- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
The ABCDE approach is used to systematically assess an acutely unwell patient. It involves working through the following steps:
- Airway
- Breathing
- Circulation
- Disability
- Exposure
Each stage of the ABCDE approach involves clinical assessment, investigations and interventions. Problems are addressed as they are identified, and the patient is re-assessed regularly to monitor their response to treatment.
The ABCDE approach aims to improve the clinical outcome of unwell patients, regardless of the definitive diagnosis. It is not a substitute for formally examining a specific system you are concerned about. It can help you identify life-threatening problems and structure your response in a real clinical setting.
This guide provides a general guide to the ABCDE approach and can be used for any unwell patient in a simulation setting. It may seem intimidating initially, but your patient will unlikely need all of the investigations or interventions mentioned in this guide.
This guide has been created to assist healthcare students in preparing for emergency simulation sessions as part of their training. It is not intended to be relied upon for patient care.
Tips before you begin
General tips for applying an ABCDE approach in an emergency setting include:
- Treat problems as you discover them and re-assess after every intervention
- Remember to assess the front and back of the patient when carrying out your assessment (e.g. looking underneath the patient’s legs or at their back for non-blanching rashes or bleeding)
- If the patient loses consciousness and there are no signs of life, put out a crash call and commence CPR
- Make use of the team around you by delegating tasks where appropriate
- All critically unwell patients should have continuous monitoring equipment attached
- If you require senior input, call for help early using an appropriate SBAR handover
- Review results as they become available (e.g. laboratory investigations)
- Use local guidelines and algorithms to manage specific scenarios (e.g. acute asthma)
- Any medications or fluids must be prescribed at the time (you may be able to delegate this to another staff member)
- Your assessment and management should be documented clearly in the notes; however, this should not delay management
Methodical approach
For each section of the ABCDE assessment (e.g. airway, breathing, circulation etc.), ask yourself:
- Have I checked the relevant observations for this section? (e.g. checking respiratory rate and SpO2 as part of your ‘breathing’ assessment)
- Have I examined the relevant parts of the system in this section? (e.g. peripheral perfusion, pulses, JVP, heart sounds, and peripheral oedema as part of your ‘circulation’ assessment)
- Have I requested relevant investigations based on my findings from the initial clinical assessment? (e.g. capillary blood glucose as part of your ‘disability’ assessment)
- Have I intervened to correct the issues I have identified? (e.g. administering IV fluids in response to fluid depletion/hypotension as part of your ‘circulation’ assessment)
Initial steps
Acute scenarios typically begin with a brief handover, including the patient’s name, age, background and the reason the review has been requested.
Introduction
Introduce yourself to whoever has requested a review of the patient and listen carefully to their handover.
Preparation
Ensure the patient’s notes, observation chart, and prescription chart are easily accessible.
Ask for another clinical member of staff to assist you if possible.
Interaction
Introduce yourself to the patient, including your name and role.
Ask how the patient is feeling, as this may provide useful information about their condition.
If the patient is unconscious or unresponsive, and there are no signs of life, start the basic life support (BLS) algorithm as per resuscitation guidelines.
Airway
Clinical assessment
Can the patient talk?
Yes: if the patient can talk, their airway is patent, and you can move on to the assessment of breathing.
No:
- Look for signs of airway compromise: angioedema, cyanosis, see-saw breathing, use of accessory muscles
- Listen for abnormal airway noises: stridor, snoring, gurgling
- Open the mouth and inspect: look for anything obstructing the airway, such as secretions or a foreign object
Causes of airway compromise
Causes of airway compromise include:
- Inhaled foreign body
- Blood in the airway: epistaxis, haematemesis and trauma
- Vomit/secretions in the airway: alcohol intoxication, head trauma and dysphagia
- Soft tissue swelling: anaphylaxis and infection (e.g. quinsy, sub-mandibular gland swelling)
- Local mass effect: tumours and lymphadenopathy (e.g. lymphoma)
- Laryngospasm: asthma, gastro-oesophageal reflux disease (GORD) and intubation
- Depressed level of consciousness: opioid overdose, head injury and stroke
Interventions
Regardless of the underlying cause of airway obstruction, seek immediate expert support from an anaesthetist and the emergency medical team (often called the ‘crash team’). You can perform basic airway manoeuvres to help maintain the airway whilst awaiting senior input.
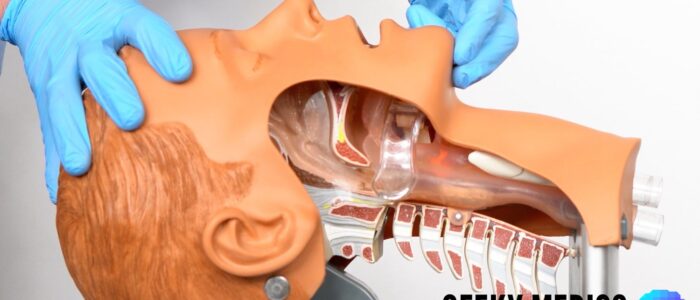
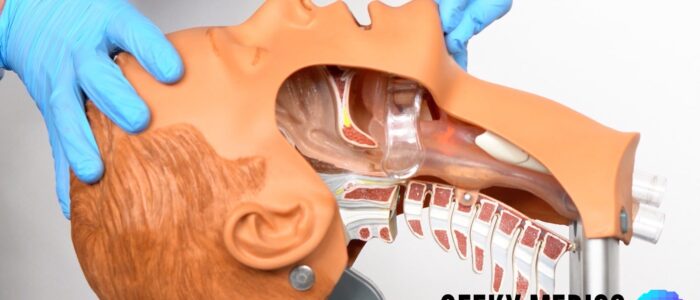
Head-tilt chin-lift manoeuvre
Open the patient’s airway using a head-tilt chin-lift manoeuvre:
- Place one hand on the patient’s forehead and the other under the chin
- Tilt the forehead back whilst lifting the chin forwards to extend the neck
- Inspect the airway for obvious obstruction. If an obstruction is visible within the airway, use a finger sweep or suction to try and remove it. Be careful not to push it further into the airway.
Jaw thrust
If the patient is suspected of having suffered significant trauma with potential spinal involvement, perform a jaw-thrust rather than a head-tilt chin-lift manoeuvre:
- Identify the angle of the mandible
- Place two fingers under the angle of the mandible (on both sides) and anchor your thumbs on the patient’s cheeks
- Lift the mandible forwards
Other interventions
Airway adjuncts are helpful and, in some cases, essential to maintain a patient’s airway. They should be used in conjunction with the manoeuvres mentioned above.
An oropharyngeal airway is a curved plastic tube with a flange on one end that sits between the tongue and hard palate to relieve soft palate obstruction. It should only be inserted in unconscious patients as it may induce gagging and aspiration in semi-conscious patients.
A nasopharyngeal airway is a soft plastic tube with a bevel at one end and a flange at the other. NPAs are typically better tolerated in partly or fully conscious patients than oropharyngeal airways.
Specific airway interventions
If a specific cause of airway compromise is identified, it should be rapidly treated:
- Anaphylaxis: intramuscular adrenaline
- Blood, vomit or secretions in the airway: suction, patient positioning (left lateral position)
- Stridor: sit the patient upright, urgent anaesthetic/ENT input
- Foreign body: basic life support choking algorithm
Re-assessment
Re-assess the patient after any intervention.
Breathing
Clinical assessment
Observations
Review the patient’s respiratory rate:
- A normal respiratory rate is between 12-20 breaths per minute
- Bradypnoea may be due to sedation, opioid toxicity, raised intracranial pressure (ICP) or exhaustion in airway obstruction with CO2 retention/narcosis (e.g. COPD)
- Tachypnoea may be due to airway obstruction, asthma, pneumonia, pulmonary embolism (PE), pneumothorax, pulmonary oedema, heart failure, or anxiety
Review the patient’s oxygen saturation (SpO2):
- A normal SpO2 range is 94-98% in healthy individuals and 88-92% in patients with COPD at high risk of CO2 retention
- Hypoxaemia may be seen in PE, aspiration, COPD, asthma and pulmonary oedema
See our guide to performing observations/vital signs for more details.
General inspection
Inspect the patient whilst at rest, looking for clinical signs suggestive of underlying pathology:
- Cyanosis: bluish skin discolouration due to poor circulation (e.g. peripheral vasoconstriction secondary to hypovolaemia) or inadequate oxygenation (e.g. right-to-left cardiac shunting).
- Shortness of breath: signs may include nasal flaring, pursed lips, use of accessory muscles, intercostal muscle recession and the tripod position, which involves the patient sitting or standing whilst leaning forward and supporting their upper body with their hands on their knees or other surfaces. The inability to speak in full sentences indicates significant shortness of breath.
- Cough: a productive cough can be associated with several respiratory pathologies, including pneumonia, bronchiectasis, COPD and cystic fibrosis. A dry cough may suggest a diagnosis of asthma or interstitial lung disease.
- Stridor: a high-pitched extra-thoracic breath sound resulting from turbulent airflow through narrowed upper airways. Stridor has a variety of causes, including foreign body inhalation (acute) and subglottic stenosis (chronic).
- Cheyne-Stokes respiration: cyclical apnoeas, with varying depth of inspiration and rate of breathing. It may be caused by stroke, raised intracranial pressure, pulmonary oedema, opioid toxicity, hyponatraemia or carbon monoxide poisoning.
- Kussmaul’s respiration: deep, sighing respiration associated with metabolic acidosis (e.g. diabetic ketoacidosis).
Tracheal position
Gently assess the position of the trachea, which should be central in healthy individuals:
- The trachea deviates away from tension pneumothorax and large pleural effusions
- The trachea deviates towards lobar collapse and pneumonectomy
Palpation of the trachea can be uncomfortable, so warn the patient and be gentle.
Chest expansion
Assess the patient’s chest expansion looking for evidence of reduced chest wall movement. Reduced chest expansion may indicate underlying pathology:
- Symmetrical: pulmonary fibrosis reduces lung elasticity, restricting overall chest expansion
- Asymmetrical: pneumothorax, pneumonia, and pleural effusion can all cause ipsilateral reduced chest expansion
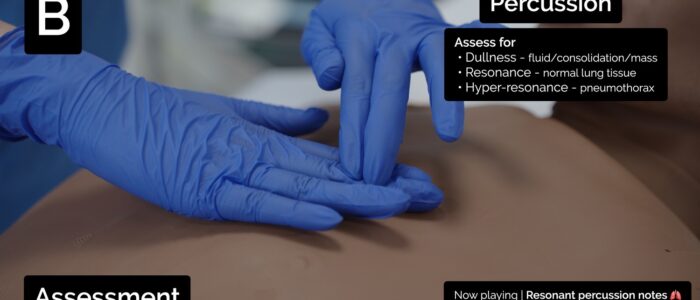
Percussion of the chest
Percuss the patient’s chest, listening to the resulting percussion note, which should be resonant in healthy individuals. Abnormal findings on percussion include:
- Dullness: suggests increased tissue density (e.g. cardiac dullness, consolidation, tumour, lobar collapse)
- Stony dullness: typically caused by an underlying pleural effusion
- Hyper-resonance: the opposite of dullness, suggestive of decreased tissue density (e.g. pneumothorax)
Auscultation
Auscultate the patient’s chest and identify any abnormalities such as:
- Bronchial breathing: harsh-sounding (similar to auscultating over the trachea), inspiration and expiration are equal, and there is a pause between. This type of breath sound is associated with consolidation.
- Quiet/reduced breath sounds: suggest reduced air entry into that lung region (e.g. pleural effusion, pneumothorax).
- Wheeze: a continuous, coarse, whistling sound produced in the respiratory airways during breathing. Wheeze is often associated with asthma, COPD and bronchiectasis.
- Coarse crackles: discontinuous, brief, popping lung sounds typically associated with pneumonia, bronchiectasis and pulmonary oedema.
- Fine end-inspiratory crackles: often described as sounding similar to the noise generated when separating velcro. Fine end-inspiratory crackles are associated with pulmonary fibrosis.
See our respiratory examination guide for more details.
Investigations and procedures
Arterial blood gas (ABG)
Take an ABG if indicated (e.g. low SpO2) to quantify the degree of hypoxia and help determine the potential underlying cause.
See our guides for taking and interpreting an ABG for more details.
Chest X-ray
Order a portable chest X-ray if you suspect lung pathology (e.g. pneumonia, pneumothorax, pulmonary oedema).
See our chest X-ray interpretation guide for more details.
Interventions
Patient positioning
If the patient is conscious, sit them upright, which can help with oxygenation.
Oxygen
Administer oxygen to all critically unwell patients during your initial assessment. This typically involves using a non-rebreathe mask with an oxygen flow rate of 15L. You can then trial titrating oxygen levels downwards after your initial assessment.
In COPD, target SpO2 levels accordingly (88-92%) and consider using a venturi mask: 24% (4L) or 28% (4L). Consider discussing non-invasive ventilation (NIV) with a senior in acute exacerbations of COPD where there is evidence of type 2 respiratory failure.
See our guide to oxygen administration and non-invasive ventilation for more details.
Specific breathing interventions
If a specific cause of breathing difficulties is identified, it should be rapidly treated:
- Acute asthma: nebulised bronchodilators (salbutamol/ipratropium), corticosteroids and other agents (e.g. magnesium sulphate, aminophylline)
- Exacerbation of COPD: bronchodilators (salbutamol/ipratropium), corticosteroids, antibiotics (if evidence of infection)
- Pneumothorax: management as per British Thoracic Society guidelines
- Pneumonia: antibiotics
Re-assessment
Re-assess the patient after any intervention.
Circulation
Clinical assessment
Observations
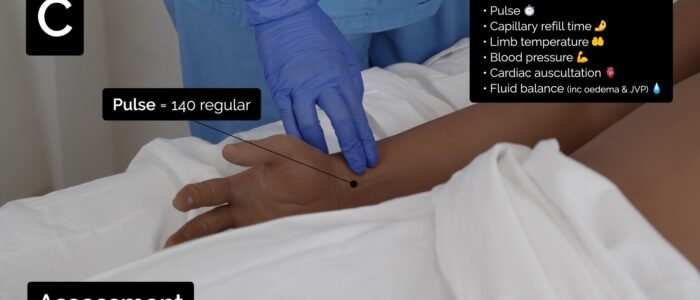
Review the patient’s heart rate:
- A normal resting heart rate (HR) can range between 60-99 beats per minute
- Causes of tachycardia (HR>99) include hypovolaemia, arrhythmia, infection, hypoglycaemia, thyrotoxicosis, anxiety, pain and drugs (e.g. salbutamol)
- Causes of bradycardia (HR<60) include acute coronary syndrome (ACS), ischaemic heart disease, electrolyte abnormalities (e.g. hypokalaemia) and drugs (e.g. beta-blockers)
Review the patient’s blood pressure:
- A normal blood pressure (BP) range is between 90/60mmHg and 140/90mmHg, but you should review previous readings to gauge the patient’s usual baseline BP
- Causes of hypertension include hypervolaemia, stroke, Conn’s syndrome, Cushing’s syndrome and pre-eclampsia (in pregnant females). Severe hypertension (systolic BP > 180 mmHg or diastolic BP > 100 mmHg) may present with confusion, drowsiness, breathlessness, chest pain and visual disturbances.
- Causes of hypotension include hypovolaemia, sepsis, adrenal crisis and drugs (e.g. opioids, antihypertensives, diuretics).
Extremes of heart rate or blood pressure, combined with other concerning features (e.g., syncope, pre-syncope, shortness of breath or evidence of myocardial ischaemia), require urgent senior and/or critical care input.
See our guide to performing observations/vital signs for more details.
Fluid balance assessment
Calculate the patient’s fluid balance:
- Calculate the patient’s current fluid balance using their fluid balance chart (e.g. oral fluids, intravenous fluids, urine output, drain output, stool output, vomiting) to inform resuscitation efforts
- Reduced urine output (oliguria) is typically defined as less than 0.5ml/kg/hour in an adult
- Causes of oliguria include dehydration, hypovolaemia, reduced cardiac output and acute kidney injury
General inspection
Inspect the patient from the end of the bed whilst at rest, looking for clinical signs suggestive of underlying pathology:
- Pallor: can suggest underlying anaemia (e.g. haemorrhage, chronic disease) or poor perfusion (e.g. congestive cardiac failure)
- Oedema: typically presents with swelling of the limbs (e.g. pedal oedema) or abdomen (ascites) and may indicate underlying heart failure
Palpation
Place the dorsal aspect of your hand onto the patient’s to assess temperature:
- The hands should be symmetrically warm in healthy individuals, indicating adequate perfusion
- Cool hands indicate poor peripheral perfusion (e.g. congestive cardiac failure, acute coronary syndrome)
- Cool and sweaty/clammy hands indicate poor peripheral perfusion and autonomic dysfunction (e.g. acute coronary syndrome)
Measure capillary refill time (CRT):
- Check this centrally on the sternum and compare it with a peripheral CRT on the fingertip
- In healthy individuals, the initial pallor of the area you compressed should return to its normal colour in less than two seconds
- A peripheral CRT greater than two seconds suggests poor peripheral perfusion (e.g. hypovolaemia, congestive heart failure) and the need to assess central CRT
Pulses and blood pressure
Assess the patient’s radial and brachial pulse to assess rate, rhythm, volume and character:
- An irregular pulse is associated with arrhythmias such as atrial fibrillation
- A slow-rising pulse is associated with aortic stenosis
- A pounding pulse is associated with aortic regurgitation as well as CO2 retention
A thready pulse is associated with intravascular hypovolaemia (e.g. sepsis).
Jugular venous pressure (JVP)
Briefly inspect for a significantly raised JVP, which may be caused by:
- Right-sided heart failure: commonly caused by left-sided heart failure (e.g. secondary to fluid overload). Pulmonary hypertension is another cause of right-sided heart failure, often due to chronic obstructive pulmonary disease or interstitial lung disease.
- Tricuspid regurgitation: causes include infective endocarditis and rheumatic heart disease.
- Constrictive pericarditis: often idiopathic, but rheumatoid arthritis and tuberculosis are also possible underlying causes.
Auscultation
In an acute situation, cardiac auscultation should be brief and focused on identifying acute cardiovascular conditions:
- A pericardial rub or muffled heart sounds may indicate underlying pericarditis or cardiac tamponade
- A third heart sound is typically associated with congestive heart failure
- A murmur of recent onset may suggest recent myocardial infarction (e.g. papillary muscle rupture) or endocarditis
Ankles and sacrum
Assess the patient’s ankles and sacrum for evidence of oedema, which is typically associated with heart failure.
Investigations and procedures
Intravenous cannulation
Insert at least one wide-bore intravenous cannula (14G or 16G) and take blood tests as discussed below.
See our intravenous cannulation guide for more details.
Blood tests and blood cultures
Request a full blood count (FBC), urea & electrolytes (U&E) and liver function tests (LFTs) for all acutely unwell patients and consider additional blood tests in these situations:
- Sepsis: CRP, lactate and blood cultures
- Haemorrhage or surgical emergency: coagulation and cross-match
- Acute coronary syndrome: troponin
- Arrhythmia: calcium, magnesium, phosphate, thyroid function tests, coagulation
- Pulmonary embolism: D-dimer (if appropriate based on Well’s score)
- Overdose: toxicology screen (e.g. paracetamol levels)
- Anaphylaxis: consider serial mast cell tryptase levels
For more information, see our blood culture and blood bottle guides.
ECG
Record a 12-lead ECG if appropriate (e.g. chest pain, arrhythmia, a murmur, or suspected electrolyte imbalance).
Consider continuous cardiac monitoring for critically unwell patients (e.g. myocardial infarction, severe electrolyte abnormalities requiring replacement).
See our guides to recording and interpreting an ECG for more details.
Bladder scan
Perform a bladder scan in suspected urinary retention or obstruction.
Urine pregnancy test
Perform a urine pregnancy test in any female of childbearing age presenting with clinical evidence of shock, abdominal pain or gynaecological symptoms.
Other cultures/swabs
Ask the nursing staff to collect and send other appropriate cultures (e.g. sputum, urine, line cultures).
Fluid output/catheterisation
Ask the nursing staff to initiate a strict fluid balance if not already in place.
Consider catheterisation to allow accurate monitoring of urine output or to relieve urinary retention where appropriate.
See our guide to catheterisation for more details.
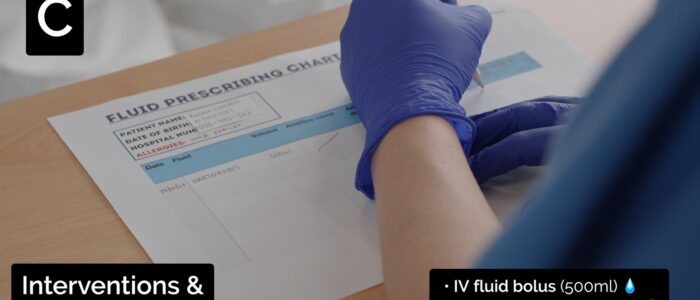
Interventions
Fluid resuscitation
Hypovolaemic patients require fluid resuscitation (the below guidelines are for adults):
- Administer a 500ml bolus of Hartmann’s solution or 0.9% sodium chloride (warmed if available) over less than 15 mins.
- Administer 250ml boluses in patients at increased risk of fluid overload (e.g. heart failure).
After each fluid bolus, reassess for clinical evidence of fluid overload (e.g. auscultation of the lungs, assessment of JVP).
Repeat administration of fluid boluses up to four times (e.g. 2000ml or 1000ml in patients at increased risk of fluid overload), reassessing the patient each time.
Seek senior input if the patient has a negative response (e.g. increased chest crackles) or isn’t responding adequately to repeated boluses (e.g. persistent hypotension).
See our fluid prescribing guide for more details on resuscitation fluids.
Blood transfusion
Patients with a significant haemorrhage who are in shock need a balanced transfusion of red cells, platelets and fresh frozen plasma.
This is usually arranged via a massive transfusion protocol which simplifies the ordering and administration of large amounts of blood products (usually at least six units of red cells).
See our post-operative bleeding guide and major trauma guide for more details.
Specific circulation interventions
If a specific cause of circulatory compromise is identified, it should be rapidly treated:
- External haemorrhage: direct pressure
- Acute coronary syndrome: analgesia (morphine), nitrates, aspirin, antiplatelets (e.g. clopidogrel) and oxygen if required
- Sepsis: sepsis six (alert senior clinician, oxygen if required, blood cultures and lactate, IV antibiotics, IV fluids, and ongoing monitoring)
- Fluid overload: diuretics, close fluid balance monitoring
- Atrial fibrillation: treatment of underlying trigger, consideration of rate vs rhythm control
- Pulmonary embolism (unstable): alert senior clinician for consideration of systemic thrombolysis
Re-assessment
Re-assess the patient after any intervention.
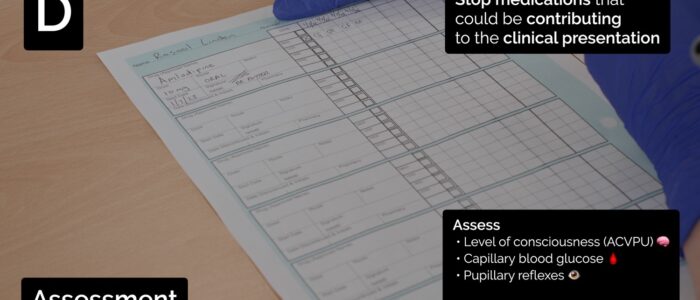
Disability
Clinical assessment
Consciousness
Assess the patient’s level of consciousness using the ACVPU scale:
- Alert: the patient is fully alert
- Confusion: the patient has new onset confusion or worse confusion than usual
- Verbal: the patient makes some kind of response when you talk to them (e.g. words, grunt)
- Pain: the patient responds to a painful stimulus (e.g. supraorbital pressure)
- Unresponsive: the patient does not show evidence of any eye, voice or motor responses to pain
If a more detailed assessment of the patient’s level of consciousness is required, use the Glasgow Coma Scale (GCS).
Causes of depressed consciousness
Causes of depressed consciousness include:
- Hypovolaemia
- Hypoxia
- Hypercapnia
- Metabolic disturbance (e.g. hypoglycaemia)
- Seizure
- Raised intracranial pressure or other neurological insults (e.g. stroke)
- Drug overdose
- Iatrogenic causes (e.g. administration of opiates)
Pupils
Assess the patient’s pupils:
- Inspect the size and symmetry of the patient’s pupils (e.g. pinpoint pupils in opioid overdose, dilated pupils in tricyclic antidepressant overdose). Asymmetrical pupillary size may indicate intracerebral pathology (e.g. stroke, space-occupying lesion, raised intracranial pressure).
- Assess direct and consensual pupillary responses which may reveal evidence of intracranial pathology (e.g. stroke).
Brief neurological assessment
Perform a brief neurological assessment by asking the patient to move their limbs.
If a patient cannot move one or all of their limbs, this may be a sign of focal neurological impairment, which requires a more detailed assessment.
Drug chart review
Review the patient’s drug chart for medications which may cause neurological abnormalities (e.g. opioids, sedatives, anxiolytics).
Investigations and procedures
Blood glucose and ketones
Measure the patient’s capillary blood glucose level to screen for abnormalities (e.g. hypoglycaemia or hyperglycaemia).
A blood glucose level may already be available from earlier investigations (e.g. ABG, venepuncture).
The normal reference range for fasting plasma glucose is 4.0 – 5.8 mmol/l.
Hypoglycaemia is defined as a plasma glucose of less than 3.0 mmol/l. In hospitalised patients, a blood glucose ≤4.0 mmol/L should be treated if the patient is symptomatic.
If the blood glucose is elevated, check ketone levels which, if also elevated, may suggest a diagnosis of diabetic ketoacidosis (DKA).
See our blood glucose measurement, hypoglycaemia and diabetic ketoacidosis guides for more details.
Imaging
Request a CT head if intracranial pathology is suspected after discussion with a senior.
See our guide on interpreting a CT head for more details.
Interventions
Maintain the airway
Alert a senior clinician immediately if you have concerns about a patient’s consciousness level.
A GCS of 8 or below, or a P or U on the ACVPU scale, warrants urgent expert help from an anaesthetist. In the meantime, you should re-assess and maintain the patient’s airway, as explained in the airway section of this guide.
Correct hypoglycaemia
Hypoglycaemia should always be considered in patients presenting with a reduced level of consciousness, regardless of whether they have diabetes. The management of hypoglycaemia involves the administration of glucose (e.g. oral or intravenous).
See our hypoglycaemia guide for more details.
Specific disability interventions
If a specific cause of reduced consciousness is identified, it should be rapidly treated:
- Opioid overdose: ventilation, naloxone
- Diabetic ketoacidosis (DKA): intravenous fluids and insulin
- Seizures: maintain airway, benzodiazepines
- Hypercapnia: urgent senior clinician review for consideration of ventilation
Re-assessment
Re-assess the patient after any intervention.
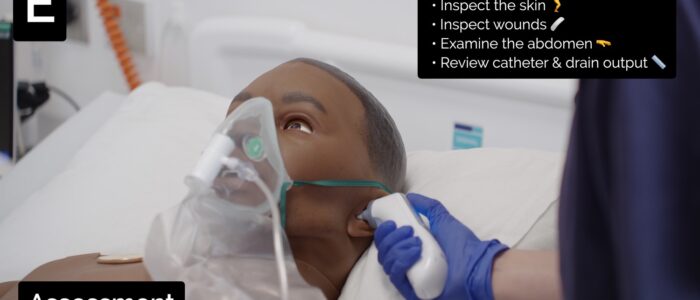
Exposure
Exposing the patient during your assessment may be necessary. Remember to prioritise patient dignity and the conservation of body heat.
Clinical assessment
Begin by asking the patient if they have pain anywhere, which may be helpful to guide your assessment.
Inspection
Inspect the patient’s skin for evidence of rashes (e.g. adverse drug reaction, meningococcal sepsis), bruising (e.g. coagulation disorders, trauma, surgery) and signs of infection (e.g. cellulitis).
Review any in situ intravenous lines for evidence of surrounding erythema or discharge.
Expose and inspect the patient’s abdomen for signs of abdominal distension and swelling (e.g. hernias).
Inspect the patient’s calves for erythema or swelling, which may suggest a deep vein thrombosis.
Review any surgical wounds for evidence of haematoma, active bleeding or infection (e.g. purulent discharge).
Review the output of the patient’s catheter and any surgical drains for blood loss, fluid loss and evidence of infection (e.g. pus).
Palpation
Briefly palpate the abdomen for signs of peritonism or other life-threatening pathology (e.g. abdominal aortic aneurysm).
Palpate the calves for tenderness which may suggest a deep vein thrombosis.
Temperature
Review the patient’s body temperature:
- A normal body temperature range is between 36°c – 37.9°c
- A temperature of >38°c is most commonly caused by infection (e.g. sepsis)
- A temperature <36°c may also be caused by sepsis or cold exposure (e.g. drowning, inadequate clothing outside)
Investigations and procedures
Cultures/swabs
Ask the nursing staff to take relevant swabs/samples of any potential infection source (e.g. line tip culture).
Interventions
Control bleeding
If active bleeding, which was not identified earlier, is found:
- Take steps to control the blood loss (if possible)
- Estimate the total blood loss and the rate of blood loss
- Re-assess for signs of hypovolaemic shock (e.g. hypotension, tachycardia, pre-syncope, syncope) and act accordingly (see circulation section)
Warm the patient
In hypothermic patients, apply blankets and seek senior advice to consider active warming (e.g. warmed fluids, Bair Hugger™).
Treat infection
If an infection is suspected (e.g. a surgical wound is leaking pus), re-assess the patient for clinical evidence of sepsis and perform the sepsis six if appropriate.
Consult local guidelines and/or microbiology advice to guide appropriate antibiotic treatment.
See our sepsis guide for more details.
Re-assessment
Re-assess the patient after any intervention.
Re-assessment and escalation
Re-assess the patient using the ABCDE approach to identify any changes in their clinical condition and assess the effectiveness of your previous interventions.
Any clinical deterioration should be recognised quickly and acted upon immediately.
Seek senior help if the patient shows no signs of improvement or if you have any concerns.
Escalation
You may need further help or advice from a senior clinician or a specialist team, and you should not delay seeking help if you have concerns about your patient.
Use an effective SBAR handover to communicate the key information to other medical staff.
Important teams to contact
If a patient is critically unwell (e.g. peri-arrest, cardiac arrest), the cardiac arrest team should be alerted (the team typically consists of an anaesthetist, medical registrar and other clinicians).
Airway problems
- Anaesthetics +/- ENT
Breathing problems
- Medical registrar on call
- Critical care team
Circulation problems
- Medical registrar on call
- Critical care team
- Other specialists depending on the suspected pathology (e.g. microbiologist, cardiologist, surgeon, gastroenterologist)
Disability problems
- Medical registrar on call
- Anaesthetics if the airway is threatened (e.g. GCS<8)
- Other specialists depending on the suspected pathology (e.g. neurosurgeon, endocrinologist, neurologist)
Exposure problems
- Medical registrar on call
- Other specialists depending on the suspected pathology (e.g. surgeon, dermatologist, microbiologist)
Next steps
Take a history
Take a thorough history to help narrow down the differential diagnoses.
See our history taking guides for more details.
Examine relevant body systems
Perform an in-depth clinical examination of the system or systems you feel contribute to the patient being acutely unwell.
Review medical records
Review the patient’s notes, charts and recent investigation results.
Review the patient’s current medications and check any regular medications are prescribed appropriately.
Discuss
Discuss the patient’s clinical condition with a senior clinician using an SBAR handover.
Questions which may need to be considered include:
- Are any further assessments or interventions required?
- Does the patient need a referral to HDU/ICU?
- Does the patient need reviewing by a specialist?
- Should any changes be made to the current management of their underlying condition(s)?
The next team of clinicians on shift should be informed of any acutely unwell patient.
Document
Document your ABCDE assessment, including history, examination, observations, investigations, interventions, and the patient’s response.
The ABCDE approach can also form the structure for documenting your assessment.
See our documentation guides for more details.
Reviewer
Dr James McFetrich
Emergency Medicine Consultant
Editor
Dr Chris Jefferies
References
- Resuscitation Council (UK). ABCDE Approach. Available from: [LINK].
- Resuscitation Council (UK). Peri-arrest arrhythmias. Available from: [LINK].