- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Hypothyroidism occurs when there is insufficient thyroid hormone production and secretion by the thyroid gland to meet the body’s demands.
The most common cause of hypothyroidism in developed populations is an autoimmune condition, Hashimoto’s thyroiditis, which results in the underproduction of endogenous thyroid hormones.1
Aetiology
Anatomy
The thyroid gland is a butterfly-shaped structure that sits wrapped around the cricoid cartilage and trachea in the anterior aspect of the neck at the level of C5-T1.2
Normal physiology
Thyroid hormones have a wide range of functions, including regulating basal metabolic rate, weight, internal temperature, hair growth, nail health and skin condition.
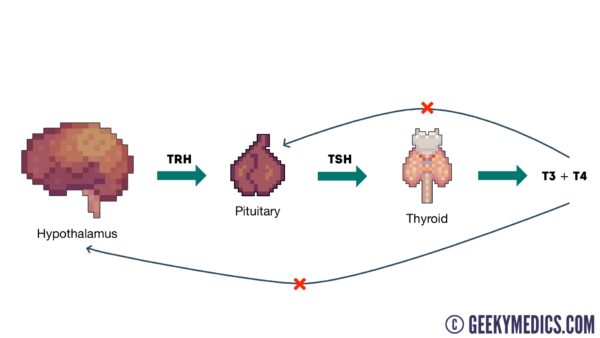
The synthesis of these thyroid hormones is regulated by the hypothalamic-pituitary-thyroid (HPT) axis (Figure 1). Thyrotropin-releasing hormone (TRH), produced by the hypothalamus, stimulates the production of thyroid-stimulating hormone (TSH) from the anterior pituitary gland.
TSH binds to the thyroid gland surface receptors and stimulates the production of T3 (triiodothyronine) and T4 (thyroxine) thyroid hormones, which are produced from the follicular cells of the thyroid gland.3
The HPT axis is regulated by a negative feedback loop whereby a decrease in thyroid gland hormones signals the hypothalamus and anterior pituitary to synthesise more TRH and TSH hormones. However, in hypothyroidism, the HPT axis becomes deranged.
Causes of hypothyroidism
Hypothyroidism can be stratified into primary and secondary causes:4
- Primary hypothyroidism refers to thyroid hormone underproduction caused by the thyroid gland itself
- Secondary hypothyroidism refers to thyroid hormone underproduction caused by the structures/factors external to the thyroid gland
Hashimoto’s disease (autoimmune)
Hashimoto’s (autoimmune) thyroiditis is the most common cause of hypothyroidism in Western populations. Anti-thyroid peroxidase antibodies (anti-TPO) attack the thyroid gland, impairing the gland’s ability to produce thyroid hormones.
It is most common in women aged 30 to 50 and is four to ten times more common in women than men. Individuals with other autoimmune conditions, such as diabetes and rheumatoid arthritis, are more likely to develop autoimmune thyroiditis.5
Iodine deficiency
Iodine deficiency is the most common cause of hypothyroidism worldwide.6 Iodine is a key component of thyroxine (T4) and triiodothyronine (T3). Therefore, a deficiency leads to the underproduction of thyroid hormones.
Congenital hypothyroidism
Congenital hypothyroidism is a condition present from birth where the thyroid gland is underdeveloped or absent, resulting in thyroid hormone deficiency. Symptoms include reduced tone, poor growth, and if untreated, can lead to developmental delay.7
Pituitary tumours
Pituitary tumours such as pituitary adenomas can cause central hypothyroidism by compressing the pituitary gland or interrupting the gland’s blood flow, which can reduce the production of TSH. This can subsequently lead to secondary hypothyroidism due to a lack of stimulation to produce the thyroid hormones.8
De Quervain’s thyroiditis
De Quervain’s thyroiditis is a transient inflammation of the thyroid gland causing three stages: thyrotoxicosis, hypothyroidism and euthyroidism. It is usually triggered by a virus and is a self-limiting condition.9
Post-partum thyroiditis
Following the relative immunosuppressive state of pregnancy, thyroid gland inflammation can occur post-partum. Classically, this is triphasic: hyperthyroidism, hypothyroidism and euthyroidism. However, the hypothyroid period of this condition may persist in 20-30% of cases.10
Iatrogenic
Iatrogenic causes such as medications, sphenoid surgery and radiotherapy to the brain may also cause hypothyroidism. Medications that commonly cause hypothyroidism include amiodarone and lithium.11
Risk factors
Risk factors for hypothyroidism include:12
- A family history of hypothyroidism
- Pregnancy in the last six months
- Autoimmune diseases such as type 1 or 2 diabetes, coeliac disease and rheumatoid arthritis
- Previous thyroid surgery or treatment with radioactive iodine
- Radiation treatment to the head, neck or thorax
Clinical features
History
Typical symptoms of hypothyroidism include:
- Weight gain
- Constipation
- Depression
- Brittle hair and nails
- Irregular or heavy periods
- Loss of libido
- Lethargy
- Cold intolerance
Other important areas to cover in the history include:
- Obstetric history: current or recent pregnancy
- Drug history: to identify any drugs which may cause hypothyroidism (e.g. lithium)
- Past medical history: history of other autoimmune conditions (e.g. rheumatoid arthritis)
- Family history: thyroid or autoimmune disease
Clinical examination
All those presenting with symptoms suggestive of hypothyroidism should have a thyroid status examination.
Typical clinical findings of hypothyroidism on examination may include:13
- Dry skin
- Bradycardia
- Cold peripheries
- Stiff muscles
- Hair loss
Hertoghe’s sign
Hertoghe’s sign (also called Queen Anne’s sign), the loss of the outer third of the eyebrow, is a rare sign of hypothyroidism (Figure 2).

Investigations
Thyroid function tests (TFTs)
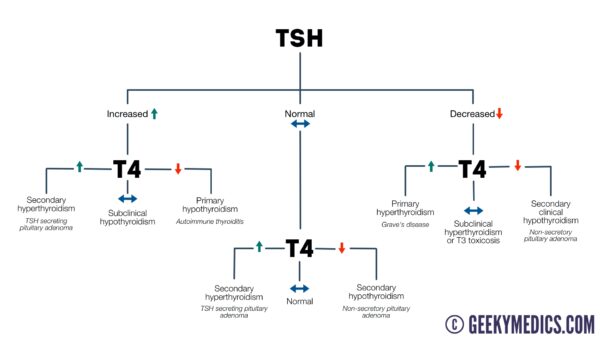
Thyroid function blood tests, including TSH, free T3 and free T4, should be performed when investigating potential thyroid conditions. In hypothyroidism, these tests will show a low free T3 and low free T4.
In primary hypothyroidism, the HPT axis will attempt to correct the deficiency, resulting in a raised TSH. However, in secondary causes, this will be low or normal due to reduced pituitary production of TSH.14
For more information, see the Geeky Medics guide to thyroid function test interpretation.
Autoantibody testing
Testing for autoantibodies such as anti-thyroid peroxidase (anti-TPO) can aid the identification of autoimmune thyroid conditions. TPO antibodies are found in 90% of people with Hashimoto’s thyroiditis. However, they may also be present in Grave’s thyrotoxicosis.15
Imaging
Doppler ultrasound can visualise the thyroid gland to assess for nodules and/or infiltrative disease.
Management
First line management of hypothyroidism is hormone replacement therapy with levothyroxine, a synthetic T4 hormone.
Individuals usually take this life-long, and thyroid function tests should be performed every three months to titrate the medications appropriately. Following a stable TSH level, thyroid function tests should be performed annually.
Complications
Myxoedema coma
Myxoedema coma is a rare and potentially fatal complication of hypothyroidism presenting with altered mental state, hypothermia, bradycardia, and hypoventilation. This is a medical emergency which must be treated rapidly under specialist endocrine input with thyroid replacement therapy, glucocorticoid therapy, and supportive measures.16
Cardiac complications
Individuals with hypothyroidism are at risk of heart disease, including coronary artery disease, heart failure and atherosclerosis, due to its association with elevated serum total and LDL cholesterol.17
Reproductive complications
Overt hypothyroidism is also associated with sub-fertility and may increase the risk of miscarriage, stillbirth, pre-eclampsia and postpartum haemorrhage in pregnancy.18
Key points
- Hypothyroidism is a common endocrine condition caused by low circulating thyroid hormone concentrations
- The most common cause of hypothyroidism in Western populations is Hashimoto’s thyroiditis (autoimmune)
- Symptoms of hypothyroidism, such as weight gain, lethargy and low mood, occur due to a reduced basal metabolic rate
- Thyroid function blood tests are the key investigation and help distinguish primary hypothyroidism from secondary hypothyroidism
- Hypothyroidism is treated by hormone replacement with levothyroxine
- Myxoedema coma, heart disease and reproductive issues are key complications of hypothyroidism
Reviewer
Dr Juliane Kause
Editor
Dr Chris Jefferies
References
- Parveen K, Michael C. Kumar and Clark’s Clinical Medicine. 9 ed. London: Elsevier; 2017
- Netter FH. Atlas of human anatomy. Philadelphia, PA: Elsevier; 2011.74 – 80p
- Lingvay I and Holt S. Textbook of Endocrine Physiology. 5th ed. New York: Oxford Academic; 2011. 311-345p
- Owen K, Turner H, H. WJA. Oxford Handbook of Endocrinology and Diabetes. Oxford: Oxford University Press; 2022
- Hashimoto’s disease. 2021. Available from: [LINK]
- World Health Organization. Iodine deficiency. 2013. Available from: [LINK]
- PIER Network. Management of raised neonatal bloodspot TSH and initial management of congenital hypothyroidism. 2020. Available from: [LINK]
- BMJ Best Practice. Central hypothyroidism. 2023. Available from: [LINK]
- BMJ Best Practice. Subacute thyroiditis. 2023. Available from: [LINK]
- Epp R, Malcolm J, Jolin-Dahel K, Clermont M, Keely E. Postpartum thyroiditis. British Medical Journal Publishing Group; 2021. Available from: [LINK]
- Kavanagh S, Boparai P. Thyroid dysfunction and drug interactions. The Pharmaceutical Journal. 2015. Available from: [LINK]
- Chaker L, Razvi S, Bensenor I et al. Hypothyroidism. Nature Reviews Disease Primers. 2022; 8 (30).
- Fisher D, Wittner L, Gill D. Oxford Clinical Guidelines: Newly qualified doctor. Oxford: Oxford University Press; 2022
- Starr O, Tidy C. Thyroid Function Tests. 2020. Available from: [LINK]
- Fröhlich E, Wahl R. Thyroid autoimmunity: Role of anti-thyroid antibodies in thyroid and extra-thyroidal diseases. Frontiers in Immunology. 2017;8.
- Willacy D. Myxoedema Coma: Causes, symptoms, treatment. Patient Info. 2022. Available from: [LINK]
- Mayer O, Šimon J, Filipovský J, Plášková M, Pikner R. Hypothyroidism in coronary heart disease and its relation to selected risk factors. Vascular Health and Risk Management. 2006;2(4):499–506.
- NICE CKS. Hyperthyroidism: Complications. Available from: [LINK]
Image references
- Figure 1. Geeky Medics.
- Figure 2. Jane Kobylianskii and Wayne L Gold. Queen Anne Sign. License: [CC BY-NC-ND]




