- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Chest pain is a common presentation, and the diagnosis of acute coronary syndrome is frequently suspected. Acute coronary syndrome (ACS) encompasses a variety of diagnoses and can be subcategorised into:
- ST-elevation ACS: ST-elevation myocardial infarction (STEMI)
- Non-ST elevation ACS: Non-ST elevation myocardial infarction (NSTEMI) and unstable angina
Aetiology
Two of the three diagnoses that exist under the umbrella of ACS are types of myocardial infarction (STEMI and NSTEMI).
Definition of myocardial infarction (MI)
The European Society of Cardiology’s definition of MI is as follows…
Detection of a rise and/or fall in cardiac biomarker values (preferably troponin) with at least one value above the 99th percentile (upper reference limit) with at least one of the following:
- Symptoms of ischaemia (the patient’s history and clinical presentation and the history are vital to guide your interpretation of the tests you are about to perform)
- New or presumed new significant ST segment or T wave changes or new left bundle branch block (LBBB)
- Pathological Q wave changes on the ECG
- Imaging evidence of new loss of viable myocardium or new regional wall motion abnormality
- Identification of an intracoronary thrombus by angiography
A ‘new left bundle branch block’ does not mean ‘a left bundle branch block that has just been found because the patient has never had an ECG before’. Nor does it mean ‘a left bundle branch block that is present now but was not present on an ECG in 2006’.
A new LBBB due to ischaemia is the result of an occluded proximal left anterior descending (LAD) or left main stem artery. A large amount of myocardium and conductive tissue needs to be affected to cause this ECG appearance and these patients are usually acutely unwell.
Development of Q waves on the ECG
The Q wave reflects septal depolarisation. This is usually hidden behind the much more forceful and electrically active ventricular wall depolarisation. If the ventricular wall is dead, a ‘window’ is created that allows the septal depolarisation to show up on the surface ECG.
Imaging evidence of new regional wall abnormality
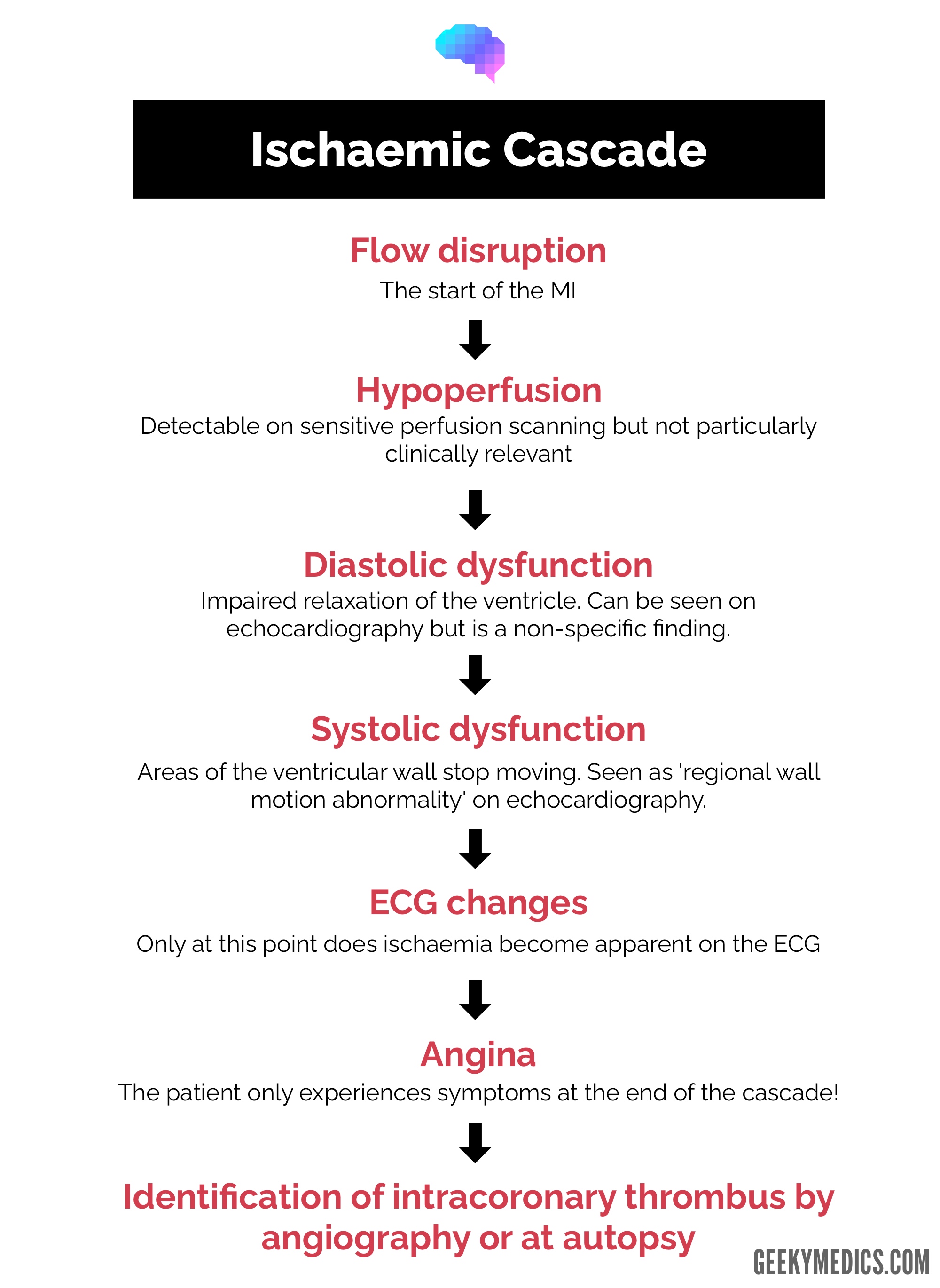
The sequence of changes and signs of ischaemia (the ischaemic cascade) on various tests is shown in Figure 1.
Troponin
A troponin level is only a number. It is only relevant when applied in the context of other clinical findings.
There are many causes of a raised troponin, including:1
- Myocardial infarction
- Tachy/bradyarrhythmias
- Aortic dissection
- Severe aortic valve disease
- Hypertrophic cardiomyopathy
- Severe respiratory failure
- Severe anaemia
- Coronary spasm
- Heart failure
- Takotsubo cardiomyopathy
- Sepsis
- Renal failure
- Stroke
- Subarachnoid haemorrhage
Classification of myocardial infarctions
Type 1: spontaneous myocardial infarction
This is your ‘typical’ myocardial infarction. Atherosclerosis originates from damage to the endothelium and a build-up of cholesterol.
The inflammatory reaction to atherosclerosis by macrophages causes a plaque of foam cells, lipids, cellular debris and (eventually) calcium to build up with a fibrous cap on top.
When this cap cracks, the exposed debris triggers thrombus formation in the confines of the affected coronary artery (which are only typically between 2 and 5mm in diameter), causing partial or total occlusion of the artery.
Type 2: myocardial infarction secondary to ischaemia
A type 2 myocardial infarction is a common event in hospitals where patients with stable coronary artery disease +/- previous coronary intervention (PCI or CABG) are unwell and put additional stress on their heart that would not normally be present.
If there is a sufficient imbalance between the supply of blood (e.g. anaemia/hypovolaemia, coronary vasospasm) and demand for blood (e.g. sepsis/hypovolaemic shock, tachyarrhythmia) then the myocardium can become ischaemic without a plaque rupture event.
Type 3 MI: post-mortem
A type 3 myocardial infarction is diagnosed post-mortem.
Type 4a MI: percutaneous coronary intervention
This is related to percutaneous coronary intervention (i.e. caused by an angioplasty procedure blocking a side branch or damaging the main coronary artery causing ischaemia)
Type 4b MI: stent thrombosis
This is related to stent thrombosis. If patients stop anti-platelets early post-angioplasty or continue to smoke, stents can occlude (this usually results in a STEMI if complete sudden thrombosis or NSTEMI if gradual re-stenosis over time).
Type 5 MI: bypass
Type 5 myocardial infarction is related to a bypass graft (CABG) operation.
Clinical features
The clinical features of ACS are similar, regardless of the underlying diagnosis (e.g. NSTEMI, STEMI or unstable angina).
Typical clinical presentations of ACS include:2
- pain in the chest and/or other areas (for example, the arms, back or jaw) lasting longer than 15 minutes
- chest pain associated with nausea and vomiting, marked sweating and breathlessness
- chest pain associated with haemodynamic instability
- new-onset chest pain, or abrupt deterioration in previously stable angina, with recurrent chest pain occurring frequently and with little or no exertion, and with episodes often lasting longer than 15 minutes.
For more information, see the Geeky Medics guide to a chest pain history.
Management
When ACS is suspected, initial management should be commenced as soon as possible:2
- Resting 12-lead ECG
- Morphine
- Oxygen: only if low SpO2
- Nitrates (e.g. glyceryl trinitrate)
- Aspirin (300 mg) and a second rapid-acting antiplatelet such as Ticagrelor or Prasugrel
For more information, see the Geeky Medics guide to the emergency management of ACS.
ST-elevation ACS
ST-elevation myocardial infarction (STEMI)
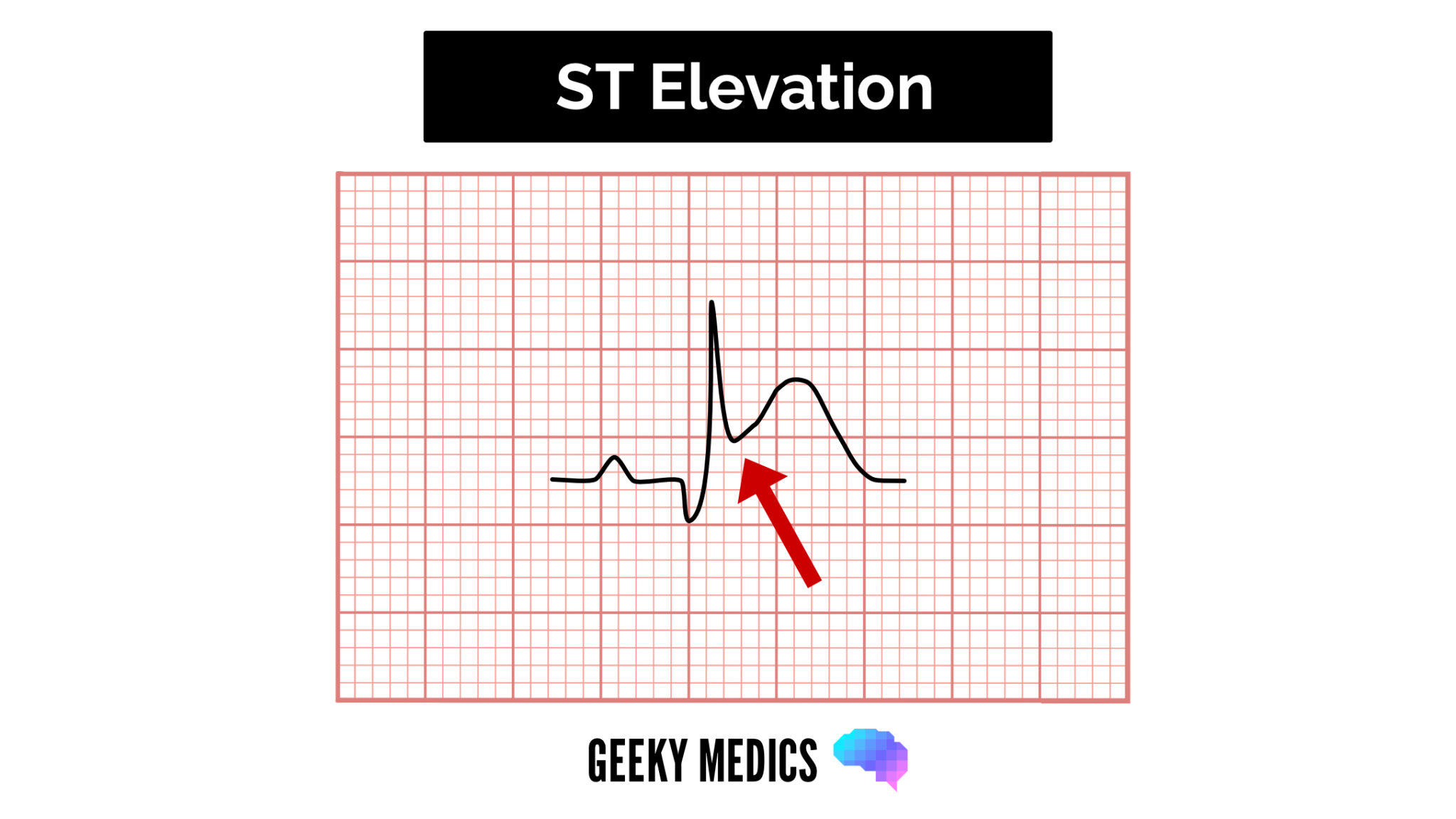
Patients with STEMI typically present with acute chest pain and persistent (>20 minutes) ST-segment elevation.
ST elevation is a sign of complete occlusion of an epicardial coronary artery by thrombus causing immediate myocardial death relating to the territory affected:
- Anterior: V1-V4
- Inferior: II, III, aVF
- High lateral: I, aVL
- Low lateral: V5, V6
- Posterior: a dominant R wave in V1-3 with ST depression in V1-3 (the mirror image of an anterior MI)
These patients are at elevated risk of ventricular arrhythmias and myocardial damage can be minimised by rapidly opening the artery.
Management of STEMI3
The current gold standard treatment option is primary percutaneous intervention (PCI) to allow the vessel to be opened as quickly as possible (as ‘time is muscle’).
Studies have shown that it is beneficial to delay treatment for up to 90 minutes to allow transfer to a primary PCI centre rather than resorting to thrombolysis.
There is a benefit associated with performing primary PCI up to 12 hours from the onset of pain. After that point, the OAT trial suggests that there is limited benefit in opening up the occluded artery as the damage is already done.4
The recommended treatment used to be thrombolysis to try and break down the clot in the artery. However, this has significant bleeding risks attached to it and often failed to open the artery up requiring the patient to undergo ‘rescue angioplasty’ with higher bleeding risks associated due to the pre-medication.
Non-ST-elevation ACS
Non-ST-elevation myocardial infarction (NSTEMI)
Non-ST elevation myocardial infarctions (NSTEMIs) are often seen as a more ‘routine’ heart attack. However, they have worse long-term outcomes than STEMIs (although a lower risk of death in the short term).
They tend to be associated with partial coronary occlusion.
Diagnosis of an NSTEMI involves a combination of, clinical assessment, serial troponin measurement and ECG analysis (see definition of MI earlier in the article). For more information, see the Geeky Medics guide to NSTEMIs.
Management of NSTEMI5
Initiate further medical treatment once a diagnosis of NSTEMI is confirmed (with serial troponin measurement):
- Beta blockade (or alternative rate-limiting agent if contraindicated – aim HR of 50-60 bpm)
- ACE inhibitor (unless contraindicated – aim for a systolic blood pressure of 120 mmHg or less)
- Atorvastatin 80mg OD
Once someone is diagnosed with a type I NSTEMI and commenced on appropriate medical therapy, there are various risk scores that can be calculated to assess the value of invasive angiography.
NICE recommends the use of the GRACE score which is used to predict in-hospital and post-discharge to 6-month mortality.
Other factors that should be considered before proceeding to angiography include:
- Renal function (there is a risk of contrast nephropathy and this can leave predialysis patients permanently dependent on dialysis)
- Bleeding risk (as above)
- Can the patient lie flat? Although angiography can be performed whilst patients with severe heart failure are sat upright, it is not fun for the operator, cath lab team or the patient. In a non-urgent setting, angiography should be delayed until the patient is able to tolerate lying flat.
- Other significant co-morbidities: patients with poor quality of life and/or short life expectancy (age/dementia/malignancy) may not gain any prognostic benefit from the procedure and should be managed medically.
When to perform angiography
Unstable angina
Stable (or ‘exertional’) angina is defined as:
- Typical cardiac pain
- Brought on by exertion and relieved by rest
- Lasting less than 20 minutes
Diagnosis of unstable angina is based on clinical assessment. Troponin measurements will be normal as there has not been any ischaemic damage (yet) and the ECG may be normal for similar reasons.
Management of unstable angina5
Management of unstable angina is the same as for NSTEMI discussed above.
Editor
Dr Chris Jefferies
References
- Third Universal Definition of Myocardial Infarction. European Heart Journal (2012) 33, 2551 – 2567.
- Acute coronary syndromes (including myocardial infarction); NICE Quality Standard, Sept 2014. Available from: [LINK]
- NICE Guideline. Myocardial infarction with ST-segment elevation: acute management. Clinical guideline [CG167].
Published date: - Yousef ZR, Redwood SR, Bucknall CA, Sulke AN, Marber MS. Late intervention after anterior myocardial infarction: effects on left ventricular size, function, quality of life, and exercise tolerance: results of the Open Artery Trial (TOAT Study). J Am Coll Cardiol 2002;40:869-876
- NICE Guideline. Unstable angina and NSTEMI; NICE Clinical Guideline (March 2010 – last updated November 2013). Available from: [LINK]
- Roffi M, Patrono C, Collet JP, et al. 2015 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J. 2016 Jan 14;37(3):267-315.




