- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
The ankle-brachial pressure index (ABPI) is a non-invasive method of assessing peripheral arterial perfusion in the lower limbs.
ABPI is a ratio composed of the blood pressure of the upper arm (brachial artery) and the blood pressure of the lower limb (dorsalis pedis and the posterior tibial artery). This guide provides a step-by-step approach to performing ABPI measurement in an OSCE setting.
Gather equipment
Gather the relevant equipment to perform ABPI measurement:
- Sphygmomanometer: to assess blood pressure.
- Doppler probe: make sure to check the Doppler probe is functioning correctly.
- Ultrasound gel
Introduction
Wash your hands and don PPE if appropriate.
Introduce yourself to the patient including your name and role.
Confirm the patient’s name and date of birth.
Briefly explain what the procedure will involve using patient-friendly language: “Today I need to measure the blood pressure in your arm and ankle. This will involve inflating a cuff around your arm and ankle briefly and then listening to your pulse with a probe. It shouldn’t be painful, but it may feel a little tight temporarily. If you want me to stop at any point, just let me know.”
Gain consent to proceed with ABPI measurement.
Ask if the patient has diabetes: individuals with diabetes often have calcified vessels which are less compressible. These calcified vessels can, therefore, cause misleadingly high ABPI results. In such cases, the toe pressure can be measured instead of the ankle pressure (using a special toe cuff). This is known as the toe brachial pressure index (TBPI).
Ask the patient if they have any pain before continuing with the clinical procedure.
Position the patient so that they are lying on the examination couch: if the patient has leg ulcers these can be covered in sterile cling-film and the cuff applied as normal, provided it isn’t too uncomfortable for the patient.
Measure ABPI
Measure the brachial pressure
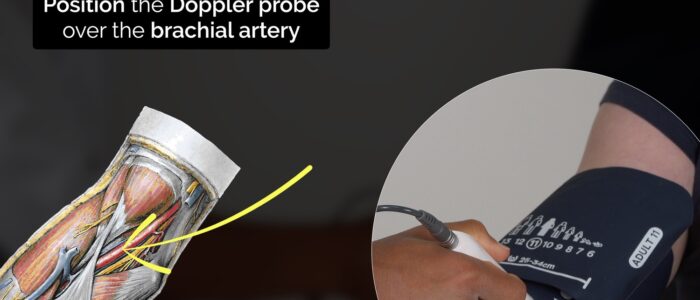
1. With the patient lying on the examination couch, place the sphygmomanometer cuff over the left arm proximal to the brachial artery and position the Doppler probe on the brachial artery at a 45° angle (medial to the biceps tendon in the antecubital fossa).
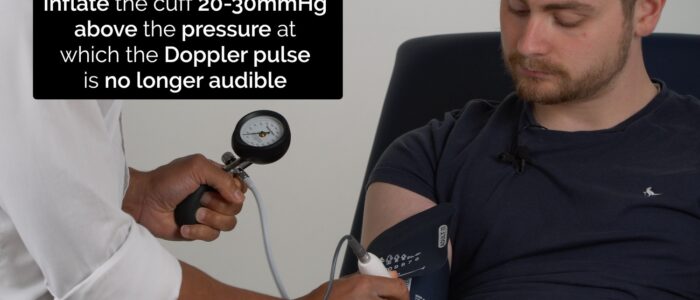
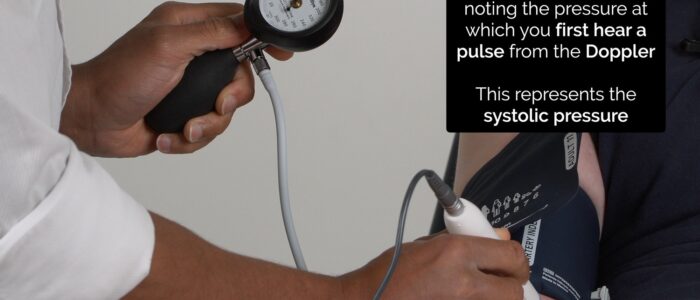
2. Inflate the cuff 20-30 mmHg above the pressure at which the Doppler pulse is no longer audible and then deflate the cuff slowly, noting the pressure at which you first detect a pulse from the Doppler. This represents the systolic pressure in the vessel being assessed.
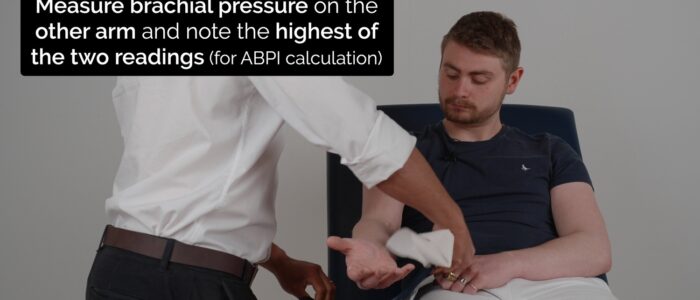
3. Now repeat steps 1 and 2 on the right brachial artery to assess systolic pressure.
4. Record the higher of the two systolic readings when calculating ABPI.
Measure the ankle pressure
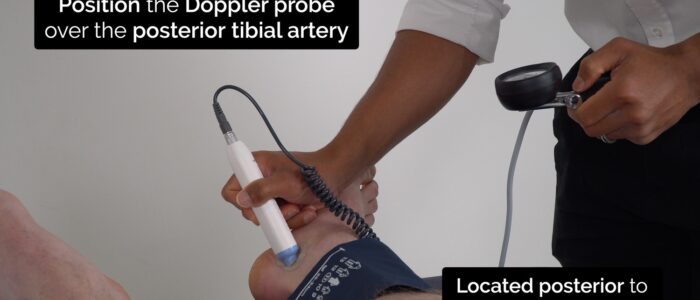
1. Place the sphygmomanometer on the left ankle and position the Doppler probe over the posterior tibial artery, which is located posterior to the medial malleolus.
2. Inflate the cuff 20-30 mmHg above the pressure at which the Doppler pulse is no longer audible, and then deflate the cuff slowly, noting the pressure at which you first detect a pulse from the Doppler. This represents the systolic pressure in the vessel being assessed.
3. Keep the sphygmomanometer in the same location but re-position the Doppler probe over the dorsalis pedis artery of the left foot, which is located lateral to the extensor hallucis longus tendon.
4. Assess the systolic pressure in the dorsalis pedis artery of the left foot by repeating step 2.
5. Record the highest of the two pressures obtained from dorsalis pedis (DP) and the posterior tibial artery (PTA) for use when calculating the left ABPI.
6. Repeat the same process on the right leg to calculate the right ABPI.
Calculate ABPI
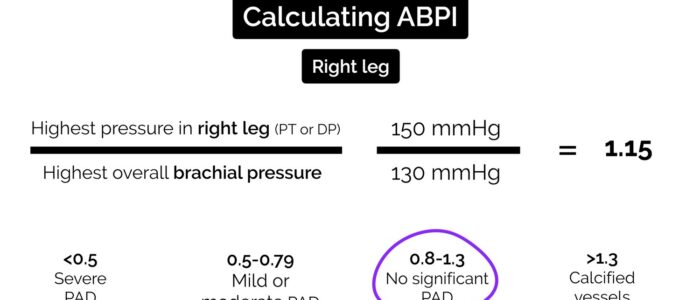
Left ABPI = (highest pressure of either left PTA or DP) ÷ (highest brachial pressure)
Right ABPI = (highest pressure of either right PTA or DP) ÷ (highest brachial pressure)
Erroneous results can occur due to:
- Incorrectly positioned cuff
- Irregular pulse (e.g. atrial fibrillation)
- Calcified vessels (e.g. diabetes)
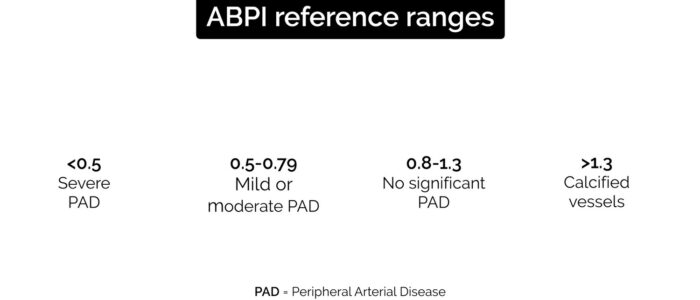
| ABPI value | Interpretation |
| >1.3 | Calcified vessels often cause unusually high ABPI results. In this scenario, further assessments such as duplex ultrasound and angiography are advised to accurately assess perfusion. |
| 0.8-1.3 | No evidence of significant peripheral arterial disease |
| 0.5-0.79 | Mild or moderate arterial disease: typical presenting features include claudication |
| <0.5 | Severe arterial disease: typical presenting features include rest pain, ulceration and gangrene. This is also known as critical limb ischaemia. |
Worked example
Right brachial artery: 120 mmHg
Left brachial artery: 125 mmHg
Right dorsalis pedis: 80 mmHg
Right posterior tibial artery: 75 mmHg
Right ABPI = 80/125 = 0.64 (moderate arterial disease)
To complete the procedure…
Explain to the patient that the procedure is now complete.
Thank the patient for their time.
Dispose of PPE appropriately and wash your hands.
Document the left and right ABPI results in the patient’s notes.
Suggest further assessments and investigations
- Peripheral arterial exam: to assess for clinical signs of peripheral arterial disease.
- Blood tests: as part of a general assessment of vascular risk factors (e.g. serum cholesterol, HbA1c).
- Further imaging: such as duplex ultrasound or a CT/MRI angiogram.
Reviewer
Mr Peter Gogalniceanu
Vascular Surgeon
References
- Mo Al-Qaisi, David M Nott, David H King, and Sam Kaddoura. (2009). Ankle Brachial Pressure Index (ABPI): An update for practitioners. Vasc Health Risk Manag. 5, 833–841.
- McDermott MM, Criqui MH, Liu K, Guralnik JM, Greenland P, Martin GJ, Pearce W (2000). “Lower ankle/brachial index, as calculated by averaging the dorsalis pedis and posterior tibial arterial pressures, and association with leg functioning in peripheral arterial disease”. J Vasc Surg. 32 (6): 1164–71
- Gogalniceanu P, Pegrum J, Lynn W. (2015) Physical Examination for Surgeons – a guide to the MRCS OSCE. Cambridge University Press, UK.