- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
There is a wide variety of equipment that can be used to support a patient’s airway and at first glance, it can seem a little overwhelming. This article aims to provide a basic overview of the most common airway equipment you may come across on the wards and in theatre.
The primary aims of airway management are to:
- ensure airway patency
- ensure ventilation of the lungs
- protect the lungs from soiling
For more information on oxygen masks, see the Geeky Medics guide to oxygen delivery devices.
Airway intervention overview
Table of airway interventions
| Airway intervention | Is the airway protected? |
| Airway manoeuvres | No |
| Oropharyngeal (Guedel) airway | No |
| Nasopharyngeal airway | No |
| iGel | No |
| Laryngeal mask | No |
| Proseal laryngeal mask | No |
| Endotracheal tube | Yes |
| Fibreoptic intubation | Yes |
| Cricothyroidotomy | Yes |
Airway manoeuvres
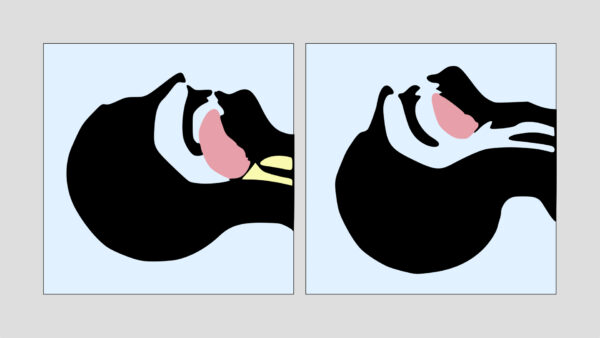
The overall aim of airway manoeuvres is to lift the tongue and soft tissues of the pharynx anteriorly to open the airway.
Head-tilt, chin-lift manoeuvre
Position the patient on their back.
Open their airway using a head-tilt chin-lift manoeuvre:
- Place one hand on the patient’s forehead and the other under the chin.
- Tilt the forehead back whilst lifting the chin forwards to extend the neck.
Jaw thrust
If the patient is suspected to have suffered significant trauma (with potential spinal involvement) perform a jaw-thrust rather than a head-tilt chin-lift manoeuvre. Use both hands to apply force behind the ramus of the mandible, displacing the lower jaw forwards and upwards.

Video demonstration
Oropharyngeal (Guedel) airway
Key facts:
- An oropharyngeal airway can help prevent the tongue and soft tissues of the pharynx from obstructing the airway.
- There are a variety of sizes available for children and adults.
- Size a patient’s airway by measuring the Guedel against a patient’s face: when the tip is placed at the angle of the jaw the flange should align with the centre of the top teeth (i.e. hard airway = measure “hard to hard”).
- Insert into the patient’s mouth upside down, pass to the back of the throat and rotate 180 degrees to fit behind the tongue base. In children, the Guedel should be inserted the right way up (i.e. not upside down).
Issues with Guedel airways:
- They are poorly tolerated in conscious and semi-conscious patients as it induces a gag reflex.
- They can cause trauma to teeth and the mucous membranes of the oral cavity.
Nasopharyngeal airway (NPA)
Key facts:
- Nasopharyngeal airways (NPAs) are typically used to bypass obstructions in the mouth, nose, nasopharynx or base of the tongue.
- The appropriate NPA size can be calculated by measuring from the tip of the patient’s nose to the tragus of the ear (i.e. soft airway = measure “soft to soft”).
- To insert an NPA, lubricate the tip and insert it into the right nostril aiming perpendicularly to the face to pass along the nasal passage and down into the pharynx.
- The NPA tip should sit just above the epiglottis and the flange should be at the tip of the nose.
Issues with NPAs:
- They should not be used in patients with suspected base of skull fracture.
- They can cause trauma to the nostril.

Supraglottic airways
Overview
Key facts:
- Supraglottic airways are a group of devices that sit abutting the larynx, above the vocal cords.
- They are typically used as alternatives to endotracheal airways in short or low-risk anaesthetic cases.
- They can also be used in prehospital and cardiac arrest settings to achieve a more secure airway without endotracheal intubation.
- If placed in cardiac arrest, cardiac compressions do not need to be interrupted as ventilation can be delivered simultaneously.
- Different types of supraglottic airways are described below with varying advantages and disadvantages.
Issues with supraglottic airways:
- Supraglottic airways do not protect against aspiration and therefore do not provide a definitive airway.
- Complications include gastric insufflation, aspiration, laryngospasm and partial airway obstruction.
- Supraglottic airways should not be used if there is poor mouth opening, pharyngeal pathology or obstruction at/below the level of the larynx.
Insertion method:
- The patient is positioned supine, with the neck flexed and head extended at the atlanto-occipital joint.
- The tube is inserted blind into the patient’s mouth and guided over the tongue until resistance is encountered.
- The tube can then be connected to a ventilation device and airway patency confirmed with chest movement, fogging of the tube and a CO2 trace.
- If there is no CO2 trace present, the airway is not patent and must be removed or adjusted.
Laryngeal mask airway (LMA)
Key facts:
- A laryngeal mask airway (LMA) is a reusable supraglottic device.
- It is made up of a silicone rubber tube that ends with an elliptical, spoon-shaped mask designed to fit over the larynx.
- The inflatable mask rim forms a low-pressure seal over the laryngeal inlet.
- Reinforced laryngeal masks are also available to prevent kinking.
- Proseal is a type of LMA that has an additional inflatable segment that provides a greater seal within the larynx and a gastric port for drainage of gastric secretions.
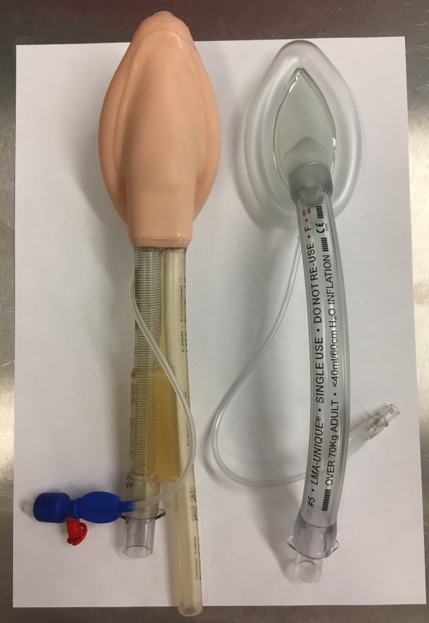
iGel
Key facts:
- An iGel is a single-use supraglottic airway device.
- It is made up of a non-inflatable thermoplastic elastomer that has been designed to create an anatomical seal around the larynx and peri-laryngeal structures when warmed to body temperature.
- An iGel is inserted via the same method discussed above, however, it does not require inflation to form a seal.

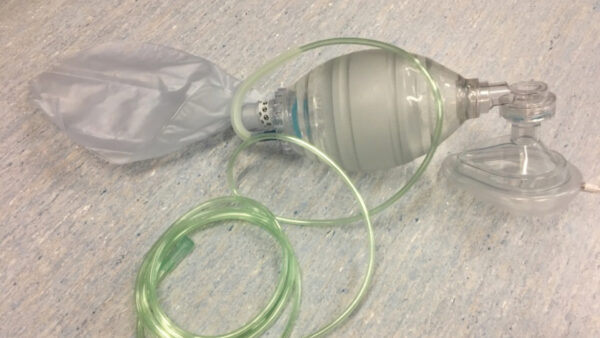
Self-inflating bag-valve resuscitator
Key facts:
- A self-inflating bag-valve resuscitator is also known by several other names including ambu bag, bag valve mask (BVM), self-inflating bag and manual resuscitator.
- A BVM is typically used to provide oxygenation and ventilation prior to placement of a definitive airway.
- The device consists of a face mask (variable size based on the patient) attached via a shutter valve to a flexible air chamber. The tubing connects the BVM to a flowmeter or oxygen cylinder.
- When the face mask is placed firmly over the patient’s face to create a seal, air entrainment is reduced and high oxygen concentrations can be delivered. If a reservoir bag is also used, it is possible to achieve an FiO2 of 100%.
- Patients can breathe spontaneously through the system or can be ventilated by squeezing the bag provided there is a firm seal between the mask and the patient’s face.
- Typically one person performs the airway opening manoeuvres and holds the mask onto the patient’s face with an effective seal and a second person squeezes the bag. If practised, one person can both hold the airway open and ventilate using the bag.
- The shutter valve and bag can also be connected to airway devices such as an LMA, iGel or ETT.
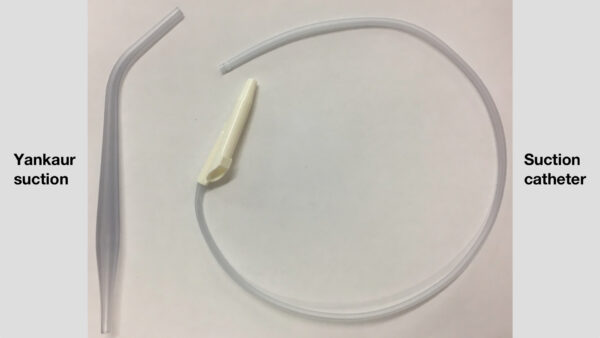
Suction
Key facts:
- In emergency situations, unprotected airways are at risk of soiling from secretions, saliva, gastric contents, blood or other debris. In these situations, suction can be used to clear the airway and improve the view during laryngoscopy.
- Suction devices should be available in all hospital bed spaces. Portable devices are also available for patient transfers.
- Yankaur suction refers to a firm plastic tube with a large opening that is used to clear the oropharynx.
- Suction catheters are long, flexible tubes that can be inserted into an ETT or tracheostomy tube to clear secretions from within the airway.
Laryngoscopes
Key facts:
- Laryngoscopy refers to the process of visualising the larynx and can be either direct or indirect. It is typically performed when attempting to pass an endotracheal tube through the vocal cords in order to achieve a definitive, protected airway.
- Laryngoscopes are used to facilitate endotracheal intubation as part of rapid sequence induction (RSI) or modified induction of anaesthesia. This should only be performed by trained clinicians.
- Macintosh laryngoscopes consist of a handle (with a battery inside) and attachable blades of different sizes. Each blade has a light that allows visualisation of the vocal cords. It is essential to check the connection and light before use.
- Laryngoscopes are held in the left hand. The blade is inserted along the right side of the tongue and positioned in the groove between the tongue and epiglottis. Soft tissues are lifted in the direction of the handle to reveal the vocal cords.
- A video laryngoscope is made up of a laryngoscope blade with a built-in camera that allows the larynx and vocal cords to be viewed on-screen beside the patient’s bed. Video laryngoscopy is used in airways where direct visualisation of the airway may be difficult. This is often not useful in patients with blood or secretions in the airway as the camera becomes obscured.
Issues with supraglottic airways:
- There is a significant risk of damaging teeth and oropharyngeal tissues.

Endotracheal tubes
Key facts:
- Endotracheal tubes (ETT) vary in length and diameter (the general sizing rule is 7.0 for women and 8.0 for men). Guidelines are available to calculate appropriate tube size for children based on weight.
- One end of the tube has a universal plastic connector that fits bag valve masks or a variety of ventilator tubing types. The distal end is shaped to ensure ventilation of both right and left bronchi and has a small hole (known as Murphy’s eye) which can be used for ventilation should the end of the tube become obstructed.
- Centimetre markings indicate the depth to which tube has been inserted. In normal adults, a tube should sit 20-24cm at the teeth.
- An inflatable cuff seals the trachea to protect against airway contamination and gas leaks. The cuff and pilot balloon should be tested before the tube is used.
- Variations include tubes with additional suction ports to remove secretions above the cuff, reinforced tubes with metal rings to reduce kinking and nasal endotracheal tubes for intubation of the trachea through the nose.

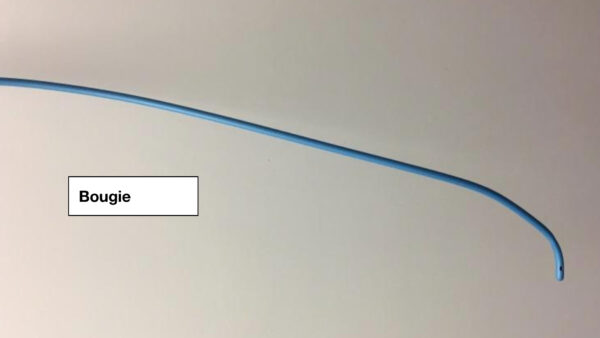
Gum elastic bougie
Key facts:
- A gum elastic bougie is a flexible instrument that can be moulded into a curved shape.
- It is placed into the airway under direct/indirect guidance before an ETT is railroaded over the top.
- They are typically used in situations where an airway may be challenging to intubate.
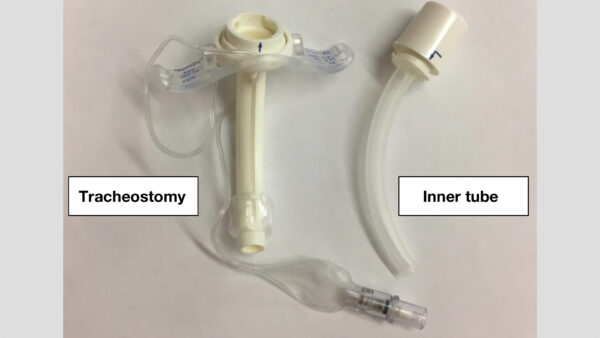
Tracheostomy tube
Key facts:
- Tracheostomies are used to bypass the upper airway, allowing a patient’s trachea to be ventilated through the front of the neck.
- A variety of specialised tracheostomy airway devices can be used depending on the patient’s requirements.
Insertion techniques:
Different insertion techniques are used, depending on the urgency of the situation:
- Cricothyroidotomy is performed in emergencies such as airway obstruction using needle or scalpel dissection to insert an airway through the membrane between the cricoid and thyroid cartilage.
- Surgical tracheostomy refers to an airway inserted directly through the trachea below the cricoid cartilage. It is performed by trained ENT surgeons in a controlled operating theatre environment.
Monitoring
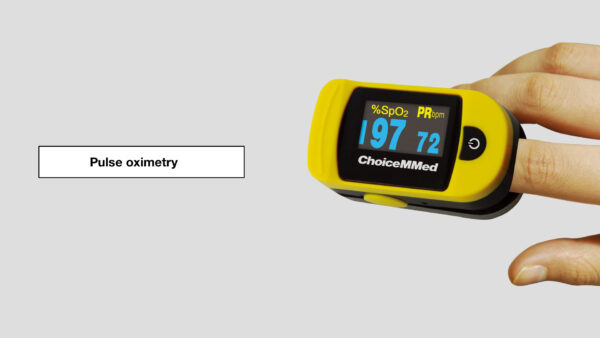
Pulse oximetry
Key facts:
- A pulse oximeter estimates arterial saturation of oxygen and is typically placed on the fingers, toes or ears.
- As a result of the oxyhaemoglobin dissociation curve, when oxygen saturations fall below 90%, any fall in the arterial partial pressure of oxygen will result in a sharp fall in recorded oxygen saturation.
Issues with pulse oximetry:
- Pulse oximetry is affected by the poor perfusion of the peripheries, false nails/nail varnish, excessive motion and carboxyhaemoglobin
Capnography
Key facts:
- Capnography is essential in determining the patency of a patient’s airway.
- CO2 is only produced in the lungs, therefore the presence of CO2 in expired gas confirms that the patient is being ventilated.
- Capnography is used to confirm the position of an ETT in the trachea. If there is no CO2 trace following intubation, the ETT must be removed and/or replaced.
- The shape of a CO2 curve can give an indication of the efficacy of ventilation.

References
- Nasal cannula: By BruceBlaus (Own work) [CC BY-SA 4.0] via Wikimedia Commons.
- Jaw thrust: By Randhillon (Own work) [CC BY-SA 4.0] via Wikimedia Commons.
- Pulse oximeter: By Thinkpaul (Own work) [CC BY-SA 3.0] via Wikimedia Commons.