- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
The brachial plexus is a complex intercommunicating network of nerves formed by spinal nerves C5, C6, C7, C8 and T1. The brachial plexus, frequently appears in examination questions.
This guide will cover the brachial plexus and includes a summary diagram. One of the best ways to memorise the brachial plexus is by drawing it.
If you’d like to put your knowledge of the brachial plexus to the test, take a look at the Geeky Medics brachial plexus quiz.
Overview of the brachial plexus
The brachial plexus is a complex intercommunicating network of nerves formed by spinal nerves C5, C6, C7, C8 and T1.
It supplies all sensory innervation to the upper limb and most of the axilla, with the exception of an area of the medial upper arm and axilla, which is supplied by the intercostobrachial nerve T2.
It supplies all motor innervation to the muscles of the upper limb and shoulder girdle, with the exception of the trapezius, which is supplied by the spinal accessory nerve XI.
It also supplies autonomic innervation to the upper limb by intercommunicating with the stellate ganglion of the sympathetic trunk at the level of T1, where it gains sympathetic fibres which supply specialist functions:
- Vasomotor: stimulates vasoconstriction of arteries, arterioles and capillaries resulting in skin pallor and coldness
- Pilomotor: stimulates contraction of arrector pili muscles within hair follicles, making hairs stand on end
- Sudomotor or secretomotor: stimulates the production of sweat from sweat glands
Outline of the brachial plexus
The brachial plexus begins as the anterior rami of five spinal nerve roots C5-T1, which emerge from the intervertebral foramen of their respective vertebrae to lie in the posterior triangle of the neck between the anterior and medial scalene muscles.
The five spinal nerves quickly unite to form superior, middle and inferior trunks, which continue to pass laterally between the anterior and medial scalene muscles and cross the base of the posterior triangle of the neck, where they can be found behind the subclavian artery. They pass over the apex of the lung and the first rib towards the clavicle.
Behind the middle third of the clavicle, each trunk splits into an anterior division and a posterior division. These continue to pass downwards behind the clavicle to enter the axilla.
The six divisions combine to form lateral, posterior and medial cords. These are distributed around and named according to their relationship with the second part of the axillary artery, which is located behind the pectoralis minor muscle.
The cords travel laterally with the axillary artery towards the arm. The artery and cords are ensheathed by an extension of the prevertebral fascia known as the axillary sheath, this is a target for brachial plexus nerve blocks.
The cords divide around the third part of the axillary artery into their five terminal branches: the musculocutaneous, axillary, radial, median and ulnar nerves.
Vascular supply
The brachial plexus gets its blood supply from various branches of the subclavian artery along its length, including:
- Roots: vertebral artery, anterior and posterior spinal arteries
- Trunks and divisions: ascending and deep cervical arteries, superior intercostal artery
- Cords: axillary artery
Structure of the Brachial Plexus
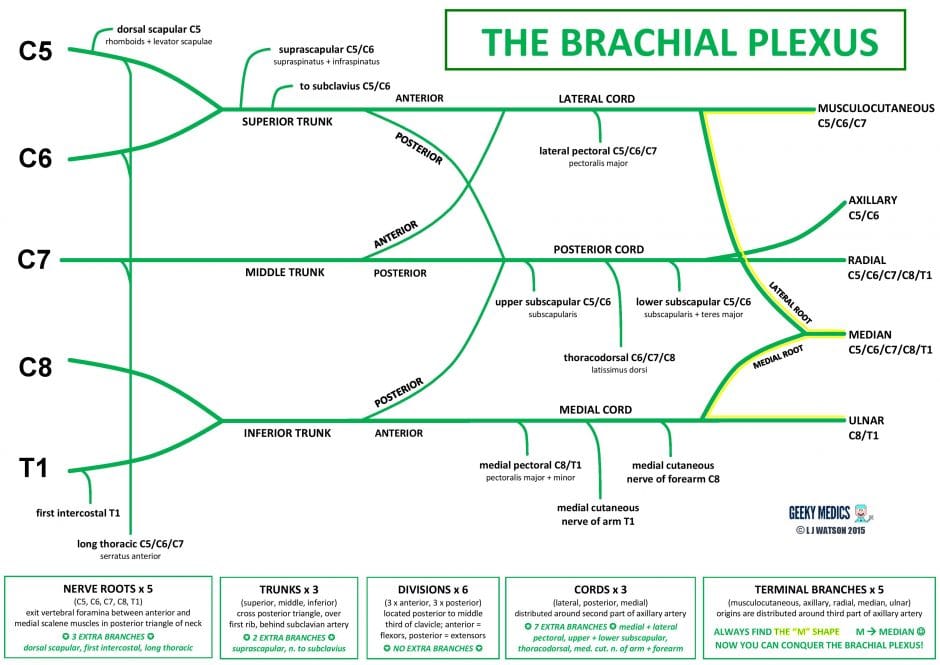
Figure 1 summarises the structure and branches of the brachial plexus.
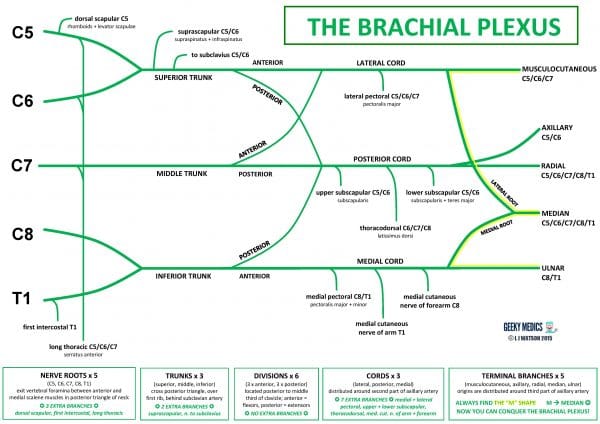
The brachial plexus is easier to understand once broken down into its component segments: these are roots, trunks, divisions, cords and terminal branches.
Roots
There are five nerve roots from C5-T1, which give three nerve branches:
- Dorsal scapular nerve
- Long thoracic nerve
- First intercostal nerve
It is important to remember that C5 also gives fibres which join fibres from C3 and C4 to form the phrenic nerve, which is not shown in the diagram.
Trunks
The five nerve roots combine to form three trunks:
- The superior trunk is formed from C5 and C6
- The middle trunk is formed from C7
- The inferior trunk is formed from C8 and T1
The superior trunk gives rise to two nerve branches: the suprascapular nerve and the nerve to subclavius. The middle and inferior trunks do not give off any extra branches.
Divisions
There are six divisions in total, comprising of an anterior division and a posterior division from each of the three trunks:
- Anterior division fibres usually supply flexor muscles
- Posterior division fibres usually supply extensors
- There are no extra nerve branches arising from the divisions
Cords
The divisions combine to form three cords, which are distributed around the axillary artery:
- The lateral cord is formed from the anterior divisions of the superior and middle trunks. It gives one extra nerve branch: the lateral pectoral nerve.
- The posterior cord is formed from the posterior divisions of the superior, middle and inferior trunks. It gives three nerve branches: the upper subscapular nerve, the thoracodorsal nerve and the lower subscapular nerve.
- The medial cord is formed from the anterior division of the inferior trunk. It gives three nerve branches: the medial pectoral nerve, the medial cutaneous nerve of the arm (also known as the medial brachial cutaneous nerve) and the medial cutaneous nerve of the forearm (also known as the medial antebrachial cutaneous nerve).
Terminal branches
The three cords branch to form five terminal nerve branches which supply the upper limb:
- The lateral cord gives rise to the musculocutaneous nerve and the lateral root of the median nerve
- The posterior cord gives rise to the axillary nerve and the radial nerve
- The medial cord gives rise to the medial root of the median nerve and the ulnar nerve
Identifying structures
It is easy to panic when given a diagram or prosection of the brachial plexus to label in exams. The key is to look for the “M” shape formed around the axillary artery by the musculocutaneous, median and ulnar nerves.
This is an easy landmark to find and will give you your bearings. Once you have found this, you should be able to confidently identify those three nerves. You will then be able to identify the small axillary nerve and large radial nerve originating from the posterior cord behind the axillary artery.
The medial cutaneous nerves of the arm and forearm can be found travelling down the arm below the ulnar nerve. The three branches from the posterior cord should also be easy to spot, you will see the two small subscapular nerves and the large thoracodorsal nerve between them, which forms a bundle with the thoracodorsal artery and vein to supply latissimus dorsi.
Anatomical variations
There are many recognised anatomical variations to this structure, which may affect over 50% of people. The most significant ones include:
- Pre-fixed brachial plexus: contributing nerve roots all moved up one, therefore the plexus is derived from C4-C8
- Post-fixed brachial plexus: contributing nerve roots all moved down one, therefore the plexus is derived from C6-T2
- Individual nerves may also arise from different cords, intercommunicate with others or be completely absent.
Nerve branches from the roots
Dorsal scapular nerve (C5)
Origin
C5 nerve root of the brachial plexus
Sensory supply
None
Motor supply
Levator scapulae (elevates scapula)
Rhomboid major and rhomboid minor (stabilise, retract and medially rotate scapula)
Long thoracic nerve (C5/C6/C7)
Origin
C5, C6 and C7 nerve roots of the brachial plexus
Sensory supply
None
Motor supply
Serratus anterior (protracts and stabilises scapula)
Clinical significance: long thoracic nerve
An injury to the long thoracic nerve, for example as a result of a sports injury or damage during axillary surgery, results in winging of the scapula on examination.
The deformity may be visible at rest, and a classic way to elicit or exaggerate it is by asking the patient to push against a wall and looking for abnormal posterior protrusion of the scapula on the affected side.
First intercostal nerve (T1)
Origin
T1 nerve root of the brachial plexus
Sensory supply
A narrow strip of skin over first intercostal space
Motor supply
First intercostal muscles (elevate and depress the rib cage during inspiration and expiration)
Nerve branches from the trunks
Suprascapular nerve (C5/C6)
Origin
Superior trunk of the brachial plexus
Sensory supply
Glenohumeral and acromioclavicular joints
Motor supply
Supraspinatus (stabilises and abducts shoulder) and infraspinatus (stabilises and externally rotates shoulder)
Nerve to subclavius (C6)
Origin
Superior trunk of the brachial plexus
Sensory supply
None
Motor supply
Subclavius (depresses clavicle and elevates the first rib)
Branches from the cords
Lateral pectoral nerve (C5/C6/C7)
Origin
Lateral cord of the brachial plexus
Sensory supply
None to the skin, but it is thought to play an important role in the sensation of chest wall pain, for example after mastectomy or breast implant insertion, and is, therefore, a target for regional nerve blocks
Motor supply
Upper clavicular part of the pectoralis major (flexes, adducts and internally rotates shoulder)
Upper subscapular nerve (C5/C6)
Origin
Posterior cord of the brachial plexus
Sensory supply
None
Motor supply
Subscapularis (stabilises and internally rotates shoulder)
Lower subscapular nerve (C5/C6)
Origin
Posterior cord of the brachial plexus
Sensory supply
None
Motor supply
Subscapularis (stabilises and internally rotates shoulder) and teres major (adducts and internally rotates shoulder, protracts and depresses scapula)
Thoracodorsal nerve (C6/C7/C8)
Origin
Posterior cord of the brachial plexus
Sensory supply
None
Motor supply
Latissimus dorsi (extends, adducts and internally rotates shoulder, externally rotates trunk)
Clinical significance: thoracodorsal nerve
The thoracodorsal nerve is vulnerable to injury during axillary dissection, for example during lymph node clearance for breast cancer.
This results in shoulder movement weakness, which is best elicited on examination by asking the patient to place the dorsum of their hand on the opposite buttock to test extension, adduction and internal rotation.
Most patients do not suffer from significant loss of function in terms of day-to-day activities, but elderly people may struggle to pull themselves up from a sitting position, and young climbers or bodybuilders are likely to notice significantly reduced performance on the affected side.
Medial pectoral nerve (C8/T1)
Origin
Medial cord of the brachial plexus
Sensory supply
None to the skin, but may have a role in the sensation of chest wall pain following breast surgery
Motor supply
Pectoralis minor (stabilises scapula, raises ribs during inspiration)
Lower sternocostal part of the pectoralis major (extends, adducts and internally rotates shoulder)
Medial cutaenous nerve of the arm (T1)
Origin
Medial cord of the brachial plexus
Sensory supply
Skin of the lower third the of the medial arm
Motor supply
None
Medial cutaneous nerve of the forearm (C8)
Origin
Medial cord of the brachial plexus
Sensory supply
Skin over biceps muscle, antecubital fossa and medial forearm
Motor supply
None
Terminal branches
For more information on the terminal branches, see the Geeky Medics guide to the nerve supply to the upper limb.
Musculocutaneous nerve (C5/C6/C7)
Origin
Lateral cord of the brachial plexus
Sensory supply
Lateral forearm
Motor supply
Anterior compartment of the arm:
- Biceps (flexes elbow, supinates forearm)
- Brachialis (flexes elbow)
- Coracobrachialis (adducts shoulder, flexes elbow)
Clinical significance: musculocutaenous nerve
Musculocutaneous nerve injuries are rare, but result in very weak elbow flexion and weak forearm supination which can be very disabling.
Axillary nerve (C5/C6)
Origin
Posterior cord of the brachial plexus
Sensory supply
“Sergeant’s patch” over the lower deltoid
Motor supply
Deltoid (abducts, flexes and extends shoulder) and teres minor (stabilises and externally rotates shoulder)
Clinical significance: axillary nerve
The axillary nerve may be injured by shoulder dislocations or proximal humeral fractures, resulting in numbness over the sergeant’s patch and profound weakness of shoulder abduction from 15-90°.
Other examination findings include deltoid wasting and weakness of shoulder flexion, extension and external rotation.
Radial nerve (C5/C6/C7/C8/T1)
Origin
Posterior cord of the brachial plexus
Sensory supply
The radial nerve supplies sensation to:
- Posterior arm and forearm
- Lateral ⅔ of the dorsum of the hand
- Proximal dorsal aspect of lateral 3½ fingers
Motor supply
The radial nerve supplies the posterior compartment of the arm, which contains triceps (extends and adducts shoulder, extends elbow).
It also supplies the entirety of the posterior compartment of the forearm. This consists of:
- Brachioradialis (flexes elbow)
- Anconeus (extends elbow, stabilises elbow joint)
- Supinator (supinates forearm)
- Extensor carpi radialis longus and brevis (extend and abduct wrist)
- Extensor carpi ulnaris (extend and adduct wrist)
- Extensor digitorum
- Extensor pollicis longus and brevis
- Extensor indicis
- Extensor digiti minimi
- Abductor pollicis longus (abducts thumb)
Clinical significance: radial nerve
Radial nerve injuries are commonly due to compression, for example by leaning or lying on the arm for extended periods, excessively tight plaster casts or prolonged tourniquet use. It can also be damaged by fractures of the humerus or radius, or by stab wounds.
Radial nerve injury results in loss of innervation to the muscles of the posterior compartments of the arm and forearm. This manifests as numbness in the radial nerve distribution and a “wrist drop” deformity with very weak extension of the elbow, wrist and fingers.
Median nerve (C5/C6/C7/C8/T1)
Origin
Lateral and medial cords of the brachial plexus
Sensory supply
The median nerve supplies sensation to:
- Thenar eminence, the lateral ⅔ of the palm of the hand
- Palmar aspect of lateral 3½ fingers
- Dorsal fingertips of lateral 3½ fingers
Motor supply
All muscles of the anterior compartment of forearm except flexor carpi ulnaris and the medial two parts of flexor digitorum profundus.
The median nerve, therefore, supplies pronator teres, flexor carpi radialis, palmaris longus, flexor digitorum superficialis, the lateral two parts of flexor digitorum profundus, flexor pollicis longus and pronator quadratus.
These forearm muscles flex the wrist, the proximal interphalangeal joints of all four fingers and the distal interphalangeal joints of the index and middle fingers. They also pronate the forearm and abduct the wrist.
The median nerve also supplies the LOAF muscles of the hand:
- Lateral two lumbricals
- Opponens pollicis
- Abductor pollicis brevis
- Flexor pollicis brevis
The lumbricals flex the MCPJs and extend the IPJs of the index and middle finger.
The muscles of the thenar eminence flex, abduct and oppose the thumb.
Clinical significance: median nerve
The median nerve is most commonly damaged by compression within the carpal tunnel at the wrist, resulting in numbness of the median nerve distribution to the hand, wasting of the thenar eminence, weak grip strength and a “hand of benediction” deformity due to an inability to flex the index or middle fingers.
It can also be injured by supracondylar fractures of the humerus and stab wounds or lacerations to the forearm or wrist.
Ulnar nerve (C8/T1)
Origin
Medial cord of the brachial plexus
Sensory supply
The ulnar nerve supplies sensation to:
- Hypothenar eminence
- Medial ⅓ of the palm of the hand
- Palmar aspect of the medial 1½ fingers
- Medial ⅓ of the dorsum of the hand
- Dorsal aspect of the medial 1½ fingers
Motor supply
The ulnar nerve supplies just two muscles in the anterior compartment of the forearm:
- Flexor carpi ulnaris, which flexes and adducts the wrist
- The medial two parts of flexor digitorum profundus, which flex the distal interphalangeal joints (DIPJs) of the ring and little fingers.
It also supplies the intrinsic muscles of the hand except the LOAF muscles supplied by the median nerve. These can be remembered as the HILA muscles:
-
- Hypothenar eminence
- Interossei
- Medial two lumbricals
- Adductor pollicis
The hypothenar eminence consists of opponens digiti minimi, flexor digiti minimi brevis and abductor digiti minimi, which oppose, flex and abduct the little finger respectively.
The palmar interossei adduct the fingers, whilst the dorsal interossei abduct them.
The medial two lumbricals flex the MCPJs and extend the IPJs of the ring and little fingers.
Adductor pollicis adducts the thumb. This muscle does not form part of the thenar eminence and actually lies deep beneath it as a separate structure.
Clinical significance: ulnar nerve
The ulnar nerve may be injured by supracondylar fractures of the humerus, medial epicondylar fractures, stab wounds to the forearm or wrist, or compression at either the cubital tunnel in the elbow or Guyon’s canal in the wrist.
This results in numbness in the ulnar distribution to the hand, wasting of the hypothenar eminence and intrinsic muscles of the hand, a “claw hand” deformity due to an inability to extend the ring and little fingers, and weak finger abduction and adduction.
Prosected specimen
This labelled prosection specimen sums up the parts of the brachial plexus.

Brachial plexus injuries
It is possible for the brachial plexus to be injured at the level of the cervical nerve roots or trunks in the neck, causing a syndrome of neurological deficits and clinical features.
The most common injuries are Erb’s palsy, Klumpke’s palsy and Horner’s syndrome.
Brachial plexus injuries are rare, but are often appear in exams to test anatomical knowledge.
Types of brachial plexus injury
There are several different types and pathologies of nerve injuries:
- Neurapraxia: the nerve is stretched and damaged but not torn
- Rupture: the nerve is torn at a point along its length
- Axonotmesis: the nerve fibre is partially severed: the axon and myelin sheath are torn but the surrounding epineurium, perineurium and connective tissues are preserved. Natural recovery is possible through axonal regeneration, so these injuries can often be managed conservatively.
- Neurotmesis: the nerve fibre completely severed. There is no prospect of natural recovery, so this type of injury requires surgery to restore function.
- Avulsion: the nerve root is torn off the spinal cord at its origin
- Post-traumatic neuroma: a growth of scar tissue at the site of a previous nerve injury, which leads to compression
Upper brachial plexus injury: Erb’s palsy
Site of the injury
Superior trunk of the brachial plexus (C5/C6) – occasionally the middle trunk (C7) is also involved
Mechanism
Traction injury due to excessive lateral neck flexion towards the contralateral side, or excessive shoulder depression, resulting in violent stretching +/- tearing of the upper portion of the brachial plexus
Causes
The classical cause is a traction injury during difficult or obstructed childbirth, such as shoulder dystocia requiring emergency forceps delivery, or breech presentations with the arms raised above the head.
The stretching mechanism can also be caused by falls onto the neck/shoulder or excessive traction on the arm, for example during sports (often known as “burner syndrome”), motorbiking accidents or attempts to reduce a shoulder dislocation.
It can also result from direct trauma by clavicle fractures, gunshot wounds or stab injuries.
Nerves injured
- Musculocutaneous nerve
- Axillary nerve
- Suprascapular nerve
- Nerve to subclavius
Clinical features
Erb’s palsy results in loss of sensation to the skin over the “sergeant’s patch”, lateral arm and lateral forearm.
There is wasting of the deltoid, supraspinatus and infraspinatus muscles and the anterior compartment of the arm, with loss of shoulder abduction and external rotation, elbow flexion and wrist supination. This results in a “waiter’s tip” deformity characterised by a limp, adducted, internally rotated shoulder, an extended elbow and a pronated wrist.
The biceps reflex is absent. Wrist flexion, wrist extension and finger movements are usually preserved. If C7 is involved, elbow and wrist extension will also be diminished and the wrist may be held in fixed flexion.
Severely affected untreated babies may be left with stunted arm growth, joint contractures and circulatory problems.
Lower brachial plexus injury: Klumpke’s palsy
Site of injury
Inferior trunk of the brachial plexus (C8/T1)
Mechanism
Traction injury due to excessive force placed on an abducted shoulder results in violent stretching +/- tearing of the lower portion of the brachial plexus
Causes
Klumpke’s palsy is the rarest brachial plexus syndrome. The most common cause is a traction injury during difficult childbirth, such as an arm presentation requiring force on the arm to successfully deliver the rest of the baby.
The same mechanism can also be caused by a falling person grabbing onto something (e.g. grabbing a branch when falling from a tree), or by other causes of excessive abduction such as motorbiking accidents.
Direct trauma can result from clavicle fractures, gunshot wounds or stabbings.
It can also be caused by compression of the lower plexus by a mass in the root of the neck, such as lymphoma or lung cancer.
Nerves injured
Median and ulnar nerves
Clinical features
Klumpke’s palsy results in loss of skin sensation in the median and ulnar distributions of the hand, the sensory supply to the lateral dorsum of the hand is preserved as this comes from the radial nerve. There is also loss of sensation in medial forearm and arm.
The injury affects the motor nerve fibres to all small intrinsic muscles of the hand. There is therefore generalised wasting of hand muscles with a loss of MCPJ flexion, IPJ extension, finger abduction and adduction, and opposition.
The anterior compartment of the forearm is also affected, resulting in loss of wrist flexion. This results in a “claw hand” deformity affecting all four fingers, characterised by IPJ flexion and MCPJ hyperextension at rest, and an inability to extend the fingers. The wrist is classically held supinated.
Shoulder and movements are usually preserved. T1 injuries may be associated with Horner’s syndrome, and there may be associated superior/middle trunk injuries.
Total/complete brachial plexus injury
Site of injury
Entire brachial plexus C5/C6/C7/C8/T1
Mechanism
Usually severe or complex traction injuries sustained during difficult childbirth
High-speed road traffic accidents, resulting in violent stretching +/- tearing of all nerve roots
Nerves injured
Entire brachial plexus
Clinical features
Totally limp, dangling, atrophied and numb upper limb with associated Horner’s syndrome
Horner’s syndrome
Site of injury
T1 nerve root
Mechanism
Any injury to the T1 nerve root associated with loss of sympathetic function
Causes
Acquired Horner’s syndrome may be due to a traction injury, direct trauma, cerebral pathology or extrinsic compression. The classical cause is usually a Pancoast tumour in the apex of the lung.
Nerves injured
T1 nerve root, sympathetic trunk or stellate ganglion
Clinical features
Horner’s syndrome causes loss of sympathetic nerve supply to the face and neck. The key features are ipsilateral partial ptosis (drooping eyelid), miosis (constricted pupil), anhidrosis (loss of sweating on affected side of face), dilatation lag (slowly dilating pupil) and enophthalmos (eye appears sunken).
With traction injuries there may be associated Klumpke’s palsy. With nerve root compression there may be associated hand/arm pain and wasting of the intrinsic muscles of the hand, this should trigger alarm bells for an underlying malignancy.
Thoracic outlet syndrome
Site of injury
Trunks of brachial plexus, classically the inferior trunk but can affect any or all of the trunks
Mechanism
Compression of neurovascular structures at the level of the thoracic outlet between the root of the neck and the upper thorax. The thoracic outlet is bounded by the scalene muscles, the first rib, and the clavicle.
Causes
Causes of thoracic outlet syndrome include:
- Congenital fibrous tissue band
- Cervical rib
- Musculoskeletal abnormality
- Acquired pathology such as whiplash trauma, repetitive strain/sports injury
- Malunion of a clavicular fracture
- Underlying malignancy such as lymphoma or lung cancer.
Nerves injured
Classically, the ulnar nerve, but may affect any combination of nerves supplying the upper limb.
In about 5% of cases, compression may also affect the subclavian artery and/or vein which run with the trunks through the thoracic outlet.
Clinical features
Thoracic outlet syndrome leads to a combination of neurological and vascular symptoms. Neurological features include wasting of the intrinsic muscles of the hand with reduced grip strength, and some patients may experience numbness or paraesthesia. Some patients report neuropathic pain affecting the arm, shoulder and neck.
Vascular symptoms tend to be brought on or exacerbated by vigorous overhead activities, such as lifting or throwing. Subclavian artery compression causes aching or painful claudication of the arm, pallor and extreme cold; severe cases may lead to ischaemia with ulceration and gangrene. Subclavian vein compression can result in diffuse arm pain and swelling, venous distension and cyanosis.
Venous obstruction may lead to thrombosis of the subclavian or axillary veins, which is known as Paget-Schroetter syndrome.
Brachial neuritis / plexitis
Site of injury
Any part of brachial plexus – may affect individual nerves/cords or entire plexus
Mechanism
Inflammatory reaction against the nerves of the brachial plexus
Causes
Brachial neuritis may be idiopathic (Parsonage-Turner syndrome). Commonly recognised triggers include bacterial, viral or parasitic infections, immunisations, trauma, childbirth, recent surgery or radiotherapy, and systemic inflammatory disorders such as lupus, polyarteritis nodosa or other types of vasculitis.
It may also occur as part of a polyneuropathy, such as Guillain-Barre syndrome or motor neurone disease, or as a paraneoplastic syndrome associated with lymphoma.
Nerves injured
Any component of brachial plexus
Clinical features
Brachial neuritis classically starts with the sudden onset of excruciating shoulder and arm pain on the affected side, followed by the development of paralysis and atrophy of affected muscle groups within a couple of weeks.
The onset of symptoms may be preceded by prodromal symptoms of a systemic infection, or another immunological trigger such as trauma, surgery or immunisation. The syndrome is particularly associated with hepatitis E virus infection, occurring bilaterally in up to 10% of cases.
Patients usually present acutely due to the severity of the pain and tend to support the affected arm in an adducted, internally rotated position. The phrenic nerve or lower cranial nerves may also be affected in a minority of cases.
Summary diagram
Editor
Dr Chris Jefferies
References
- Chhabra A, Thawait GK, Soldatos T et al; High-Resolution 3T MR Neurography of the Brachial Plexus and Its Branches, with Emphasis on 3D Imaging. American Journal of Neuroradiology. Published in 2013;
- Heise C et al; Neonatal brachial plexus palsy: a permanent challenge. Arquivos de Neuro-Psiquiatra 2015 73(9)
- Netter FH. Atlas of Human Anatomy, 5th Edition. Published in 2010.
- Paradowski B et al; Plexiform neurofibromas of the brachial plexus. NeuroImages 2005
- Radiopaedia.org. Pancoast Tumour. Available from: [LINK]
- Sinnatamby CS. Last’s Anatomy, 12th Edition. Published in 2011
- Snell RS. Clinical Anatomy by Regions, 9th Edition. Published in 2011