- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
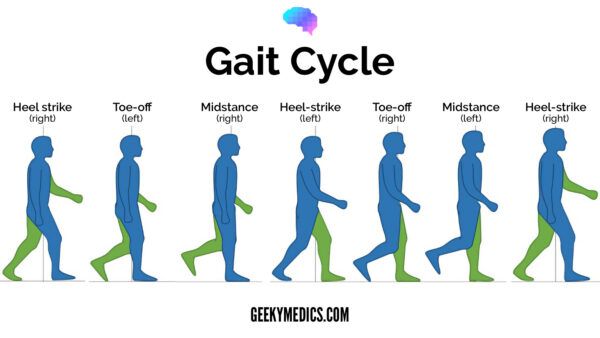
Normal gait cycle
The gait cycle has six phases:
- Heel-strike: initial contact of the heel with the floor.
- Foot flat: weight is transferred onto this leg.
- Mid-stance: the weight is aligned and balanced on this leg.
- Heel-off: the heel lifts off the floor as the foot rises but the toes remain in contact with the floor.
- Toe-off: as the foot continues to rise the toes lift off the floor.
- Swing: the foot swings forward and comes back into contact with the floor with a heel strike (and the gait cycle repeats).
Hemiplegic gait
A hemiplegic gait is typically caused by a lesion in the central nervous system (e.g. stroke) which results in unilateral weakness and spasticity.
Patients with hemiplegia exhibit spastic flexion of the upper limb and extension of the lower limb.
Due to the extension of the lower limb (fixed ankle plantar flexion and knee extension), the leg is elongated meaning patients have to circumduct their leg to prevent their foot from dragging on the ground.
Associated clinical features
Clinical features which may be associated with a hemiplegic gait include:
- Increased tone with clasp-knife spasticity
- Hyperreflexia with or without clonus
- Upgoing plantars (i.e. positive Babinski)
- Reduced power
- Sensory deficit: the pattern of sensory loss depends on the site of the lesion in the nervous system
Causes
Unilateral cerebral lesion:
- Stroke
- Space-occupying lesion
- Trauma
- Multiple sclerosis
Hemisection of the spinal cord:
- Trauma
Diplegic gait
A diplegic gait (a.k.a scissoring gait) may be caused by a lesion in the central nervous system (e.g. stroke, or complete transection of the spinal cord).
Clinical findings are similar to those in hemiplegic gait but are bilateral in nature. Spasticity is typically worse in the lower limbs compared to the upper limbs.
The hips and knees are flexed and adducted whilst the ankles are extended and internally rotated.
The knees are forced together due to spasticity in the adductor muscles resulting in leg overlap when walking (a.k.a. scissoring).
In an attempt to overcome this adduction, the patient circumducts both legs during the swing phase.
The upper limb may have flexor posturing of the elbows and wrist with shoulders and fingers in adduction (known as ‘low guard’ or ‘mid-guard’ position). They also typically lack the swinging movements present in a normal gait.
Associated clinical features
Clinical features which may be associated with a diplegic gait include:
- Increased tone with clasp-knife spasticity
- Hyperreflexia with or without clonus
- Upgoing plantars (i.e. positive Babinski)
- Reduced power
- Sensory deficit – if a diplegic gait is caused by spinal cord pathology, the ‘sensory level’ (ie. the lowest dermatome level with normal sensation) correlates with the level of spinal cord pathology
- Wasting and fasciculations (consider motor neuron disease)
Causes
Spinal cord lesion (sensation usually affected):
- Prolapsed intervertebral disc
- Spinal spondylosis
- Spinal tumour
- Transverse myelitis
- Spinal infarct
- Syringomyelia
- Hereditary spastic paraparesis
Bilateral brain lesion:
- Cerebral palsy
- Multiple sclerosis
- Bilateral brain infarcts
- Midline tumour (e.g. paraspinal meningioma)
Motor neuron disease: associated with lower motor neuron findings
Parkinsonian gait
A Parkinsonian gait (a.k.a. festinant gait) is caused by rigidity and bradykinesia as a result of the loss of dopaminergic neurons in the basal ganglia.
Features of a Parkinsonian gait include:
- Initiation: typically slow to start walking due to failure of gait ignition and hesitancy.
- Step length: reduced stride length with short steps is common (shuffling gait). Each step may get progressively smaller as the patient attempts to retain balance (known as festinant gait).
- Arm swing: reduced arm swing on one or both sides (often an early feature of Parkinson’s disease).
- Posture: flexed trunk and neck causing a stooped appearance.
- Tremor: resting tremor can be observed when the patient is distracted by walking.
- Turning: impaired balance on turning or hesitancy is common due to postural instability.
Associated clinical features
Clinical features which may be associated with a Parkinsonian gait include:
- Tremor
- Rigidity
- Bradykinesia
- Hypomimia
Causes
Features of the Parkinsonian gait are observed in both idiopathic Parkinson’s disease and other Parkinsonian disorders.
Idiopathic Parkinson’s disease usually has most features of the gait described above and the classic triad of tremor, rigidity and bradykinesia.
Other Parkinsonian disorders may only have a few of the gait features, may not have all features of the triad, and may be associated with other findings.
Examples of disorders with Parkinsonian features include:
- Vascular Parkinson’s disease
- Dementia with Lewy bodies
- Parkinson’s plus syndromes (e.g. multisystem atrophy and progressive supranuclear palsy)
- Drug-induced Parkinsonism (e.g. antipsychotics, antiemetics)
- Dementia pugilistica
Ataxic gait
An ataxic gait is typically broad-based and associated with midline cerebellar disease (e.g. alcoholic cerebellar degeneration), vestibular disease (e.g. labyrinthitis) or loss of proprioception (known as sensory ataxia).
Features of an ataxic gait include:
- Stance: a broad-based ataxic gait is typically associated with midline cerebellar pathology (e.g. a lesion in multiple sclerosis or degeneration of the cerebellar vermis secondary to chronic alcohol excess).
- Stability: a staggering, slow and unsteady gait is typical of cerebellar pathology. In unilateral cerebellar disease, patients will veer towards the side of the lesion.
- Turning: patients with cerebellar disease will find the turning manoeuvre particularly difficult.
Associated clinical features
The presence of an ataxic gait may be the result of cerebellar, vestibular or sensory impairment.
Clinical features associated with cerebellar ataxia:
- Nystagmus
- Ataxic dysarthria
- Dysmetria
- Intention tremor
- Dysdiadokokinesia
Clinical features associated with sensory ataxia:
- Positive Romberg’s sign
- Impaired proprioception
- Impaired vibration sensation
- Absence of other cerebellar signs (e.g. dysmetria, nystagmus, dysarthria)
Clinical features associated with vestibular ataxia:
- Vertigo
- Nausea
- Vomiting
Causes
Cerebellar ataxia:
- Cerebellar stroke (ischaemic or haemorrhagic)
- Space-occupying lesion
- Multiple sclerosis
- Alcoholism
- B12 deficiency
- Drugs (e.g. phenytoin, carbamazepine, barbiturates, lithium)
- Genetic disease (e.g. Frederich’s ataxia, spinocerebellar ataxia)
- Paraneoplastic disease
Sensory ataxia:
- Peripheral neuropathy (e.g. diabetes mellitus)
Vestibular ataxia:
- Labyrinthitis
- Meniere’s disease
- Acoustic neuroma
Neuropathic gait
Neuropathic gait (a.k.a. high-steppage gait) is caused by weakness of the muscles in the distal limb (typically the dorsiflexors of the foot) as a result of damage to the peripheral nerves providing motor innervation.
Weakness of the dorsiflexors of the foot results in foot drop and dragging of the toes during the swing phase of the gait cycle. To prevent the toes from dragging on the floor, the knee and hip flex excessively, thereby creating a “high stepping” gait.
Associated clinical features
Clinical features which may be associated with a neuropathic gait include:
- Peripheral vascular disease
- Peripheral sensory impairment
- Distal muscle weakness
- Reduced or absent reflexes
Causes
Foot drop is caused by weakness of the muscles of ankle dorsiflexion (tibialis anterior) supplied by the common peroneal nerve (L4, L5 and S1 nerve root).
Foot drop may therefore be caused by:
- Isolated common peroneal nerve palsy (e.g. secondary to trauma or compression)
- L5 radiculopathy (e.g. disc prolapse)
- Generalized polyneuropathy involving multiple nerves (e.g. diabetic neuropathy, motor neurone disease, Charcot-Marie Tooth disease)
Myopathic gait
A myopathic gait (a.k.a. waddling gait or Trendelenburg gait) occurs due to weakness of the hip abductors resulting in a waddling appearance.
Hip abductor weakness results in an inability to stabilize the pelvis during the stance phase. As a result, the pelvis tilts downwards towards the unsupported side during the swing phase of the gait cycle.
The body compensates to prevent the swinging foot from dragging by:
- Laterally flexing the torso away from the leg in swing phase; this draws the pelvis and leg up off the floor (causing the characteristic ‘waddling’ appearance)
- Circumducting the leg
Associated clinical features
Clinical features which may be associated with a myopathic gait include:
- Difficulty standing from a seated position without the use of the arms
- Difficulty standing from a squat or sitting up from a lying position
- Positive Trendelenburg’s sign; when the patient stands on one leg, the pelvis drops towards the contralateral side
Causes
Systemic disease:
- Hyperthyroidism
- Hypothyroidism
- Cushing’s syndrome
- Acromegaly
- Polymyalgia rheumatica
- Polymyositis
- Dermatomyositis
Muscular dystrophies:
- Duchenne’s muscular dystrophy
- Becker’s muscular dystrophy
- Myotonic dystrophy
Choreiform gait
A choreiform gait (a.k.a. hyperkinetic gait) presents with involuntary movements such as:
- Oro-facial dyskinesia (grimacing or lip-smacking)
- Choreic movements of the upper and lower limbs (writhing, dance like semi-purposeful movements)
The involuntary movements are usually present at rest, however, walking can accentuate the movements.
Causes
Basal ganglia disease:
- Huntington’s disease
- Sydenham’s chorea
- Cerebral palsy (choreiform type)
- Wilson’s disease
- Dopaminergic medications (e.g. Parkinson’s medications)
Antalgic gait
An antalgic gait is an abnormal gait pattern which develops as a result of pain. Typically the stance phase is reduced on the affected leg resulting in a limping appearance.
Causes
Any cause of lower limb pain such as:
- Osteoarthritis
- Inflammatory joint disease
- Lower limb fracture
- Nerve entrapment (e.g. sciatica)
References
- Adapted by Geeky Medics. BoH, CC BY-SA 4.0




