- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Surgeons have been stitching people back together for thousands of years. Ancient civilisations used whatever was available to do the job, including linen, plant fibres, thorns, animal hair, or the jaws of black ants. They soon discovered naturally derived suture materials (e.g. catgut, silk and cotton) which formed the backbone of surgical practice until the 1930s. Over the last century, scientific advances have developed a diverse range of synthetic suture materials.
Whilst nobody should expect you to be an expert on suture materials, it is helpful to understand the options available and the general principles for their use.
This article will describe the different types of suture materials you may encounter in clinical practice, the alternatives to sutures and some clinical scenarios.
What are sutures?
Sutures are medical devices which are used to sew living tissues. They essentially consist of a needle and a thread, known as the suture material. Sutures can hold wound edges together while healing, control bleeding, repair tissue defects or damaged structures, create anastomoses and secure foreign objects such as mesh implants, vascular grafts and drains in place.
Suturing is a core surgical skill and one of the first techniques surgeons are taught during their training. In addition to perfecting the physical art of suturing, surgeons must make important decisions about the best suturing methods to use and which of the vast array of available needles and suture materials to choose for each step of an operation.
Suture needles
Any sort of sewing requires a needle to carry the thread through the tissues. Suture needles are made from stainless steel alloys and have three parts:
- a narrow point which is driven into the tissue
- a wider body which is grasped by the needle holder
- a swage where it joins with the suture material
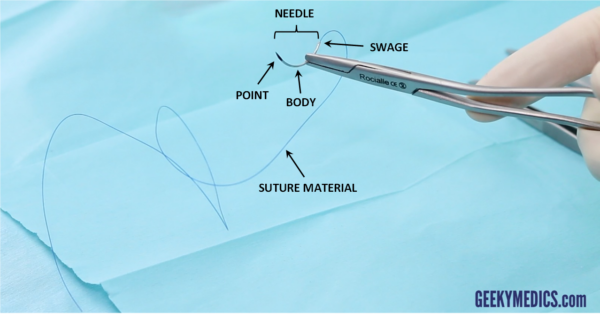
Unlike sewing at home, where you have to push the thread through the eye of the needle yourself, modern suture needles are already seamlessly attached to their suture material to ensure smooth passage through tissues with minimal trauma.
Suture needles come in hundreds of different sizes and shapes. The main considerations when choosing a needle for a particular task are the needle shape and the type of needle tip and point.
Needle shape
The amount of space available in the operative field will dictate the best needle shape to use.
Curved needles
Curved needles are by far the most common type. They can be manoeuvred easily in small spaces and allow the surgeon to take decent bites of tissue by turning their wrist.
Smaller curves (such as ⅜ or ½ of a circle) are suitable for most tasks, whilst larger curves (such as ⅝) are better for very narrow or deep spaces. J-shaped needles are perfect for fascial closure of small laparoscopic port sites. Ski-shaped needles are very useful for laparoscopic suturing, where the surgeon cannot use their wrist to drive a curved needle as effectively.
Straight needles
Straight needles can be held with a needle holder or in the surgeon’s hand. They are very precise and create beautifully neat skin closures. However, they are unsuitable for deeper suturing within body cavities as they require a lot of space to manoeuvre and are more likely to inadvertently prick organs.

Needle tip
The tissue being sutured will dictate the type of needle tip and point required.
Sharp needles
Sharp needles have a sharpened tip which punctures tissue to pass through it. Most suture needles are sharp, as blunt needles are less precise and often struggle to get through tough tissues.
Blunt needles
Blunt needles have a rounded tip which dilates and separates tissue to pass through it. These have the advantage of improved safety for theatre staff, as they are much less likely to puncture gloves and have been shown to significantly reduce needlestick injuries.
Blunt needles are used for abdominal wall closure as they also reduce the risk of accidentally stabbing the bowel. However, it takes more force to pierce tissue with a blunt needle than with a sharp one, so each bite must still be as careful and controlled as possible.
Needle point
Cutting needles
Cutting needles have a sharpened point which cuts a path through tissues. This looks like a triangle in cross-section. The inner concave edge cuts through the tissue towards the surface, whilst the outer surface is flat. Cutting needles are useful for passing through tough tissues, such as thick skin, fascia and the sternum. However, they can weaken other tissues, causing sutures to cut out into the wound.
Reverse cutting needles
Reverse cutting needles also have a sharpened point, but this time the inner surface is flat, whilst the outer convex edge cuts through tissue away from the surface. This looks like an upside-down triangle in cross-section. Reverse cutting needles are useful in tissues with a risk of the suture cutting out and causing additional damage, such as thinner skin, tendons, ligaments, oral mucosa and the eye.
Side cutting (spatula) needles
Side cutting or spatula needles have a trapezoid shape with cutting edges on both sides, which allows them to safely create a path within thin layers of tissue. These are very useful for eye surgery.
Round bodied needles
Round bodied needles have a smooth, tapering point which dilates tissue. This looks like a circle in cross-section. Round-bodied needles may taper into a blunt point, a sharp point (taperpoint needles) or a cutting point (tapercut needles).
Blunt round-bodied needles are ideal for suturing friable tissues such as an injured liver or spleen. Taperpoint needles are useful in potentially leaky tissues which require precise suturing with minimal trauma, such as bowel, bile ducts, blood vessels and myocardium. Tapercut needles are useful in harder tissues and especially valuable in vascular surgery, as the needle point can easily puncture through calcified atherosclerotic tissue without cutting it any further.
Suture materials
Whilst the needle undoubtedly plays a vital role in delivering the thread into the tissues with minimal collateral damage, the suture material is even more important as it remains inside the patient and holds structures correctly.
Optimal wound healing depends upon the direct approximation of healthy tissue edges with minimal tension, no contamination or infection, a good blood supply, and adequate nutrition. Numerous technical factors may compromise wound healing after surgery, including the suturing method, the quality of the surgeon’s suturing technique and their choice of suture materials.
The ideal suture material is cheap, strong, behaves predictably in the body, generates minimal friction, is easy to handle, ties secure knots, causes little or no inflammatory response and resists infection.
Alas, this mythical perfect suture does not exist. Instead, surgeons must choose from various materials designed to perform more effectively in certain situations, each with flaws.
Suture materials are classified by two main characteristics: absorbability and structure. They can also be further classified according to whether they are naturally derived or synthetic in origin, although nowadays, most suture materials are synthetic.
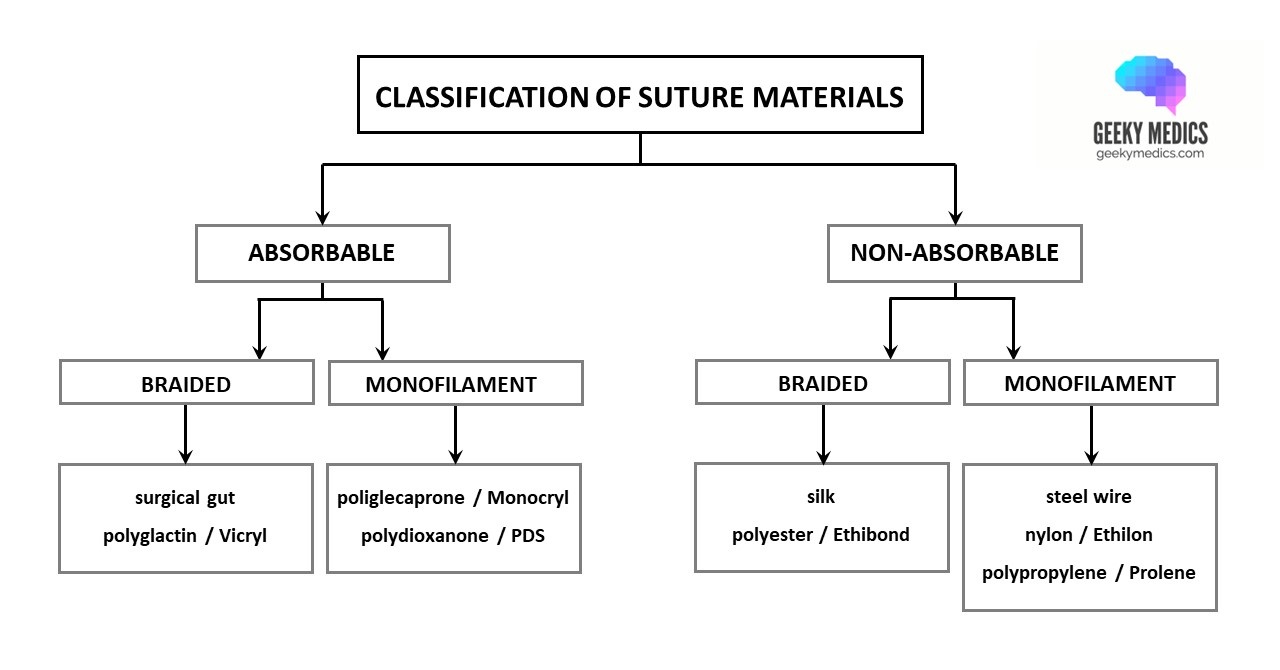
Absorbable vs non-absorbable
Absorbable suture materials maintain their strength while initial tissue healing occurs and then break down completely afterwards. This is good, as it means there is no residual foreign material left inside the patient, although the absorption process inevitably causes some local tissue reactivity.
A suture material is absorbable if it loses significant tensile strength within the first 60 days. Different materials lose strength at different rates and break down over variable periods depending on the type of tissue they were designed to repair. Modern synthetic materials break down more consistently and predictably than those made from natural proteins.
Non-absorbable suture materials maintain their strength over long periods of time. Some lose strength and break down eventually, whilst others remain in the body forever. This is helpful for tissues requiring long-term support, such as fascia and tendons, and things which literally cannot heal, such as prosthetic heart valves and vascular grafts. Synthetic non-absorbable materials are also frequently used as removable skin sutures due to their very low tissue reactivity.
Braided vs monofilament
Braided (or multifilament) suture materials consist of several strands which are twisted together. Braided materials are generally stronger than monofilaments. They are supple and pliable, making them very easy to handle and tie down into secure knots. They are also softer and more comfortable for patients.
However, they also generate high friction and drag as they pass through the tissues, resulting in additional trauma. The gaps between strands represent ideal places for bacteria to hide, and some braided materials also soak up fluid (capillarity) which further increases the risk of infection. In addition, all natural suture materials are braided. These consist of foreign proteins which trigger an immune response resulting in greater tissue reactivity, impaired wound healing and increased scarring.
Monofilament suture materials consist of a single filament or strand. They generate very low friction and pass smoothly through tissues, resulting in minimal trauma. They cause little tissue reactivity and have flat waterproof surfaces which resist infection. They also have greater elasticity and plasticity than braided sutures, allowing them to stretch to accommodate tissue swelling after surgery.
However, they are also more difficult to handle as they are less pliable, have slippery surfaces and possess memory which makes them want to spring back into the position they held inside their packaging. They also tie less secure knots, which can bounce back or unravel after being tied down. As a result, knots tied with monofilament sutures require 5-7 throws, compared with the 3 throws used for most braided sutures. Monofilament sutures are also easily damaged by instruments such as needle holders and forceps. Their firmer, sharper edges may cut through friable tissues or cause discomfort.
Suture sizes
The tensile strength of a suture material (its ability to withstand being pulled apart at either end without breaking) is directly proportional to its diameter. However, it is important to use the smallest possible size for a particular task to minimise tissue damage, inflammation and patient discomfort. The system for describing suture sizes can seem a bit confusing at first.
Historically, suture materials were available in sizes 1-7, with 1 being 0.4mm in diameter and 7 being 0.9mm. These were thick and heavy by today’s standards. Then, a slightly thinner 0.35mm suture was designed, pragmatically designated size 0.
As newer, finer materials were developed, more zeroes were added to indicate smaller diameters, resulting in sizes 2-0 (or “00”) to 5-0 (or “00000”) and eventually the vanishingly tiny 12-0 (you get the picture). For some reason, many manufacturers and surgeons eschew the hyphens and write suture sizes as 2/0 or 5/0 instead.
The main thing you need to remember is that more zeroes mean a finer suture material.
Types of suture materials
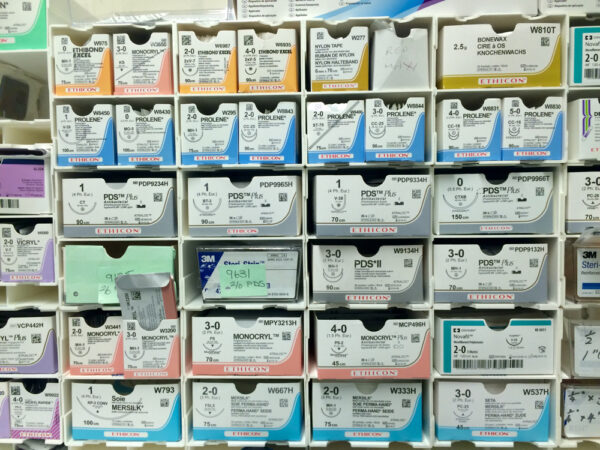
The next section will describe commonly used suture materials in more detail. These have been listed using their chemical name and their best-known proprietary name, as surgeons generally use brand names when referring to suture materials in theatre. Silk and steel wire are exceptions to this.
Most suture materials used in the NHS are manufactured by Ethicon, although alternatives with different brand names are increasingly being introduced to reduce costs.
Specific suture materials (e.g. “a double-ended 5/0 Prolene on a taperpoint needle”) are sometimes requested using their unique product code, as this reduces the risk of staff accidentally opening the wrong type of suture and wasting it.
Collagen/gut
Surgical gut (also known as catgut) is an absorbable braided suture material from natural collagen fibres obtained from sheep and cow intestines. It comes in three colours: yellow, brown and blue. Although it is braided, the fibres are tiny, so it looks and feels like a monofilament suture with a matte surface.

There are three types of catgut sutures:
- Plain gut is simply collagen treated with a glycerol solution. It has a wet consistency.
- Chromic gut is also treated with a chromium salt solution which inhibits proteolytic enzymes, resulting in longer absorption times and reduced tissue reactivity. It has a dry consistency.
- Fast-absorbing gut is heat-treated to speed up its disintegration and absorption.
Absorption time
Gut is broken down by proteolytic enzymes. Plain gut maintains its tensile strength for about 7-10 days, chromic gut maintains its tensile strength for 10-14 days, and fast-absorbing gut maintains its tensile strength for 5-7 days. Gut sutures are completely absorbed within 70-90 days.
Advantages and disadvantages
Gut is a good suture material. It is low friction (unlike other braided sutures), handles well, ties secure knots and has excellent baseline tensile strength.
However, gut absorbs rapidly and should not be used on tissues which require ongoing support or are at risk of prolonged healing. It also does not break down predictably after implantation, and the exact timings can vary considerably depending on individual patient factors. For example, gut absorbs more rapidly in the presence of infection and catabolic states such as trauma, sepsis, cancer or malnutrition. As it is a natural suture material, it triggers a moderate inflammatory reaction, especially if chromic gut is used. This may impair wound healing and can be painful for patients.
Uses
Gut was the suture material of choice for almost 2000 years – it was first documented by Galen, who used it to repair gladiators’ tendons back in 150 AD. However, it has now been superseded by synthetic alternatives and has been banned for human use in Europe and Japan due to concerns about the risk of bovine spongiform encephalopathy (BSE).
Nonetheless, gut is still used in many countries due to its low cost. It has many applications, including the closure of skin and oral mucosa, tonsillectomy, perineal repair and ligation of blood vessels.
Polyglactin (Vicryl)
Vicryl is an absorbable braided suture material made from polyglactin 910. It looks and feels like a fine cotton thread you might use for sewing at home. Vicryl comes in two colours: dyed (purple) and undyed (white). Dyed Vicryl is helpful for deeper tissues as it is much easier to see and follow. However, it is important not to use dyed materials on the skin as they can cause a tattooing effect.

There are three types of Vicryl sutures:
- Standard Vicryl is coated with polyglactin 370 and calcium stearate. This reduces bacterial adherence, improves handling and knot tying and allows the suture to pass through tissues smoothly without snagging.
- Vicryl Plus is also coated with the antiseptic triclosan. This suture material is very popular as it has been shown to significantly reduce surgical site infections.
- Vicryl Rapide is also made from coated polyglactin but has a lower molecular weight. This reduces its tensile strength but allows it to be absorbed more quickly than standard Vicryl. This is useful for simple interrupted skin sutures, which can be left to fall out on their own after a week or so.
Absorption time
Vicryl is absorbed by hydrolysis. Standard Vicryl and Vicryl Plus lose 50% of their tensile strength within 3 weeks and are completely absorbed within 70 days. Vicryl Rapide loses 50% of its tensile strength within 5 days and is completely absorbed within about 40 days.
Advantages and disadvantages
Vicryl is a relatively low friction suture which is non-traumatic to tissues, easy to handle and ties secure knots. It also causes minimal tissue reactivity and is soft and more comfortable for patients.
However, Vicryl can cause inflammation if it remains present in the skin for longer than 7 days. This can lead to the formation of scar tissue, nodules or stitch sinuses in sites where sutures are retained.
Uses
Vicryl is widely used for skin and soft tissue closure and suture ligation of blood vessels. Its softness makes it a good choice for wounds in awkward skin creases or sensitive areas (such as the perineum). It can also be used in abdominal surgery to repair holes in the gastrointestinal tract or bladder, create a hand-sewn intestinal anastomosis or secure a stoma to the skin.
Vicryl should not be used on cardiac, vascular or nerve tissue.
Standard dyed Vicryl is available as individual ties (measured lengths of suture material without a needle attached) or in long reels. These are used to tie off blood vessels during tissue dissection.
Other brand names for polyglactin sutures include Novosyn, Demecryl, Petcryl and Unisynth.
Poliglecaprone (Monocryl)
Monocryl is an absorbable monofilament suture material made from poliglecaprone 25 with a lubricant coating. Like Vicryl, it comes in two colours: undyed (clear) and dyed (purple) and is available as a Plus version coated with the antiseptic triclosan. Unlike Vicryl, it looks and feels like smooth plastic.
Absorption time
Monocryl is absorbed by hydrolysis. It loses 50% of its tensile strength within about 1 week and is completely absorbed within 120 days. Interestingly, the tensile strength of dyed Monocryl lasts slightly longer than the undyed one.
Advantages and disadvantages
Monocryl is an exceptionally smooth and atraumatic suture material. It has excellent tensile strength yet reabsorbs quickly. It also causes virtually zero tissue reactivity which may lead to decreased scar formation and better cosmetic results.
Monocryl is much easier to handle than other types of monofilament suture materials. However, due to its bouncy, plasticky nature, it still tends to have some memory which makes tying knots more difficult. It is also quite hard and sharp and takes longer to reabsorb than Vicryl. This may lead to problems with patient discomfort, particularly around knots and cut suture ends.
Uses
Monocryl is widely used for soft tissue approximation and subcuticular closure of skin incisions. It is a good choice for facial incisions due to the reduced risk of scarring compared to Vicryl.
Monocryl should not be used on cardiac, vascular, nerve or eye tissue and is unsuitable for microsurgical procedures. It may also be better to avoid Monocryl in patients with very thin or fragile skin to avoid any hard knots poking through.
Other brand names for poliglecaprone sutures include Demecaprone, Advantime, Petcryl Mono and Uniglyde Mono.
Polydioxanone (PDS)
PDS (officially known as PDS II) is an absorbable monofilament suture material made from uncoated polydioxanone. It comes in two colours: purple and clear. It looks and feels like smooth plastic.
Absorption time
PDS is absorbed slowly by hydrolysis. It loses 50% of its tensile strength within 4 weeks but hardly breaks down during the first 90 days. It is completely absorbed within about 180 days.
Pros and cons
PDS is smooth and very strong. It provides a much longer period of wound support than other absorbable sutures and only causes a mild tissue reaction. It can also maintain its strength in the presence of infection or exposure to harsh substances such as urine, bile and pancreatic juice.
However, PDS has a lot of memory and can be difficult to handle and snug down into secure knots. Compared to Vicryl, it is quite sharp and can sometimes cut out or “cheese-wire” through tissues if pulled or tightened too hard.
Uses
PDS is commonly used for deep soft tissue closures involving fascial layers or other strong connective tissue, such as closing the linea alba of the abdominal wall after a midline laparotomy. It can also be used to close hernia defects, repair holes in the bowel or create an intestinal or ureteric anastomosis.
PDS should not be used on cardiac, vascular or nerve tissue. It is currently being tested in microsurgical procedures. Vicryl may be preferable if the tissues are very inflamed and friable, for example during an appendicectomy or repair of a perforated duodenal ulcer, due to the risk of cheese-wiring with PDS.
Other brand names for polydioxanone sutures include MonoPlus, Demediox, Monotime, Duracryl and Unisynth PDS.
Silk
Silk is a non-absorbable braided suture material made from natural fibroin filaments obtained from cocoons spun by silkworm caterpillars. This is typically coated with wax or silicone. Silk is usually black, but the colours vary depending on the brand. It looks like cotton thread but is coarser in texture than Vicryl. It often comes attached to an overly large curved needle.

Behaviour over time
As its proteins naturally break down, silk gradually loses its tensile strength over about 1 year. It becomes encapsulated by fibrous scar tissue and eventually disappears after about 2 years.
Advantages and disadvantages
Silk has the best handling of any suture material and ties the most secure knots. It is also softer and more comfortable than monofilament sutures.
However, whilst silk is strong, it has the lowest tensile strength of all suture materials. In addition, silk generates more friction than other suture materials and is rougher on the tissues. It is made from foreign proteins, which may provoke a significant inflammatory reaction, impairing healing and making removal painful. It also has high capillarity and creates a nidus for wound infections.
Uses
Like catgut, silk has been used for millennia but has now been eclipsed by newer synthetic suture materials with better tensile strength, reduced tissue reactivity and lower risk of infection.
In modern practice, silk is virtually never used as a permanent internal suture, as this is akin to leaving a retained foreign body inside the patient. It is primarily used in dental procedures and for securing drains or central lines. It can also be used as a stay suture to lift or retract structures intraoperatively, or for temporary skin closure (e.g. following a fasciotomy or a trauma laparotomy).
Cotton and linen sutures are also available, but are not frequently used in clinical practice.
Polyester (Ethibond)
Ethibond is a non-absorbable braided suture material made from polyester (also known as polyethylene terephthalate) with a lubricant coating. It looks and feels like a very thin shoelace. It comes in two colours: green and white.
Behaviour over time
Ethibond does not break down and lasts indefinitely, becoming gradually encapsulated by scar tissue.
Advantages and disadvantages
Ethibond is soft, exceptionally strong, easy to handle and ties secure knots. It causes minimal tissue reactivity.
However, despite its lubricant coating, it still exerts more friction on tissues than monofilament sutures. It is also expensive.
Uses
Ethibond is highly versatile. It can be used to reapproximate the ribs during the closure of thoracotomy incisions and to close a median sternotomy alongside or instead of steel wire. It is used in cardiac surgery to secure prosthetic heart valves in place. It may be used during orthopaedic surgery as an anchoring suture, to repair tendons and to close deep fascial layers. It is used in general surgery to repair hiatus hernias and diaphragmatic injuries. Colorectal surgeons also use it as a drainage seton to treat anal fistulas.
Other brand names for polyester sutures include Mersilene, Surgidac, Ti-Cron, Tevdek, PremiCron, Demebond, Cardioxyl, Cardioflon, Procare and Unibond.
Steel wire
Steel wire is a non-absorbable monofilament suture material made from a low-carbon 316L stainless steel alloy with added molybdenum to resist corrosion. It is also available in a less commonly used braided form.
Behaviour over time
Steel wire does not lose strength over time and remains in place indefinitely. It does not adhere to any surrounding structures and is gradually encapsulated by fibrous scar tissue.
Advantages and disadvantages
Steel wire has exceptional tensile strength (it is by far the strongest suture material) and provides long-lasting security as it does not break down. It is resistant to infection and biologically inert, causing virtually zero tissue reactivity in most patients, although some may have reactions to the nickel in the alloy.
However, steel wire is difficult to handle if you aren’t used to it, as it kinks easily and can be weakened by incorrect surgical technique. The heavy steel wire cannot be tied in knots, the ends are twisted together instead. Performing this correctly and securely requires expertise, especially when approximating bones and strong connective tissue. Importantly, steel wires can also be very sharp and pose a risk of cutting through tissues or causing needlestick injuries to theatre staff.
Uses
Heavy steel wire is frequently used to close the sternum following a median sternotomy, these sutures are easily visible on chest X-rays. It is also often used in orthopaedics for cerclage fixation of fractures and large tendon repairs.
Fine steel wire can be used during a specialised inguinal hernia repair known as a Shouldice repair. This is a purely suture-based technique which does not involve any mesh and has excellent results. It is an unusual operation, as the only way to become accredited to perform the procedure is to spend several months intensively perfecting it at the Shouldice Hospital in Canada.
Nylon (Ethilon)
Ethilon is a non-absorbable monofilament suture material made from nylon 6 (also known as polyamide). It comes in three colours: black, green and clear. It looks like plastic and feels stiffer than Monocryl or PDS.
Behaviour over time
Ethilon breaks down very slowly by hydrolysis, losing tensile strength at a rate of 15-20% per year. Like most non-absorbable suture materials, it becomes gradually surrounded by fibrous scar tissue.
Advantages and disadvantages
Ethilon is very strong, has very low friction and causes minimal tissue reactivity. It is also cheap.
However, it has a lot of memory which often results in suboptimal handling and reduced knot security. This can be improved by wetting the suture material, which makes it more pliable and easier to use.
Uses
Ethilon is often used for interrupted closure of skin incisions or traumatic wounds. These sutures need to be removed after 4-14 days, depending on their location. Most are removed after 7-10 days. Ethilon is used in general surgery to close hernia defects and reinforce abdominal wall closures. Very fine Ethilon sutures are used in ophthalmology and microsurgical procedures such as nerve repairs.
As it breaks down over time, Ethilon cannot be used on tissues requiring permanent support from the suture line, such as vascular anastomoses and grafts.
Other brand names for nylon sutures include Nurolon, Dermalon, Surgilon, Monosof, Supramid, Dafilon, Demelon, Linex and Unilon.
Polypropylene (Prolene)
Prolene is a non-absorbable monofilament suture material made from polypropylene. It looks and feels like springy plastic. It comes in two colours: blue and clear. It often comes with a needle at both ends.
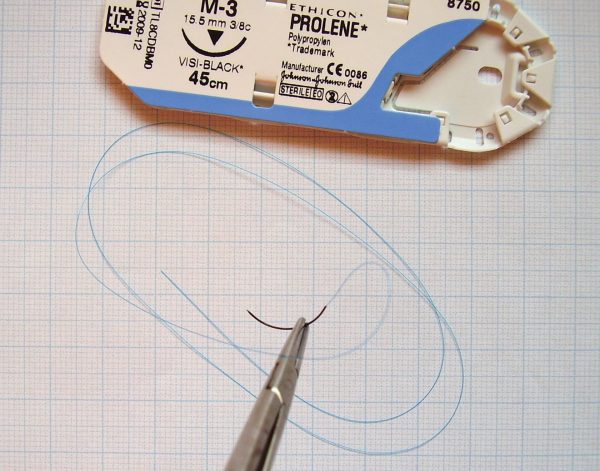
Behaviour over time
Prolene does not break down and lasts indefinitely. It does not adhere to surrounding tissues and can therefore be removed easily.
Advantages and disadvantages
Prolene is strong, has extremely low friction and is permanent, making it ideal for suturing delicate structures like blood vessels. It is biologically inert, resulting in minimal tissue reactivity or scarring, and highly resistant to infection.
However, of all monofilament suture materials, Prolene is probably the most difficult to handle and requires some prior suturing experience before using it for the first time. It is bouncy and slippery, it has considerable memory, and it also has limited elasticity, meaning that can be difficult to throw knots and to snug them down securely without snapping or stretching the thread. It is also expensive.
Uses
Prolene is the suture of choice for cardiac surgery and vascular anastomoses, including microsurgical procedures. It is also used as a removable interrupted skin suture, especially on cosmetically sensitive areas such as the face.
In obstetrics, clear Prolene can be used as a removable subcuticular skin suture after a Caesarean section – no knots are tied, so the whole suture line can simply be pulled out later. In general surgery, it is often used during hernia repairs to close fascial defects or secure mesh.
Other brand names for polypropylene sutures include Surgipro, Premilene, Optilene, Demelene, Corolene, Duracare and Unilene.
Other suture materials
There are many other suture materials on the market, but it would take a long time to cover them all in detail, and most of them have similar characteristics to the ones we have already described.
If you are interested in learning about other suture materials, additional resources can be found in the references at the bottom of this article.
Alternatives to sutures
Alternative methods of wound closure include skin staples, skin glue and steri-strips.
Skin staples
Skin staples (or clips) are made from stainless steel. They can close various traumatic wounds and are particularly useful for scalp lacerations. They are also frequently used to close surgical incisions in situations where subcuticular suturing is not appropriate.
Staples are preferred in heavily contaminated cases (such as faecal peritonitis) which have a high risk of post-operative wound infection. If this occurs, a few staples can be removed on the ward to drain any pus without compromising the rest of the skin closure. Staples are also easy to use and are the fastest option for critically unwell patients who need to get off the operating table and go to the ICU.
However, staples are more uncomfortable than sutures, and their removal is often painful. They leave staple marks on the skin, and applying them quickly may lead to poor tissue approximation with inverted or wonky wound edges. In large wounds, stapling is also more expensive than suturing.
Skin glue
Skin glue is a fast-acting adhesive liquid made from cyanoacrylate (also known as ‘super glue‘). Common brands include Dermabond and Liquiband. Glue can be used as a primary skin closure technique for small linear wounds and an effective dressing. It is safe, strong, atraumatic and seals the wound with a waterproof coating which flakes off on its own after 5-10 days.
This has many advantages, including reduced risk of post-operative infection, improved cosmetic results, constant visibility of the wound, allowing the patient to shower easily and eliminating the need for any dressing changes. It is also a fantastic option for small children.
Using glue for primary closure is a bit fiddly, and it takes practice to get it right. It does not work on wet surfaces, so you must ensure all bleeding is controlled and the wound is completely dry before you start. It requires healthy skin edges under minimal tension, which may necessitate some deep dermal or subcuticular sutures.
Glue takes a couple of minutes to reach maximum bonding strength, so you need to hold the wound edges together until it kicks in. If you aren’t careful, you can end up sticking yourself or your instruments to the patient. It is also crucial to let it dry completely before putting the patient’s gown back on!
Steri-strips
Steri-strips are strips of porous surgical tape with an acrylate adhesive. They come in a range of sizes. They can be used as a primary skin closure method for small linear wounds, or as extra support for larger wound closures. Like skin glue, they are safe, atraumatic, child-friendly and provide an additional layer of protection against infection. They usually fall off within 2 weeks.
Steri-strips are simply applied in rows perpendicular to the line of the wound. Compared with skin glue, they are easy to use and much cheaper. However, they are also less robust, are not waterproof and often need to be changed. They can come unstuck quickly if used over joints, in hairy areas or moist skin creases or folds. They can also cause skin reactions in some patients.
Suturing guidelines
Here are some examples of suture materials used in common general surgery procedures.
Before we start, an important disclaimer: these are based on my experience in the NHS in the North-East of England, but the suture materials used in different settings will vary depending on available resources, hospital policies and individual surgeons’ preferences. Even if these don’t exactly match what happens in your hospital, I hope you can recognise the underlying principles we have discussed being applied across this range of procedures.
Simple finger laceration
- interrupted 4/0 or 5/0 Ethilon to skin
- arrange removal of sutures in 10-14 days
Simple forehead laceration
- interrupted 5/0 or 6/0 Prolene to skin
- arrange removal of sutures in 4-5 days
- consider skin glue or Steri-strips in small children
Excision of sebaceous cyst or lipoma
- interrupted 2/0 Vicryl to subcutaneous fat
- usually subcuticular 3/0 Monocryl or undyed Vicryl to skin, sometimes interrupted Ethilon or Prolene if the wound is in an awkward location (e.g. the scalp) or a body area with thick skin (e.g. the back)
Inguinal hernia repair
- continuous 3/0 Prolene to secure lower edge of mesh to inguinal ligament
- interrupted 3/0 Prolene to secure upper part of mesh to conjoint tendon and internal oblique fascia
- continuous 0 Vicryl to external oblique aponeurosis
- continuous 2/0 Vicryl to Scarpa’s fascia
- interrupted or continuous 2/0 Vicryl to subcutaneous fat
- subcuticular 3/0 Monocryl or undyed Vicryl to skin
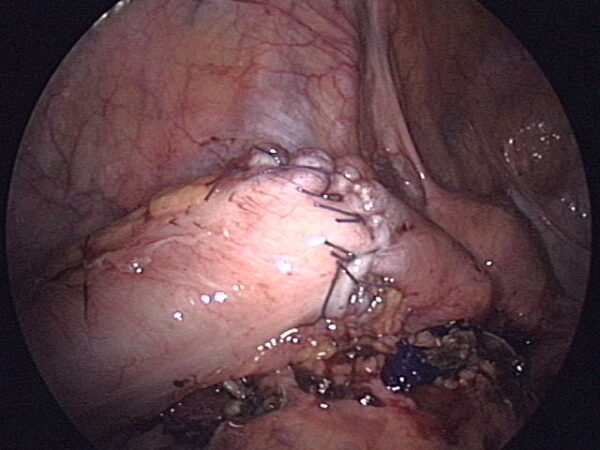
Laparoscopic appendicectomy or cholecystectomy
- interrupted 0 PDS on a J-shaped needle to fascia of all port sites larger than 5mm
- either subcuticular 3/0 Monocryl or glue to skin (or both)
- heavy silk to secure any drains
Midline laparotomy
- continuous 1 PDS to midline fascia
- interrupted 2/0 Vicryl to subcutaneous fat
- either subcuticular 3/0 Monocryl or staples to skin, depending on the amount of contamination and how quickly the patient needs to get to the ICU
- heavy silk to secure any drains
- interrupted 3/0 Vicryl Rapide to form any new stomas
Pfannenstiel incision
- continuous 2/0 Vicryl to parietal peritoneum (this is optional but it keeps the bowel out of the way)
- interrupted 0 Vicryl to reapproximate rectus abdominis muscles
- continuous 1 PDS to rectus sheath fascia
- interrupted 2/0 Vicryl to subcutaneous fat
- subcuticular 3/0 Monocryl to skin
Femoral embolectomy
- continuous 5/0 Prolene to arteriotomy +/- patch
- continuous 2/0 Vicryl to fascial tissues
- continuous 2/0 Vicryl to subcutaneous fat
- either subcuticular 3/0 Monocryl or staples to skin
Good luck, and may the forceps be with you!
Editor
Dr Chris Jefferies
References
Reference texts
- Mackenzie D. The history of sutures. SSHM 1971. Available from: [LINK]
- Byrne M, Aly A. The Surgical Needle. Aesthet Surg J 2019 Mar 14;39(Suppl_2):S73-S77. Available from: [LINK]
- USP Pharmacopeia 2007: Non-Absorbable Surgical Suture. Available from: [LINK]
- Ethicon Wound Closure Manual 2005. Available from: [LINK]
- Byrne M, Aly A. The Surgical Suture. Aesthet Surg J 2019 Mar 14;39(Suppl_2):S67-S72. Available from: [LINK]
- National Institute for Health and Care Excellence 2021. MTG59 Plus Sutures for preventing surgical site infection. Available from: [LINK]
- Yag-Howard C. Sutures, needles, and tissue adhesives: a review for dermatologic surgery. Dermatol Surg. 2014 Sep;40 Suppl 9:S3-S15. Available from: [LINK]
Image references
- Figure 1. Geeky Medics. Suture materials.
- Figure 2. Geeky Medics. Parts of a suture needle.
- Figure 3. Rocco Cusari. Surgical needles. Licence: [Public domain]
- Figure 4. Geeky Medics. Suture packaging.
- Figure 5. Saltanat ebli. Vicryl surgical suture. Licence: [Public domain]
- Figure 6. Geeky Medics. Classification of suture materials.
- Figure 7. Amehta619. Iris repair suture. Licence: [CC BY-SA]
- Figure 8. Sala-Pérez et al. Figure 3. Licence: [CC BY-SA]
- Figure 9. Adapted from Edis et al. Figure 2. Licence: [CC BY-SA]
- Figure 10. Sala-Pérez et al. Figure 4. Licence: [CC BY-SA]
- Figure 11. آرمین. Chromic (sterilized surgical suture). Licence: [Public domain]
- Figure 12. Saltanat ebli. Vicryl surgical suture 3-0.31mm. Licence: [CC BY-SA]
- Figure 13. n.raveender. Thyroid surgery. Licence: [CC BY-SA]
- Figure 14. Lamiot. Hallux valgus or bunion 03. Licence: [CC BY-SA]
- Figure 15. Azoreg. Cesarean section scar and linea nigra. Licence: [CC BY-SA]
- Figure 16. Starvee44. Scar, two months after total thyrodectomy. Licence: [Public domain]
- Figure 17. Anpol42. Manual anastomosis of sigma colon. Licence: [CC BY-SA]
- Figure 18. Saltanat ebli. Sterilized surgical suture (silk).1USP.4 Metric. Licence: [Public domain]
- Figure 19. Red minx. Central line sutures. Licence: [CC BY-SA]
- Figure 20. DDP68. SL suture. Licence: [CC BY-SA]
- Figure 21. Lena Gulenko. Heart valve replacement operations. Licence: [CC BY-SA]
- Figure 22. Adapted from Wang et al. Figure 2. Licence: [CC BY-SA]
- Figure 23. Hellerhoff. Mechanische Aortenklappe 78M – CR ap – 001. Licence: [CC BY-SA]
- Figure 24. Adapted from Michel et al. Figure 1. Licence: [CC BY-SA]
- Figure 25. Jeanne Oostdyk. Suture, before and after, RMO. Licence: [CC BY-SA]
- Figure 26. Dexter Roberts. Sutures a patients hand. Licence: [Public domain]
- Figure 27. Megor1. A human eye 1 day after a corneal transplant. Licence: [CC BY-SA]
- Figure 28. Werneuchen. Atraumatisches Nahtmaterial 17. Licence: [Public domain]
- Figure 29. Kuroczynski. Coarctatio aortae 04 – after end-to-end anastomosis. Licence: [CC BY-SA]
- Figure 30. آرمین. After orthopedic surgery. Licence: [Public domain]
- Figure 31. Steven Fruitsmaak. Skin stapler closeup. Licence: [CC BY-SA]
- Figure 32. Karl-Heinz Wellman. Hip replacement, surgical staples 01. Licence: [CC BY-SA]
- Figure 33. ragesoss. Incision wound on a child’s arm. Licence: [CC BY-SA]
- Figure 34. Kim. Cholecystectomy incisions 4 days post operation. Licence: [CC BY-SA]
- Figure 35: Z22. Steri-Strip tape and glue. Licence: [CC BY-SA]
- Figure 36. Rightdent. Ventral hernia repair 1 week. Licence: [CC BY-SA]