- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Abdominal examination frequently appears in OSCEs and you’ll be expected to pick up the relevant clinical signs using your examination skills. This abdominal examination OSCE guide provides a clear step-by-step approach to examining the gastrointestinal system, with an included video demonstration.
Introduction
Wash your hands and don PPE if appropriate.
Introduce yourself to the patient including your name and role.
Confirm the patient’s name and date of birth.
Briefly explain what the examination will involve using patient-friendly language.
Gain consent to proceed with the examination.
Adjust the head of the bed to a 45° angle and ask the patient to lay on the bed.
Adequately expose the patient’s abdomen for the examination from the waist up (offer a blanket to allow exposure only when required and if appropriate, inform patients they do not need to remove their bra). Exposure of the patient’s lower legs is also helpful to assess for peripheral oedema.
Ask the patient if they have any pain before proceeding with the clinical examination.
General inspection
Clinical signs
Inspect the patient from the end of the bed whilst at rest, looking for clinical signs suggestive of underlying pathology:
- Age: the patient’s approximate age is helpful when considering the most likely underlying pathology, with younger patients more likely to have diagnoses such as inflammatory bowel disease (IBD) and older patients more likely to have chronic liver disease and malignancy.
- Confusion: often a feature of end-stage liver disease, known as hepatic encephalopathy.
- Pain: if the patient appears uncomfortable, ask where the pain is and whether they are still happy for you to examine them.
- Obvious scars: may provide clues regarding previous abdominal surgery.
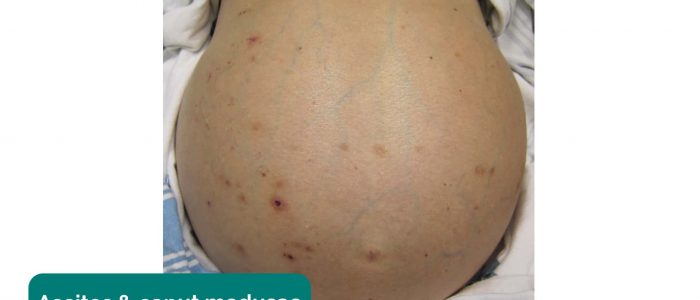
- Abdominal distention: may suggest the presence of ascites or underlying bowel obstruction and/or organomegaly.
- Pallor: a pale colour of the skin that can suggest underlying anaemia (e.g. gastrointestinal bleeding or malnutrition). It should be noted that healthy individuals may have a pale complexion that mimics pallor.
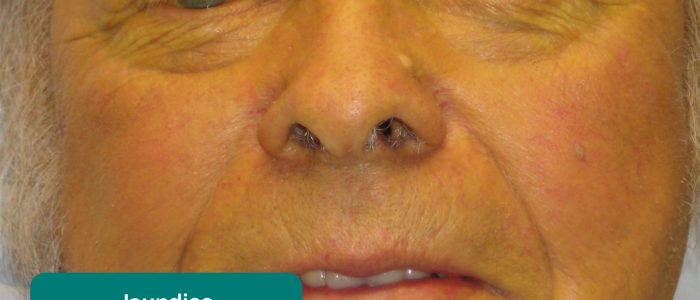
- Jaundice: a yellowish or greenish pigmentation of the skin and whites of the eyes due to high bilirubin levels (e.g. acute hepatitis, liver cirrhosis, cholangitis, pancreatic cancer).
- Hyperpigmentation: a bronzing of the skin associated with haemochromatosis.
- Oedema: typically presents as swelling of the limbs (e.g. pedal oedema) or abdomen (i.e. ascites) and is often associated with liver cirrhosis in the context of an abdominal examination OSCE station.
- Cachexia: ongoing muscle loss that is not entirely reversed with nutritional supplementation. Cachexia is commonly associated with underlying malignancy (e.g. pancreatic/bowel/stomach cancer) and advanced liver failure.
- Hernias: may be visible from the end of the bed (e.g. umbilical/incisional hernia). Asking the patient to cough will usually cause hernias to become more pronounced.
Objects and equipment
Look for objects or equipment on or around the patient that may provide useful insights into their medical history and current clinical status:
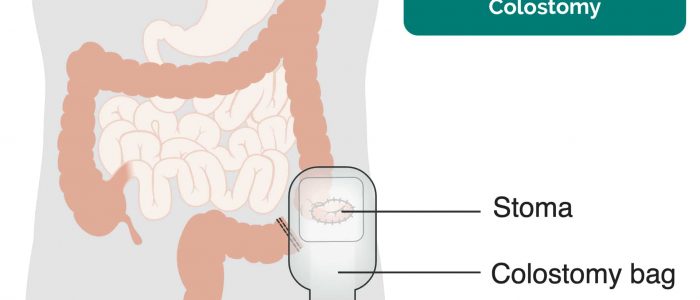
- Stoma bag(s): note the location of the stoma bag(s) as this can provide clues as to the type of stoma (e.g. colostomies are typically located in the left iliac fossa, whereas ileostomies are usually located in the right iliac fossa).
- Surgical drains: note the location of the drain and the type/volume of the contents within the drain (e.g. blood, chyle, pus).
- Feeding tubes: note the presence of feeding tubes (e.g. nasogastric/nasojejunal) and whether the patient is currently being fed.
- Other medical equipment: ECG leads, medications, total parenteral nutrition, catheters (note volume/colour of urine) and intravenous access.
- Mobility aids: items such as wheelchairs and walking aids give an indication of the patient’s current mobility status.
- Vital signs: charts on which vital signs are recorded will give an indication of the patient’s current clinical status and how their physiological parameters have changed over time.
- Fluid balance: fluid balance charts will give an indication of the patient’s current fluid status which may be relevant if a patient appears fluid overloaded or dehydrated.
- Prescriptions: prescribing charts or personal prescriptions can provide useful information about the patient’s recent medications.
Hands
The hands can provide lots of clinically relevant information and therefore a focused, structured assessment is essential.
Inspection
Palms
Inspect the palms for any of the following signs:
- Pallor: may suggest underlying anaemia (e.g. malignancy, gastrointestinal bleeding, malnutrition).
- Palmar erythema: a redness involving the heel of the palm that can be associated with chronic liver disease (it can also be a normal finding in pregnancy).
- Dupuytren’s contracture (see more details in the palpation section).
Nail signs
Inspect the nails for any of the following signs:
- Koilonychia: spoon-shaped nails, associated with iron deficiency anaemia (e.g. malabsorption in Crohn’s disease).
- Leukonychia: whitening of the nail bed, associated with hypoalbuminaemia (e.g. end-stage liver disease, protein-losing enteropathy).
Finger clubbing
Finger clubbing involves uniform soft tissue swelling of the terminal phalanx of a digit with subsequent loss of the normal angle between the nail and the nail bed. Finger clubbing is associated with several underlying disease processes, but those most likely to appear in an abdominal OSCE station include inflammatory bowel disease, coeliac disease, liver cirrhosis and lymphoma of the gastrointestinal tract.
To assess for finger clubbing:
- Ask the patient to place the nails of their index fingers back to back.
- In a healthy individual, you should be able to observe a small diamond-shaped window (known as Schamroth’s window).
- When finger clubbing develops, this window is lost.
Asterixis (flapping tremor)
Asterixis (also known as ‘flapping tremor’) is a type of negative myoclonus characterised by irregular lapses of posture causing a flapping motion of the hands. In the context of an abdominal examination, the most likely underlying cause is either hepatic encephalopathy (due to hyperammonaemia) or uraemia secondary to renal failure. CO2 retention secondary to type 2 respiratory failure is another possible cause of asterixis.
- Ask the patient to stretch their arms out in front of them.
- Then ask them to cock their hands backwards at the wrist joint and hold the position for 30 seconds.
- Observe for evidence of asterixis during this time period.
Palpation
Temperature
Place the dorsal aspect of your hand onto the patient’s to assess temperature:
- In healthy individuals, the hands should be symmetrically warm, suggesting adequate perfusion.
- Cool hands may suggest poor peripheral perfusion.
Radial pulse
Assess the patient’s radial pulse:
- Palpate the patient’s radial pulse, located at the radial side of the wrist, with the tips of your index and middle fingers aligned longitudinally over the course of the artery.
- Once you have located the radial pulse, assess the rate and rhythm.
Dupuytren’s contracture
Dupuytren’s contracture involves thickening of the palmar fascia, resulting in the development of cords of palmar fascia which eventually cause contracture deformities of the fingers and thumb. There are a number of factors that have been associated with the development of Dupuytren’s contracture including genetics, excessive alcohol use, increasing age, male gender and diabetes.
To assess for Dupuytren’s contracture:
- Support the patient’s hand and palpate the palm to detect bands of thickened palmar fascia that feel cord-like.
Arms and axillae
Arms
Inspect the patient’s arms for the following:
- Bruising: may suggest underlying clotting abnormalities secondary to liver disease (e.g. cirrhosis).
- Excoriations: scratch marks that may be caused by the patient trying to relieve pruritis. In the context of an abdominal examination, this may suggest underlying cholestasis.
- Needle track marks: important to note as intravenous drug use can be associated with an increased risk of viral hepatitis.
Axillae
Whilst supporting the patient’s arm, inspect each axilla for the following:
- Acanthosis nigricans: darkening (hyperpigmentation) and thickening (hyperkeratosis) of the axillary skin which can be benign (most commonly in dark-skinned individuals) or associated with insulin resistance (e.g. type 2 diabetes mellitus) or gastrointestinal malignancy (most commonly stomach cancer).
- Hair loss: loss of axillary hair associated with iron-deficiency anaemia and malnutrition.
Face
Eyes
Ask the patient to gently pull down their lower eyelid and inspect for signs suggestive of gastrointestinal pathology:
- Conjunctival pallor: suggestive of underlying anaemia.
- Jaundice: most evident in the superior portion of the sclera (ask the patient to look downwards as you lift their upper eyelid).
- Corneal arcus: a hazy white, grey or blue opaque ring located in the peripheral cornea, typically occurring in patients over the age of 60. In older patients, the condition is considered benign, however, its presence in patients under the age of 50 suggests underlying hypercholesterolaemia.
- Xanthelasma: yellow, raised cholesterol-rich deposits around the eyes associated with hypercholesterolaemia.
- Kayser-Fleischer rings: dark rings that encircle the iris associated with Wilson’s disease. The disease involves abnormal copper processing by the liver, resulting in accumulation and deposition in various tissues (including the liver causing cirrhosis).
- Perilimbal injection: inflammation of the area of conjunctiva adjacent to the iris. Perilimbal injection is a sign of anterior uveitis, which can be associated with inflammatory bowel disease. Other clinical features of anterior uveitis include photophobia, ocular pain and reduced visual acuity.
Mouth
Ask the patient to open their mouth and inspect for signs suggestive of gastrointestinal pathology:
- Angular stomatitis: a common inflammatory condition affecting the corners of the mouth. It has a wide range of causes including iron deficiency (e.g. gastrointestinal malignancy, malabsorption).
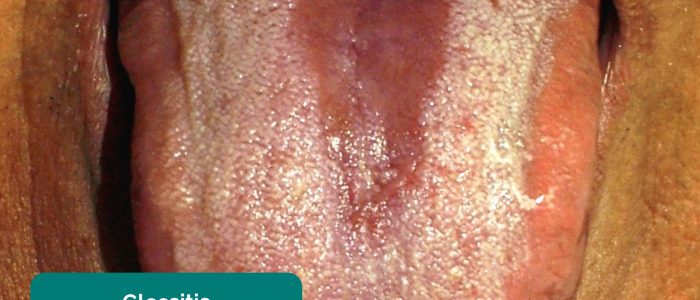
- Glossitis: smooth erythematous enlargement of the tongue associated with iron, B12 and folate deficiency (e.g. malabsorption secondary to inflammatory bowel disease).
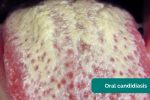
- Oral candidiasis: a fungal infection commonly associated with immunosuppression. It is characterised by pseudomembranous white slough which can be easily wiped away to reveal underlying erythematous mucosa.
- Aphthous ulceration: round or oval ulcers occurring on the mucous membranes inside the mouth. Aphthous ulcers are typically benign (e.g. due to stress or mechanical trauma), however, they can be associated with iron, B12 and folate deficiency as well as Crohn’s disease.
- Hyperpigmented macules: pathognomonic for Peutz-Jeghers syndrome, an autosomal dominant genetic disorder that results in the development of polyps in the gastrointestinal tract.
Neck
The left supraclavicular lymph node (known as Virchow’s node) receives lymphatic drainage from the abdominal cavity and therefore enlargement of Virchow’s node can be one of the first clinical signs of metastatic intrabdominal malignancy (most commonly gastric cancer). The right supraclavicular lymph node receives lymphatic drainage from the thorax and therefore lymphadenopathy in this region can be associated with metastatic oesophageal cancer (as well as malignancy from other thoracic viscera).
Palpate for lymphadenopathy
Palpate the supraclavicular fossa on each side, paying particular attention to Virchow’s node on the left for evidence of lymphadenopathy.
Chest
Inspect the patient’s chest for signs suggestive of gastrointestinal pathology:
- Spider naevi: skin lesions that have a central red papule with fine red lines extending radially caused by increased levels of circulating oestrogen. Spider naevi are commonly associated with liver cirrhosis, but can also be a normal finding in pregnancy or in women taking the combined oral contraceptive pill. If more than 5 are present it is more likely to be associated with pathology such as liver cirrhosis.
- Gynaecomastia: enlargement of male breast tissue caused by increased levels of circulating oestrogen (e.g. liver cirrhosis). Other causes include medications such as digoxin and spironolactone.
- Hair loss: also caused by increased levels of circulating oestrogen. General malnourishment can also result in hair loss.
Abdominal inspection
Position the patient lying flat on the bed, with their arms by their sides and legs uncrossed for abdominal inspection and subsequent palpation.
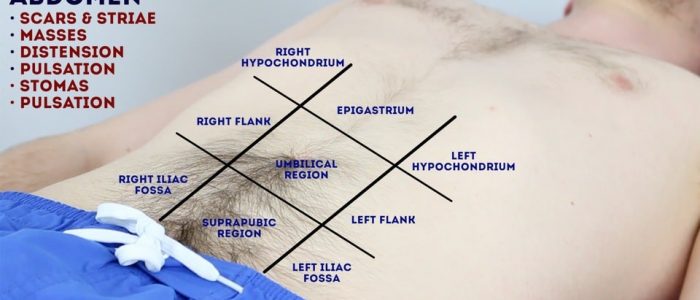
Inspect the patient’s abdomen for signs suggestive of gastrointestinal pathology:
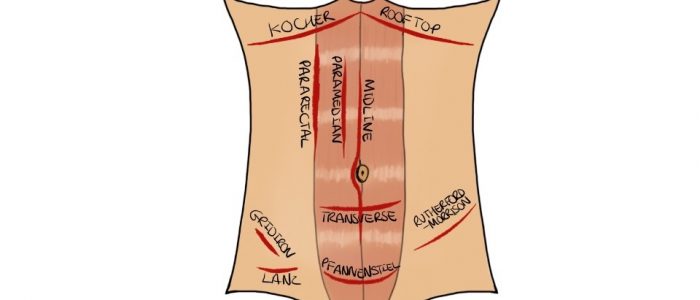
- Scars: there are many different types of abdominal scars that can provide clues as to the patient’s past surgical history (see image below for examples).
- Abdominal distension: can be caused by a wide range of pathology including the six f’s (fat, fluid, flatus, faeces, fetus or fulminant mass).
- Caput medusae: engorged paraumbilical veins associated with portal hypertension (e.g. liver cirrhosis).
- Striae (stretch marks): caused by tearing during the rapid growth or overstretching of skin (e.g. ascites, intrabdominal malignancy, Cushing’s syndrome, obesity, pregnancy).
- Hernias: ask the patient to cough and observe for any protrusions through the abdominal wall (e.g. umbilical hernia, incisional hernia).
- Cullen’s sign: bruising of the tissue surrounding the umbilicus associated with haemorrhagic pancreatitis (a late sign).
- Grey-Turner’s sign: bruising in the flanks associated with haemorrhagic pancreatitis (a late sign).
Stomas
If a stoma is present, assess the following characteristics:
- Location: this can provide clues as to the type of stoma (e.g. colostomies are typically located in the left iliac fossa, ileostomies and urostomies are typically located in the right iliac fossa).
- Contents: can be stool (e.g. colostomy or ileostomy) or urine (e.g. urostomy).
- Consistency of stool: note if it is liquid (ileostomy) or solid (colostomy).
- Spout: colostomies are flush to the skin with no spout whereas ileostomies and urostomies have a spout.
Abdominal palpation
Preparation
Before beginning abdominal palpation:
- The patient should already be positioned lying flat on the bed.
- Ask the patient if they are aware of any areas of abdominal pain (if present, examine these areas last).
- Kneel beside the patient to carry out palpation and observe their face throughout the examination for signs of discomfort.
Light palpation of the abdomen
Lightly palpate each of the nine abdominal regions, assessing for clinical signs suggestive of gastrointestinal pathology:
- Tenderness: note the abdominal region(s) involved and the severity of the pain.
- Rebound tenderness: said to be present when the abdominal wall, having been compressed slowly, is released rapidly and results in sudden sharp abdominal pain. This is a non-specific, unreliable clinical sign that can, in some cases, be associated with peritonitis (e.g. appendicitis).
- Voluntary guarding: contraction of the abdominal muscles in response to pain
- Involuntary guarding/rigidity: involuntary tension in the abdominal muscles that occurs on palpation associated with peritonitis (e.g. appendicitis, diverticulitis).
- Rovsing’s sign: palpation of the left iliac fossa causes pain to be experienced in the right iliac fossa. This sign was historically said to be indicative of appendicitis, but it is not reliable and at best indicates peritoneal inflammation of any cause affecting the left and/or right iliac fossa.
- Masses: large or superficial masses (e.g. hernias) may be noted on light palpation.
Deep palpation of the abdomen
Palpate each of the nine abdominal regions again, this time applying greater pressure to identify any deeper masses. Warn the patient this may feel uncomfortable and ask them to let you know if they want you to stop. You should also carefully monitor the patient’s face for evidence of discomfort (as they may not vocalise this).
If any masses are identified during deep palpation, assess the following characteristics:
- Location: note which of the nine abdominal regions the mass located within.
- Size and shape: assess the approximate size and shape of the mass.
- Consistency: assess the consistency of the mass (e.g. smooth, soft, hard, irregular).
- Mobility: assess if the mass appears to be attached to superficial or underlying structures.
- Pulsatility: note if the mass feels pulsatile, suggestive of vascular aetiology (e.g. abdominal aortic aneurysm).
Palpate the liver
1. Begin palpation in the right iliac fossa, starting at the edge of the superior iliac spine, using the flat edge of your hand (the radial side of your right index finger).
2. Ask the patient to take a deep breath and as they begin to do this palpate the abdomen. Feel for a step as the liver edge passes below your hand during inspiration (a palpable liver edge this low in the abdomen suggests gross hepatomegaly).
3. Repeat this process of palpation moving 1-2 cm superiorly from the right iliac fossa each time towards the right costal margin.
4. As you get close to the costal margin (typically 1-2 cm below it) the liver edge may become palpable in healthy individuals.
If you are able to identify the liver edge, assess the following characteristics:
- Degree of extension below the costal margin: if greater than 2 cm this suggests hepatomegaly.
- Consistency of the liver edge: a nodular consistency is suggestive of cirrhosis.
- Tenderness: hepatic tenderness may suggest hepatitis or cholecystitis (as you may be palpating the gallbladder)
- Pulsatility: pulsatile hepatomegaly is associated with tricuspid regurgitation.
Causes of hepatomegaly
There is a wide range of possible causes of hepatomegaly including but not limited to:
- Hepatitis (infective and non-infective)
- Hepatocellular carcinoma
- Hepatic metastases
- Wilson’s disease
- Haemochromatosis
- Leukaemia
- Myeloma
- Glandular fever
- Primary biliary cirrhosis
- Tricuspid regurgitation
- Haemolytic anaemia
Palpate the gallbladder
In healthy individuals, the gallbladder is not usually palpable. If the gallbladder is palpable it suggests enlargement secondary to biliary flow obstruction (e.g. pancreatic malignancy, gallstones) and/or infection (e.g. cholecystitis).
Palpation of the gallbladder can be attempted at the right costal margin, in the mid-clavicular line (the tip of the 9th rib). If the gallbladder is enlarged, a well-defined round mass that moves with respiration may be noted. Tenderness suggests a diagnosis of cholecystitis whereas a distended painless gallbladder may indicate underlying pancreatic cancer (particularly if also associated with jaundice).
Murphy’s sign
1. Position your fingers at the right costal margin in the mid-clavicular line at the liver’s edge.
2. Ask the patient to take a deep breath.
If the patient suddenly stops mid-breath due to pain, this suggests the presence of cholecystitis (known as “Murphy’s sign positive”).
Palpate the spleen
1. Begin palpation in the right iliac fossa, starting at the edge of the superior iliac spine, using the flat edge of your hand (the radial side of your right index finger).
2. Ask the patient to take a deep breath and as they begin to do this palpate the abdomen with your fingers aligned with the left costal margin. Feel for a step as the splenic edge passes below your hand during inspiration (the splenic notch may be noted).
3. Repeat this process of palpation moving 1-2 cm superiorly from the right iliac fossa each time towards the left costal margin.
In healthy individuals, you should not be able to palpate the spleen. A palpable spleen at the edge of the left costal margin would suggest splenomegaly (for the spleen to be palpable at this location it would need to be approximately three times its normal size).
Causes of splenomegaly
There is a wide range of possible causes of splenomegaly including but not limited to:
- Portal hypertension secondary to liver cirrhosis
- Haemolytic anaemia
- Congestive heart failure
- Splenic metastases
- Glandular fever
Ballot the kidneys
1. Place your left hand behind the patient’s back, below the ribs and underneath the right flank.
2. Then place your right hand on the anterior abdominal wall just below the right costal margin in the right flank.
3. Push your fingers together, pressing upwards with your left hand and downwards with your right hand.
4. Ask the patient to take a deep breath and as they do this feel for the lower pole of the kidney moving down between your fingers. This bimanual method of kidney palpation is known as balloting.
5. If a kidney is ballotable, describe its size and consistency.
6. Repeat this process on the opposite side to ballot the left kidney.
In healthy individuals, the kidneys are not usually ballotable, however, in patients with a low body mass index, the inferior pole can sometimes be palpated during inspiration.
Causes of enlarged kidneys
- Bilaterally enlarged, ballotable kidneys can occur in polycystic kidney disease or amyloidosis.
- A unilaterally enlarged, ballotable kidney can be caused by a renal tumour.
Palpate the aorta
1. Using both hands perform deep palpation just superior to the umbilicus in the midline.
2. Note the movement of your fingers:
- In healthy individuals, your hands should begin to move superiorly with each pulsation of the aorta.
- If your hands move outwards, it suggests the presence of an expansile mass (e.g. abdominal aortic aneurysm).
This is a crude clinical test and further investigations would be required before a diagnosis of an abdominal aortic aneurysm was made.
Palpate the bladder
Before performing bladder palpation, allow the patient the opportunity to go to the toilet. Warn the patient that palpation may be uncomfortable and bring about the sudden urge to pass urine.
A distended bladder can be palpated in the suprapubic area arising from behind the pubic symphysis (e.g. urinary obstruction/retention). In most healthy patients who are passing urine regularly, the bladder will not be palpable.
Abdominal percussion
Percuss the liver
1. Percuss upwards 1-2 cm at a time from the right iliac fossa (the same position used to begin palpation) towards the right costal margin until the percussion note changes from resonant to dull indicating the location of the lower liver border.
2. Continue to percuss upwards 1-2 cm at a time until the percussion note changes from dull to resonant indicating the location of the upper liver border.
3. Use the knowledge of the upper and lower border of the liver to determine its approximate size.
Percuss the spleen
Percuss upwards 1-2 cm at a time from the right iliac fossa (the same position used to begin palpation) towards the left costal margin until the percussion note changes from resonant to dull indicating the location of the spleen (in the absence of splenomegaly the spleen should not be identifiable using percussion).
Percuss the bladder
Percuss downwards in the midline from the umbilical region towards the pubic symphysis. A distended bladder will be dull to percussion allowing you to approximate the bladder’s upper border.
Assess shifting dullness
Percussion can also be used to assess for the presence of ascites by identifying shifting dullness:
1. Percuss from the umbilical region to the patient’s left flank. If dullness is noted, this may suggest the presence of ascitic fluid in the flank.
2. Whilst keeping your fingers over the area at which the percussion note became dull, ask the patient to roll onto their right side (towards you for stability).
3. Keep the patient on their right side for 30 seconds and then repeat percussion over the same area.
4. If ascites is present, the area that was previously dull should now be resonant (i.e. the dullness has shifted).
Abdominal auscultation
Assess bowel sounds
Auscultate over at least two positions on the abdomen to assess bowel sounds:
- Normal bowel sounds: typically described as gurgling (listen to an example in our video demonstration)
- Tinkling bowel sounds: typically associated with bowel obstruction.
- Absent bowel sounds: suggests ileus which is a disruption of the normal propulsive ability of the intestine due to a malfunction of peristalsis. Causes of ileus include electrolyte abnormalities and recent abdominal surgery. To be able to confidently state that a patient has ‘absent bowel sounds’ you need to auscultate for at least 3 minutes (this is unlikely to be the case in an OSCE given the time restraints).
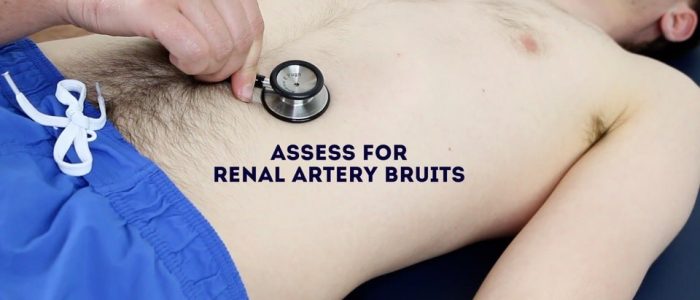
Listen for bruits
Auscultate over the aorta and renal arteries to identify vascular bruits suggestive of turbulent blood flow:
- Aortic bruits: auscultate 1-2 cm superior to the umbilicus, a bruit here may be associated with an abdominal aortic aneurysm.
- Renal bruits: auscultate 1-2 cm superior to the umbilicus and slightly lateral to the midline on each side. A bruit in this location may be associated with renal artery stenosis.
Legs
Assess the patient’s lower legs for evidence of pitting oedema which may suggest hypoalbuminaemia (e.g. liver cirrhosis, protein-losing enteropathy).
To complete the examination…
Explain to the patient that the examination is now finished.
Thank the patient for their time.
Dispose of PPE appropriately and wash your hands.
Summarise your findings.
Example summary
“Today I examined Mrs Smith, a 64-year-old female. On general inspection, the patient appeared comfortable at rest, with no evidence of abdominal distension or jaundice. There were no objects or medical equipment around the bed of relevance.”
“The hands had no peripheral stigmata of gastrointestinal disease and were symmetrically warm. There was no evidence of asterixis.”
“The pulse was regular at 70 beats per minute.”
“The arms did not have any evidence of bruising or excoriations and the axillae were unremarkable.”
“On inspection of the face, there were no stigmata of gastrointestinal disease.”
“There was no evidence of lymphadenopathy in the supraclavicular region.”
“Closer inspection of the chest did not reveal any stigmata of gastrointestinal disease.”
“On inspection of the abdomen, no scars, distension or hernias were noted. Abdominal palpation and percussion were unremarkable with no evidence of organomegaly. Bowels sounds were normal and no bruits were noted.”
“There was no evidence of peripheral oedema on the assessment of the legs.”
“In summary, these findings are consistent with a normal abdominal examination.”
“For completeness, I would like to perform the following further assessments and investigations.”
Further assessments and investigations
- Check hernial orifices (e.g. if there are signs of bowel obstruction). See our hernia examination guide for more details.
- Perform a digital rectal examination (PR) (e.g. if there is suspicion of gastrointestinal bleeding).
- Perform an examination of the external genitalia (e.g. to rule out testicular torsion as a cause of referred abdominal pain or an indirect inguinal hernia).
Reviewer
Dr Ally Speight
Consultant in Gastroenterology
References
- Adapted by Geeky Medics. James Heilman, MD. Jaundice. Licence: CC BY 3.0.
- Adapted by Geeky Medics. James Heilman, MD. Ascites. Licence: CC BY 3.0.
- Adapted by Geeky Medics. James Heilman, MD. Peripheral pallor. Licence: CC BY-SA.
- Adapted by Geeky Medics. CHeitz. Koilonychia. Licence: CC BY 2.0.
- Adapted by Geeky Medics. BrotherLongLegs. Leukonychia. Licence: CC BY-SA.
- Adapted by Geeky Medics. Desherinka. Finger clubbing. Licence: CC BY-SA.
- Adapted by Geeky Medics. Frank C. Müller. Dupuytren’s. Licence: CC BY-SA.
- Adapted by Geeky Medics. Madhero88. Acanthosis nigricans. Licence: CC BY-SA.
- Adapted by Geeky Medics. Sheila J. Toro. Scleral jaundice. Licence: CC BY 4.0.
- Adapted by Geeky Medics. Klaus D. Peter, Gummersbach, Germany. Xanthelasma. Licence: CC BY 3.0 DE.
- Adapted by Geeky Medics. Herbert L. Fred, MD, Hendrik A. van Dijk. Kayser-Fleischer ring. Licence: CC BY 3.0.
- Adapted by Geeky Medics. Jonathan Trobe, M.D. Anterior uveitis. Licence: CC BY 3.0.
- Adapted by Geeky Medics. Matthew Ferguson. Angular stomatitis. Licence: CC BY-SA.
- Adapted by Geeky Medics. Klaus D. Peter, Gummersbach. Glossitis. Licence: Klaus D. Peter, Gummersbach, Germany. Licence: CC BY 3.0 DE.
- Adapted by Geeky Medics. James Heilman, MD. Oral candidiasis. Licence: CC BY-SA.
- Adapted by Geeky Medics. Aphthous ulcer. Licence: Public domain.
- Adapted by Geeky Medics. Abdullah Sarhan. Peutz-Jager syndrome. Licence: CC BY-SA.
- Adapted by Geeky Medics. Herbert L. Fred, MD and Hendrik A. van Dijk. Spider naevi. Licence: CC BY.
- Adapted by Geeky Medics. PanaromicTiger. Striae. Licence: CC BY-SA.
- Adapted by Geeky Medics. Umbilical hernia. Licence: Public domain.
- Adapted by Geeky Medics. Jmarchn. Incisional hernia. Licence: CC BY-SA.
- Adapted by Geeky Medics. Herbert L. Fred, MD and Hendrik A. van Dijk. Cullen’s sign. Licence: CC BY.
- Adapted by Geeky Medics. Herbert L. Fred, MD and Hendrik A. van Dijk. Grey-Turner’s sign. Licence: CC BY.
- Adapted by Geeky Medics. Cancer Research UK. Colostomy. Licence: CC BY-SA.
- Adapted by Geeky Medics. Eric Polsinelli. Ileostomy. Licence: CC BY 4.0.
- Adapted by Geeky Medics. Anandselvam85. Hepatomegaly. Licence: CC BY-SA.
- Adapted by Geeky Medics. Stefania Leoni, Dora Buonfrate, Andrea Angheben, Federico Gobbi, Zeno Bisoffi. Splenomegaly. Licence: CC BY 4.0.
- Adapted by Geeky Medics. James Heilman, MD. Pedal oedema. Licence: CC BY-SA.