- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Amblyopia, commonly known as lazy eye, is a unilateral or bilateral reduction in visual acuity due to an insult to the visual pathway during the critical period of visual development.
The critical period for visual development is considered from birth to three months of age. However, some visual development continues until 7-8 years of life.
Amblyopia is the most common cause of preventable visual disability in children, occurring in approximately 2-5% of the general population.1 Awareness of this condition is important as nearly all amblyopic visual loss is preventable or reversible with appropriate intervention.
Aetiology
Amblyopia occurs when an ocular pathology (e.g. squint, high refractive error or deprivation) interferes with normal cortical visual development.
Classification
Amblyopia can be classified depending on the underlying pathology:
- Strabismic amblyopia: the most common form which develops in the consistently deviating eye of a child with ocular misalignment. For more information, see the Geeky Medics article on strabismus.
- Anisometropic amblyopia: develops when an unequal refractive error in the two eyes causes the image on one retina to be chronically defocused.
- Isometropia amblyopia: bilateral reduction in acuity that results from large approximately equal uncorrected refractive errors in both eyes of a young child causing blurred retinal images on both retinas.
- Deprivation amblyopia: usually caused by congenital or early acquired media opacities such as congenital cataracts or early-onset ptosis. This is the least common, but most damaging and difficult to treat amblyopia.
Clinical features
Amblyopia should be considered when there is reduced visual acuity which is not entirely explained by a structural eye problem.
History
Most cases of unilateral amblyopia are asymptomatic, as children do not notice the decreased visual acuity. In the United Kingdom, the majority of unilateral amblyopia is detected by vision screening programmes.
Children may present with clinical features of the cause of amblyopia (e.g. cataracts or early-onset ptosis).
Important areas to cover in the ophthalmic history include:
- Prematurity: squint is more common in premature children
- Family history: squint, glasses and amblyopia
Clinical examination
Clinical examination of children should consist of:
- Age-appropriate vision testing
- Recording the power of current spectacles
- Test of stereopsis and binocular function
- External examination looking for ptosis, large haemangiomas that can cause deprivation
- Relative afferent pupillary defect
- Anterior segment examination looking for media opacity
- Motility and ocular alignment
- Fundus examination
- Cycloplegic refraction
For more information, see the Geeky Medics OSCE guide to examining the eyes and vision.
Investigations
Amblyopia is usually a clinical diagnosis after appropriate history taking and examination and does not require investigations.
If the cause of amblyopia cannot be explained by clinical examination, or the vision is deteriorating despite treatment, then neuroimaging should be considered.
Management
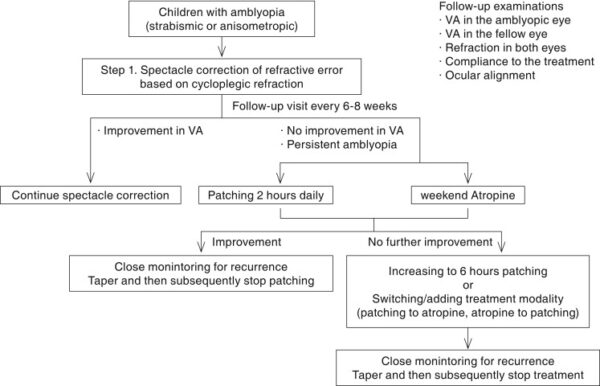
Treatment of amblyopia consists of:
- Eliminating, if possible, any obstacle to vision such as cataracts
- Correcting refractive error
- In unilateral/asymmetrical cases, forcing the use of the poorer eye by limiting the use of the better eye within the sensitive period of visual development.
Optical correction
Optical correction aims to provide a clear retinal image to each eye for children with amblyopia.
This is done by correcting the full refractive error as determined by cycloplegia. This is the first step in the management of amblyopia in all children.
Patching
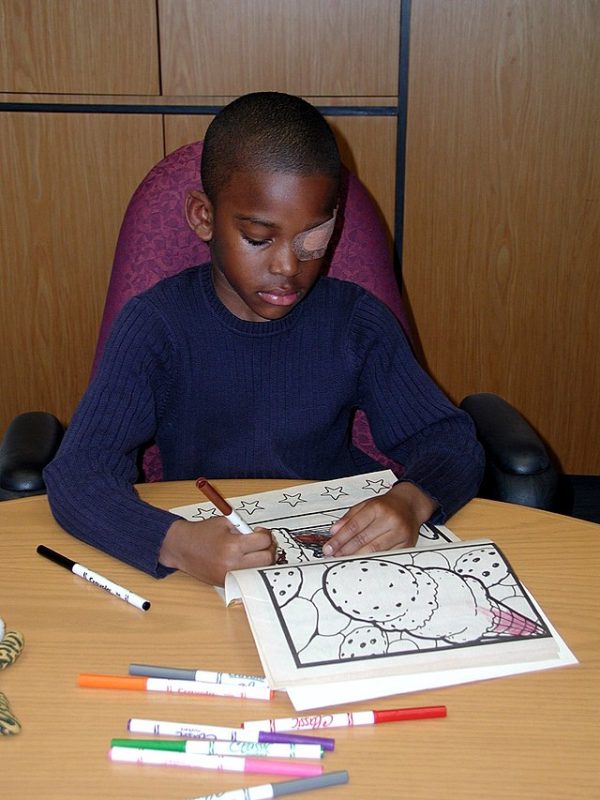
After providing full optical correction, full-time patching of the ‘good’ eye is the most effective means of treating amblyopia by forcing the use of the ‘weak’ eye. This is usually done with commercially available patches (Figure 1).
The duration of patching depends on the severity of the amblyopia and response to treatment:2.3
- Severe amblyopia (20/100 to 20/400): six hours per day of occlusion (similar efficacy to full-time occlusion)
- Moderate amblyopia (20/40 to 20/80): initially two hours per day of occlusion, increasing to six hours a day when vision in the amblyopia eye stops improving
Children treated with patching may develop occlusion amblyopia in the ‘good’ eye and therefore regular follow-up is required.
Patching compliance is a major concern with high rates of poor or no compliance in some studies. Compliance with therapy can be improved with educational programmes and effective communication with children and their parents.
Atropine penalisation
Atropine penalisation involves optical degradation of the ‘better’ eye image by using cycloplegic drops to force the child to use the weaker eye. It is an effective treatment in those who do not show an improvement with spectacles alone and who are uncooperative with patching.
Atropine 1% eye drops are used for this purpose and are most effective when the non-amblyopic eye is hyperopic.
Atropine is usually prescribed daily for amblyopia treatment. The cycloplegic effect of topical atropine usually lasts for several days.
Less frequent dosing of atropine may improve compliance with treatment. Studies have shown that magnitude of improvement was equal when using drops daily or at weekends only in children with moderate amblyopia.4
Complications
If left untreated amblyopia can result in permanent reduced visual acuity in children. Poor co-operation with patching is common. Rarely atropine drops can cause side effects such as flushing, tachycardia and photophobia.
Key points
- Amblyopia (lazy eye) is a unilateral or bilateral reduction in visual acuity due to an insult to the visual pathway in the critical period of visual development.
- Strabismic amblyopia is the most common form which develops in the consistently deviating eye of a child with ocular misalignment.
- Amblyopia should be considered when there is reduced visual acuity which is not entirely explained by a structural eye problem.
- Amblyopia is usually a clinical diagnosis after appropriate history taking and examination and does not require investigations.
- Treatment of amblyopia consists of eliminating any obstacle to vision (e.g. cataracts), correcting refractive error and forcing the use of the poorer eye by limiting the use of the better eye (e.g. patching).
- If left untreated amblyopia can result in permanent reduced visual acuity in children.
Reviewer
Mr Amit Gaur
Consultant Ophthalmologist
Editor
Dr Chris Jefferies
References
- Wallace D, Repka M, Lee K, Melia M, Christiansen S, Morse C et al. Amblyopia Preferred Practice Pattern®. Ophthalmology. 2018;125(1):P105-P142.
- A randomized trial of prescribed patching regimens for treatment of severe amblyopia in children. Ophthalmology. 2003;110(11):2075-2087.
- A Randomized Trial of Patching Regimens for Treatment of Moderate Amblyopia in Children. Archives of Ophthalmology. 2003;121(5):603.
- A randomized trial of atropine regimens for treatment of moderate amblyopia in children. Ophthalmology. 2004;111(11):2076-2085.e4.
Image references
- Figure 1. National Eye Institute, National Institutes of Health. Child eyepatch. License: [Public domain]
- Figure 2. Shin Hae Park / The Korean Ophthalmological Society. Current Management of Childhood Amblyopia. License: [CC BY-NC]




