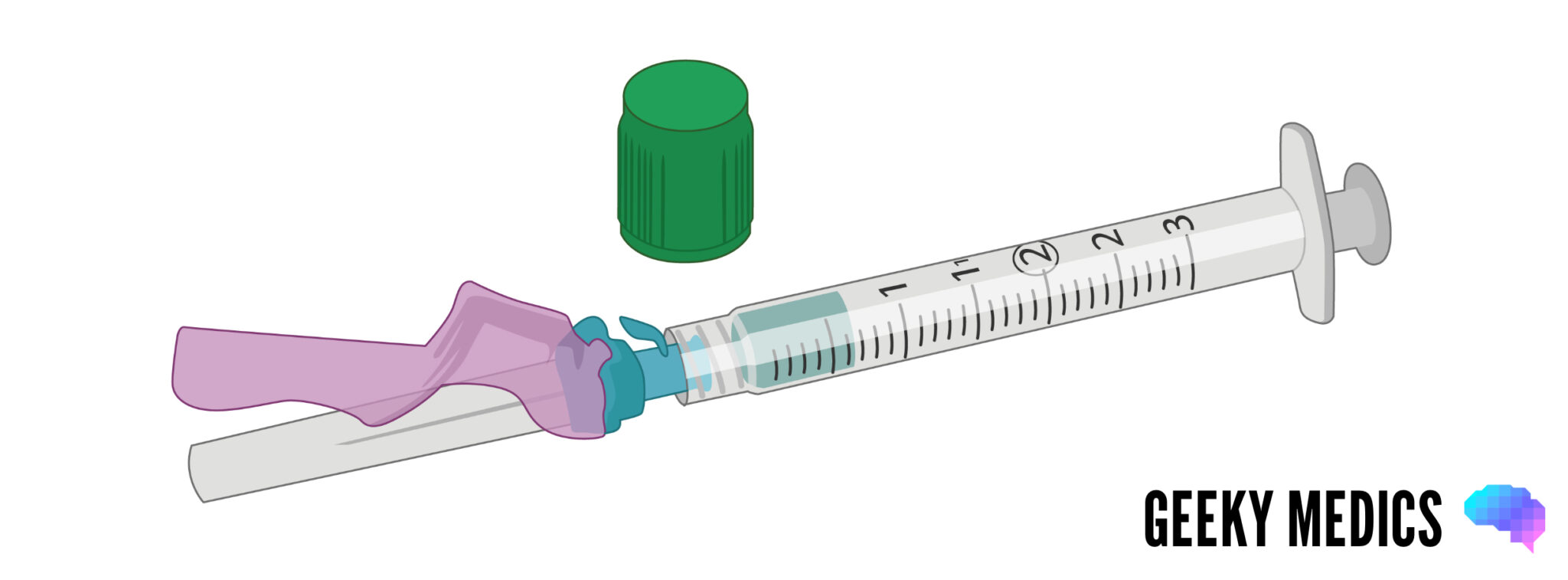
Overview
An arterial blood gas is a very useful test when confronted with a critically unwell patient. It tells you about their oxygenation, their acid-base balance, and in some cases, their potassium and lactate. The results are usually available within minutes.
Tips for use
ABG syringes contain heparin to prevent the sample from clotting – you need to expel this through the needle before taking your sample. Some fill automatically as the plunger is pushed back by the pressure of the blood coming through the needle, whilst others require you to pull on the plunger yourself to fill the syringe. Try to get the self-filling ones – like those shown above – if possible, as they are infinitely better.
Compared to taking a venous blood sample, ABGs are technically more challenging, riskier and much more uncomfortable for the patient. For more details and tips on taking an ABG, see our OSCE guide to performing an ABG.
Once you have obtained your sample, it must be taken straight to the lab, as it will become denatured and useless within 10 minutes. To learn how to interpret an ABG, see our guide to ABG interpretation.
Tips for easy venepuncture
Invert doesn’t mean shake: be gentle with your samples, or they’ll haemolyse.
Tests above with a star (*) next to them need to be sent to the lab immediately on ice – to do this, you either need to get a special ice bag directly from the lab or if your ward has an ice freezer, you can make one yourself by filling a normal sample bag with crushed ice. If you’re not sure you’re doing it right, ring the lab and check before you take the blood sample.
The bottles can be used for other non-blood fluids too, for example, pleural aspirates, ascitic taps and CSF samples obtained by lumbar puncture. Each bottle’s tests are the same: the purple one is for cell count, the yellow one is for electrolytes, albumin and LDH, the grey one is for glucose, and blood culture bottles can be used for fluid cultures. Don’t forget to specify on your request form what kind of fluid is in the bottle and which part of the patient you got it from.
If you ever have to get blood from a child, there are special paediatric blood bottles which are much smaller than the adult ones. The colours vary compared to adult bottles, so always check with the local laboratory. For more information, see our guide to paediatric venepuncture.
If you are unsure what to do for a particular blood test, ask your friendly local lab technician. They are usually more than happy to advise you as it means they can prevent you from making mistakes that create hassle and annoying paperwork.
Blood bottle summary
We have summarised the different types of blood bottles below, organised by order of draw, including the relevant tests and the number of required inversions.
Table 1. Blood bottle summary
| Colour | Tests | Inversions required |
|
Light blue |
|
3-4 |
|
Yellow/gold |
|
5-6 |
|
Purple |
|
8-10 |
|
Pink |
|
8-10 |
|
Grey |
|
8-10 |
References
- BD Vacutainer Product FAQs. Available from: [LINK].
- BD Vacutainer Venous Blood Collection Tube Guide. Available from [LINK].
- UCI Pathology Services Manual. Specimen Tube Containers. Available from: [LINK].