- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
A 50 year old woman visits her GP with worsening tiredness. Work through the case to reach a diagnosis.
UK Medical Licensing Assessment (UKMLA)
This clinical case maps to the following UKMLA presentations:
History
Presenting complaint
“It all started about 3 months ago when I was late to work after sleeping through my alarm clock, despite having had an early night. Since then I’ve been feeling tired most of the time, regardless of how much sleep I have. I’m struggling to make it through a full shift at work and I only work from 9 am-3 pm. Yesterday I fell asleep during my lunch break and the manager told me I need to get checked out by the doctor, so that’s why I’m here. Oh, I’ve also not got much of an appetite.”
History of presenting complaint
Tiredness
- How many hours is she sleeping a day?
- Does she wake frequently when sleeping?
- Did the tiredness come on suddenly or has it gradually gotten worse?
- Does she take any sleep medications/remedies or any other regular medications?
- Has she had problems with sleep or tiredness in general in the past?
For more information, see our guide to tiredness history taking.
Appetite
- When did her appetite change?
- Is her appetite getting worse, better or remaining the same?
- How much is she managing to eat on an average day?
- Does she stop eating because she feels nauseated or just “full” (early satiety)?
- Is she experiencing nausea or vomiting?
- What is her normal bowel habit? Has this changed? Any change to the colour of the stool? Any blood in the stool?
- Has she lost any weight? If so, how much and over what time period?
- Does she have any reflux symptoms or abdominal pain?
Other questions that you could ask in the history of presenting complaint
- Any recent illnesses?
- Any current infective symptoms (e.g. fever, cough, dysuria, diarrhoea)?
- Any contact with others who are unwell or have similar symptoms?
- Any significant psychological stress at present?
- Other symptoms (e.g. polydipsia, polyuria, weight gain, memory impairment, cold intolerance)
Past medical history
- Does the patient have any medical conditions? If so, are they currently managed well?
Menstrual history
- Is the patient pre/post-menopausal?
- If pre-menopausal does she feel her periods are heavy/prolonged?
- Any intermenstrual bleeding?
- If post-menopausal, is the patient experiencing any vaginal bleeding?
Family history
- Any family history of specific medical conditions?
Drug history
- Any regular medication?
- Any over-the-counter medication? (e.g. sleep remedies)
Social history
- Where is the patient currently living?
- Who does the patient live with?
- What is the patient’s occupation?
- Smoking history
- Alcohol history
- Impact of symptoms on activities of daily living
Patient’s response…
“I’ve been sleeping around 14 hours a day, which is far more than the 7 hours I was sleeping a few months ago. It didn’t suddenly switch to 14 hours though, it’s just been gradually increasing over the last few months. I don’t remember waking frequently, I seem to sleep pretty well and I’m not taking any regular medication or anything over the counter.”
“My appetite is generally pretty good, but for the last 4-6 weeks, it’s definitely decreased. I don’t feel particularly nauseated, I just seem to feel full quicker than usual. I might have a piece of toast and then feel like I don’t need anything else for another 6-8 hours, it’s really weird. I haven’t had any vomiting either. My bowels haven’t really changed, I go on average once a day and there’s no blood or anything. My weight has decreased, I’m not sure by how much, but I’ve started wearing a belt with my jeans as they were slipping down. I haven’t noticed any abdominal pain though and certainly no acid reflux type symptoms.”
“I’ve been fairly well otherwise, no recent colds or anything like that. I haven’t had any coughs or burning when passing water. I have woken up feeling quite hot and sweaty on a few occasions. Nobody I’ve been in close contact with has been unwell from my knowledge and psychologically I’m feeling a bit stressed about the sleeping at work, but my mood is generally pretty good. I don’t really have periods as I have a Mirena coil. I haven’t noticed that I’m particularly thirsty or passing more water than usual. Also haven’t noticed any cold intolerance or memory problems.”
“I have some eczema, but no other medical problems and I don’t take any medication. I’ve smoked Marijuana a few times over the last few months, but I don’t take any other drugs.”
“I live with my boyfriend in a flat and I work as a hairdresser. I’ve never smoked and I only drink at weekends, maybe 6-8 units. There’s no illness that runs in my family as far as I’m aware.”
“Well now that you mention it, I have noticed a few weird bruises in random spots where I don’t remember hurting myself, there was one or two last week, but this week there’s about 6.”
Clinical examination
- Gastrointestinal system (given the reduced appetite, weight loss and tiredness)
- Lymphoreticular system (given the history of weight loss, night sweats and early satiety)
- Cardiovascular system (given the history of tiredness, fevers, rigors)
Clinical findings
Inspection
- Conjunctival pallor
- Multiple patches of petechial bruising across the limbs and trunk
Cardio-respiratory assessment
- Pulse – 95 bpm – regular
- Capillary refill time <2
- Heart auscultation – normal heart sounds with no added sounds
- Lungs – good air entry, no crackles or wheezes, resonant on percussion
Gastrointestinal system and lymphoreticular system
- No gross abdominal distension on inspection
- Abdominal palpation:
- The abdomen is soft, with some tenderness in the left upper quadrant
- On deep palpation, you note some fullness in the left upper quadrant
- Lymph nodes – 2 enlarged cervical lymph nodes are noted
Differential diagnoses
- Lymphoma
- Leukaemia
- Infectious mononucleosis – can cause splenomegaly, malaise, weight loss, fever, lethargy (however, the duration is typically shorter than 3 months)
Investigations
- Full blood count (?anaemia, ?thrombocytopenia, ?raised white cells)
- Blood film (?haematological malignancy)
- U&E (?acute kidney injury, ?electrolyte disturbances)
- Coagulation studies (?coagulopathy given the presence of multiple petechiae)
- Random blood glucose (?diabetes)
- Thyroid function (?hypothyroidism)
- EBV Monospot test (?infectious mononucleosis)
Blood test results1
- Hb – 7.9 g/dL (13.5-18.0 g/dL)
- WCC – 250 x 109 (4.0-11.0 x109)
- MCV – 90 fL (76-96 fL)
- Hct – 0.32/L (0.4-0.54/L)
- Neutrophils – 180 x 109/L (2.0-7.5 x 109/L)
- Basophils – 2 x 109/L (0.0-0.10 x109/L)
- Eosinophils – 4 x 109/L (0.04-0.44 x 109/L)
- Myeloblasts – 8.8 x 109/L (usually undetectable)
Urea & electrolytes (U&E)
- Normal
- Platelets – 13 x 109/L (150-400 x109/L)
- PTT – 11 seconds (10-14 s)
- APTT – 37 seconds (35-45 s)
Other tests
- Random blood glucose – 4.8mmol/L
- Thyroid function tests – T3, T4 and TSH normal
- EBV Monospot – negative
Blood film result
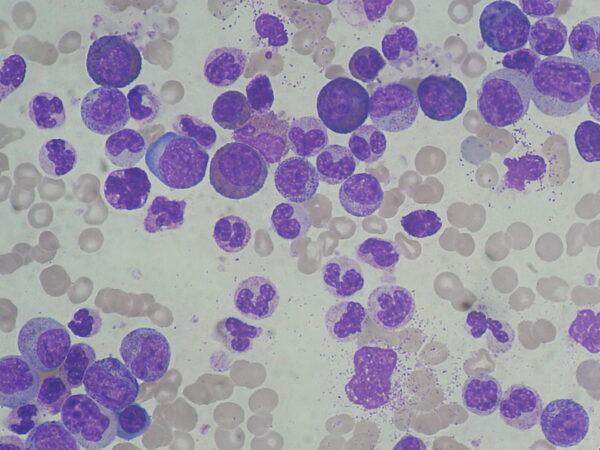
This blood film shows increased numbers of neutrophils, basophils and eosinophils, and immature myeloid cells. Overall this is referred to as leukocytosis.²
Diagnosis
Chronic myeloid leukaemia
Chronic myeloid leukaemia (CML) is a malignancy of white blood cells. It is characterised by increased numbers of myeloid cells in the bone marrow and peripheral blood (leukocytosis). This can cause several signs and symptoms. However, this depends on the degree of leukocytosis.
85-95% of patients are diagnosed incidentally in the chronic stage of the disease via routine blood tests (e.g. FBC). As a result, about 50% of patients are asymptomatic at diagnosis.
Symptoms of CML:
- Fatigue
- Night sweats
- Abdominal fullness and early satiety (due to splenomegaly)
- Low-grade fever
Clinical signs can include:
- Splenomegaly (if it can be palpated, it’s already 3x its normal size)
- Hepatomegaly
- Lymphadenopathy
- Signs of anaemia – conjunctival pallor
- Spontaneous bruising
The overproduction of myeloid cells occurs due to chromosomal translocation (9;22), which produces the characteristic Philadelphia chromosome. When the translocation between chromosomes 9 and 22 occurs, it produces a hybrid gene known as BCR-ABL.
This gene produces substances which activate a cascade of proteins, causing the speed of cell division to increase. In addition, the BCR-ABL gene produces proteins inhibiting DNA repair, making the cell more susceptible to further genetic abnormalities.4
Chronic myeloid leukaemia progresses through 3 stages, as shown below.
Chronic phase
- In this phase, the immune system remains competent, and the patient often has no symptoms.
- The chronic phase typically lasts around 4-5 years.
- Without any treatment, it will eventually progress to the accelerated phase.
Accelerated phase
Around two-thirds of patients will progress to the accelerated phase. This is often when patients become symptomatic (as in this case).
Features of the accelerated phase involve:
- ↑ Blasts in the bone marrow and peripheral blood
- ↑ Basophils and eosinophils in the bone marrow and peripheral blood
- Worsening anaemia
- Thrombocytopenia
- Increasing splenomegaly
- Additional genetic mutations in haematopoietic stem cells
Blast crisis
- Large numbers of blasts in peripheral blood and bone marrow (>30%)
- Severe weight loss
- Fever, night sweats, bone pain
- Infection (due to an incompetent immune system)
- Bleeding (due to lack of platelet production)
- Foci of blasts cause local tissue destruction
Cytogenetic testing of bone marrow aspirate for the Philadelphia chromosome.
The testing for the chromosome can be done via various methods:
- FISH (fluorescent in-situ hybridisation)
- PCR for the BCR-ABL gene
Management
BCR-ABL tyrosine kinase inhibitors (TKIs)
There are multiple TKIs available for first-line treatment to allow switching if resistance occurs to one particular agent. Treatment is usually continued indefinitely in patients who respond well to treatment.
Some examples of TKIs are:
- Imatinib
- Nilotinib
- Dasatinib
High levels of relapse have been observed in patients who stop therapy.5
TKIs specifically target BCR-ABL, blocking the ability of the gene to phosphorylate a tyrosine. As a result, TKIs inhibit the proliferation of cells and induces apoptosis in cells with the BCR-ABL fusion gene. It is better tolerated and more effective than previous therapies due to its specificity to the exact pathway responsible for CML.
Stem cell transplantation
Stem cell transplantation is a treatment option for those who do not respond well to drug treatments. This tends only to be used in younger, otherwise healthy patients. It does offer the possibility of a cure, however, there are significant risks involved, therefore it is often kept as a last resort.
Prognosis
TKIs have revolutionised CML treatment and now the 5-year survival for those treated is around 90%.³
References
- East Sussex Healthcare – Laboratory. Available from: [LINK]
- Paulo Henrique Orlandi Mourao. License: [CC BY-SA]
- Druker BJ, Guilhot F, O’Brien SG et al. (2006). “Five-Year Follow-up of Patients Receiving Imatinib for Chronic Myeloid Leukemia”. New England Journal of Medicine 355 (20): 2408–17
- Hehlmann R, Hochhaus A, Baccarani M; European LeukemiaNet (2007). “Chronic myeloid leukaemia”. Lancet 370 (9584): 342–50.
- Baccarani M, Cortes J, Pane F, et al; Chronic Myeloid Leukemia: An Update of Concepts and Management Recommendations of J Clin Oncol. 2009 Nov 2. [abstract]




