- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
The administration of local anaesthetic in dentistry is necessary to facilitate pain-free dental treatment. To achieve adequate analgesia, it is important to appreciate the relevant anatomy and be aware of the different anaesthetic agents available for use, complications associated with their administration and their contraindications.
This article provides an overview to aid your understanding of the procedure, it is not intended as a guide to performing the procedure on patients.
Innervation of the teeth
Adjacent teeth are innervated by the same nerve as outlined below.1
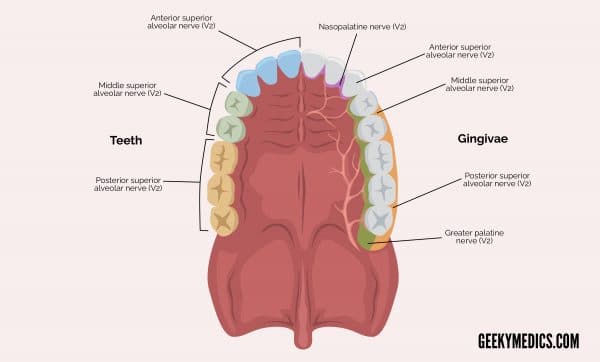
Maxillary arch
- Upper central incisor to upper canine: anterior superior alveolar nerve
- Upper first and second premolars: middle superior alveolar nerve
- Upper first molar to upper last molar: posterior superior alveolar nerve
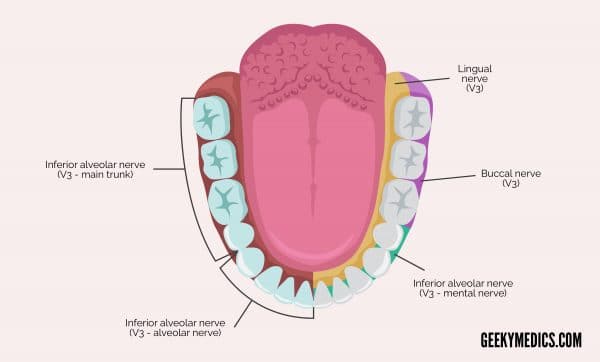
Mandibular arch
- Lower central incisor to lower first premolar: incisive branch of inferior alveolar nerve
- Lower second premolar to lower last molar: main trunk of inferior alveolar nerve
Innervation of the gingivae
The gingivae on either side of a tooth are innervated by different nerves.1
Maxillary arch
Innervation of the buccal/labial gingivae:
- Upper central incisor to upper canine: anterior superior alveolar nerve
- Upper first and second premolars: middle superior alveolar nerve
- Upper first molar to upper last molar: posterior superior alveolar nerve
Innervation of the palatal gingivae:
- Upper central incisor to upper canine: nasopalatine nerve
- Upper first premolar to upper last molar: greater palatine nerve
Mandibular arch
Innervation of the buccal/labial gingivae:
- Lower central incisor to lower second premolar: mental nerve
- Lower first molar to lower last molar: buccal nerve
Innervation of the lingual gingivae:
- Lower central incisor to lower last molar: lingual nerve
Types of local anaesthetic
The most widely used dental local anaesthetic agents are lidocaine, articaine, prilocaine and mepivacaine.
The most used local anaesthetic agent amongst general dental practitioners is lidocaine.3 Lidocaine is used in combination with adrenaline, most commonly as lidocaine hydrochloride 2% with 1:80,000 adrenaline (12.5mg/ml).
Articaine is also combined with adrenaline. For dental anaesthesia, it is used as articaine hydrochloride 4% with 1:100,000 adrenaline.
Mepivacaine hydrochloride is available with or without adrenaline. Prilocaine hydrochloride can be used with or without felypressin.4
Allergic reactions
It is uncommon for true allergy to occur. More commonly, when patients report that they are allergic to local anaesthetics, they have experienced syncope associated with injection, or cardiac palpitations from adrenaline in the local anaesthetic or released endogenously.
True allergic reactions are usually due to preservatives (e.g. methylparaben or sulphites). Allergy is more common with esters rather than amides.5
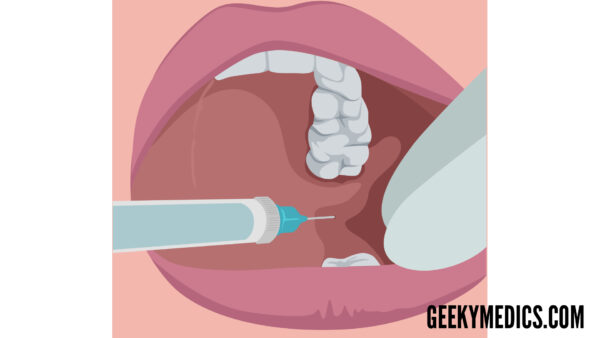
Infiltration of local anaesthetic
This technique is used to anaesthetise a single or a small number of adjacent teeth.
It works less effectively in mandibular molars and upper first molars due to the thickness of bone that must be penetrated. A supplementary local anaesthetic may be required for upper first molars. Lower molars often require an inferior alveolar nerve block for successful anaesthesia to be achieved for extractions.1
Procedure
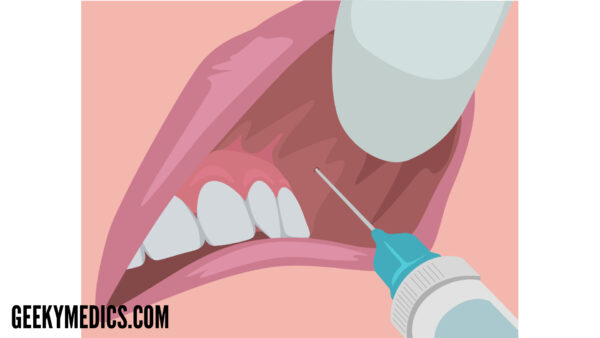
Performing infiltration of local anaesthetic involves the following steps:1,6
- Retraction of the lip/cheek
- Administration close to the tooth being anaesthetised, towards the apex of the root
- Aspiration of the needle before depositing the full volume of local anaesthetic to prevent intravascular injection
- Slow deposition of the solution
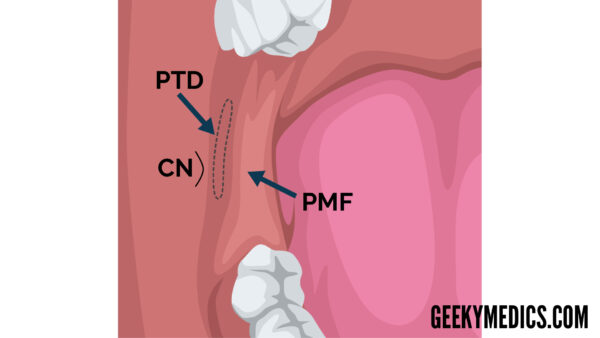
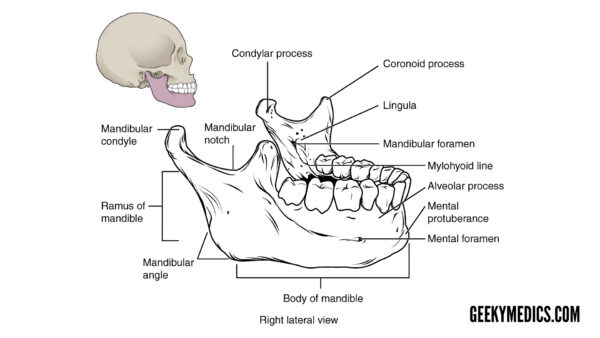
Inferior alveolar nerve block
An inferior alveolar nerve block is used to anaesthetise mandibular molar teeth. This nerve block will anaesthetise mandibular teeth from the last molar to the midline, gingivae, lip, chin, body of the mandible and periosteum.6
Procedure
1. First, the insertion point of the needle must be identified:
- Locate the coronoid notch; identify the external oblique ridge, palpate posteriorly and a concavity should be palpable.
- Palpate medially from this to find the internal oblique ridge.
- The pterygomandibular raphe should then be visualised.1,6
2. The needle must be parallel to the occlusal plane and 1.5cm above it, coming towards the point of insertion from the contralateral premolar region. The needle is inserted at this height and angle, lateral to the pterygomandibular raphe.
3. The needle is then advanced until two-thirds has penetrated the soft tissues – it is imperative that aspiration is then performed to ensure the needle is not positioned intravascularly.
4. Once aspiration has confirmed the needle is not positioned intravascularly, the local anaesthetic is administered.
5. As the needle is being removed (once halfway out), additional local anaesthetic is deposited to aid anaesthesia of the lingual nerve. Supplementary local infiltrations are often necessary to achieve complete anaesthesia for procedures such as extractions and root canal treatments.6
Complications
Penetrating the floor of the nose (maxillary infiltration)
Maxillary infiltration occurs if the needle is inserted too far superiorly, beyond the roots of maxillary incisor teeth. Consequently, analgesia is not achieved, and the patient may complain of fluid trickling down the throat.1 The risk of this complication can be reduced by using a shorter needle.
Intravascular injection
Intravascular injection can result in a haematoma and unwanted systemic side effects of local anaesthetic (and adrenaline). Again, this may also result in failed analgesia.1
Penetration of the parotid gland capsule (inferior alveolar nerve block)
Penetration of the parotid gland capsule can occur if the needle is advanced too posteriorly. The facial nerve (CN VII) becomes anaesthetised hence facial paralysis of the affected side occurs. The effects are reversible and will wear off as the local anaesthetic does, but this can be distressing for the patient.1
Rarer complications
Local ischaemic necrosis and paraesthesia may occur.5
Contraindications to local anaesthetic
True allergy to the local anaesthetic or key preservatives are the primary contraindications.5 However doses need to be administered carefully, considering the volume of adrenaline being used. Ensure a thorough medical history is taken prior to any administration of local anaesthetic.
Reviewer
Dr Anjani Holmes
Editor
Dr Chris Jefferies
References
- Liebgott B. The Anatomical Basis of Dentistry. 3rd Missouri: Elsevier Inc. 2011.
- Drake RL, Vogl AW, Mitchell AWM. Gray’s Anatomy for Students. 2nd Philadelphia: Elsevier Inc. 2010.
- Corbett, IP. Ramacciato J. Groppo, FC. Meechan, JG. A survey of local anaesthetic use among general dental practitioners in the UK attending postgraduate courses on pain control. British Dental Journal. 2005: 199(12):784-7.
- Joint Formulary Committee. British National Formulary (online). London: BMJ Group and Pharmaceutical Press. Available from: [LINK]
- Becker DE. Reed KL. Local Anesthetics: Review of Pharmacological Considerations. Anesthesia Progress. 2012: 59(2): 90–102.
- Reed KL. Malamed SF. Fonner AM. Local Anesthesia Part 2: Technical Considerations. Anesthesia Progress.2012: 59(3): 127–137.
- OpenStax College. Anatomy of the Mandible. License: [CC BY].