- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
This article provides an overview of the anatomy of the hand, part of the Geeky Medics series covering the anatomy of the upper limb.
For an overview of clinical examination of the hands, see the Geeky Medics guide to hand and wrist examination.
Bones of the hand
To understand the anatomy of the hand we first must understand the anatomy of the forearm and wrist.
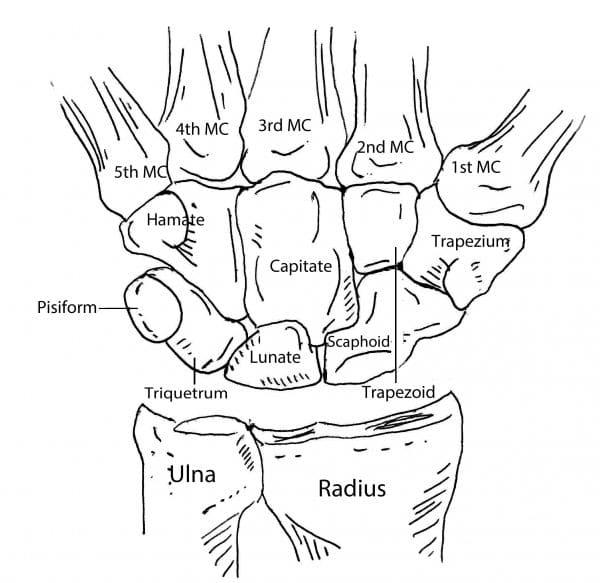
The forearm consists of two bones, the radius and the ulna. Both forearm bones articulate with the carpal bones of the wrist distally.
The radius articulates with the cashew shaped scaphoid bone, and the croissant or moon-shaped lunate bone.
The ulna articulates with the triquetrum, through a pad of intervening cartilage known as the triangular fibrocartilaginous complex. These three bones make up the proximal carpal row.
Five further carpal bones form the distal carpal row. The trapezium articulates with the first metacarpal, i.e. the thumb metacarpal (hence ‘trapezium with the thumb’).
Adjacent to this we have the trapezoid, which articulates with the second metacarpal. Superficial to the triquetrum, we have the pisiform, a pea-shaped sesamoid bone that lies within the tendon of flexor carpi ulnaris.
The capitate is adjacent and articulates with the third and fourth metacarpals. Finally, the hamate articulates with the fifth metacarpal. The hamate is easily identifiable by its ‘hook’ like volar projection.
The metacarpals articulate with the proximal phalanges, which articulate with the middle phalanges, which finally articulate with the distal phalanges.
The thumb has only a proximal and distal phalanx. It opposes the tips of the other fingers and is essential for precision grip. The thumb constitutes 70% of hand function, and a thumb injury can leave the patient debilitated, particularly if the dominant hand is injured.
For more information, see the Geeky Medics guide to the bones of the hand.
Muscles of the hand
Interossei muscles
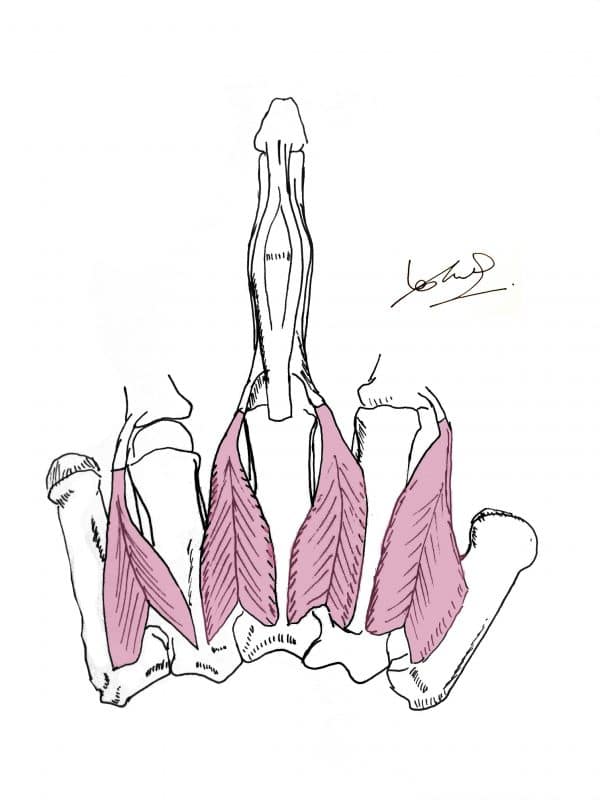
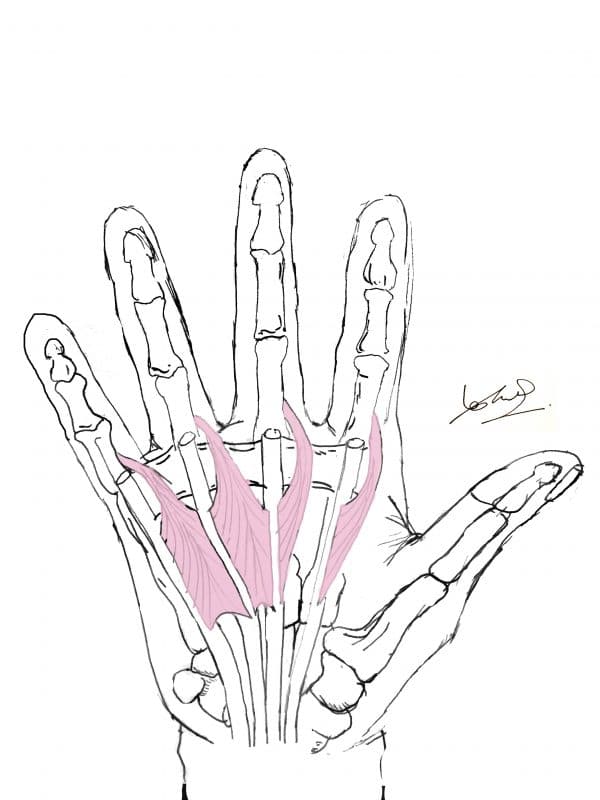
The interossei muscles are intrinsic hand muscles that originate from the intermediate surfaces of the metacarpals.
There are four dorsal and three palmar interossei muscles. They insert onto the proximal phalanx and extensor hood of each finger.
Palmar interossei ADduct the fingers, and dorsal interossei ABduct the fingers (hence PAD/DAB).
The radial artery enters the hand by passing between the two heads of the first dorsal interosseous.
Lumbricals
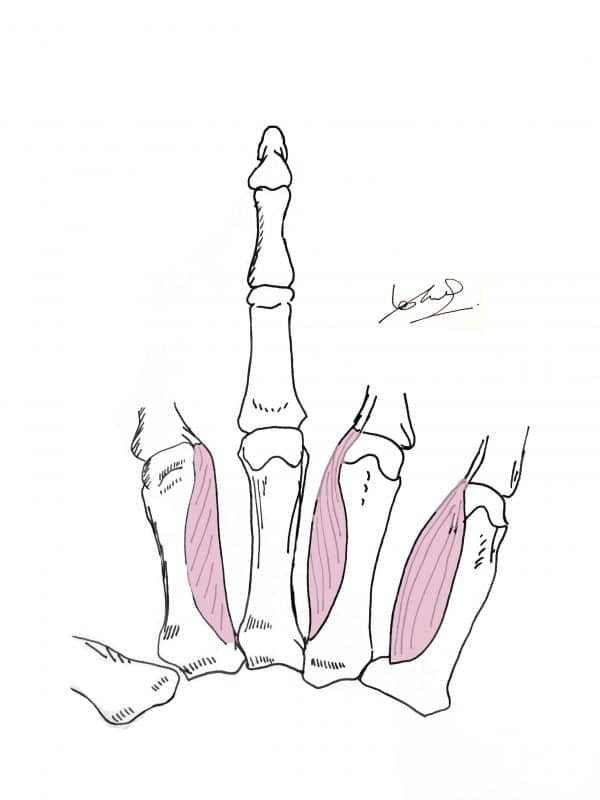
The four lumbricals are thin worm-like muscles that flex the metacarpophalangeal joints and extend the interphalangeal joints. They arise from the tendons of flexor digitorum profundus and are the only muscles in the human body to arise from the tendons of another muscle.
Thenar and hypothenar eminence
Thenar eminence (radial side)
There are three muscles that make up the thenar eminence.
Opponens pollicis is deep and helps the thumb in opposing the other digits.
Flexor pollicis brevis is on the ulnar side of the eminence and flexes the metacarpophalangeal joint of the thumb.
Abductor pollicis brevis is on the radial side of the eminence and works in conjunction with the abductor pollicis longus to abduct the thumb.
Hypothenar eminence (ulnar side)
In a similar fashion to the thenar eminence, the hypothenar eminence is formed by three muscles.
Opponens digiti minimi is deep and helps the little finger oppose the thumb.
Flexor digiti minimi is on the radial side of the eminence and flexes the metacarpophalangeal joint of the little finger.
Abductor digiti minimi is on the ulnar side of the eminence and abducts the little finger.
Nerves of the hand
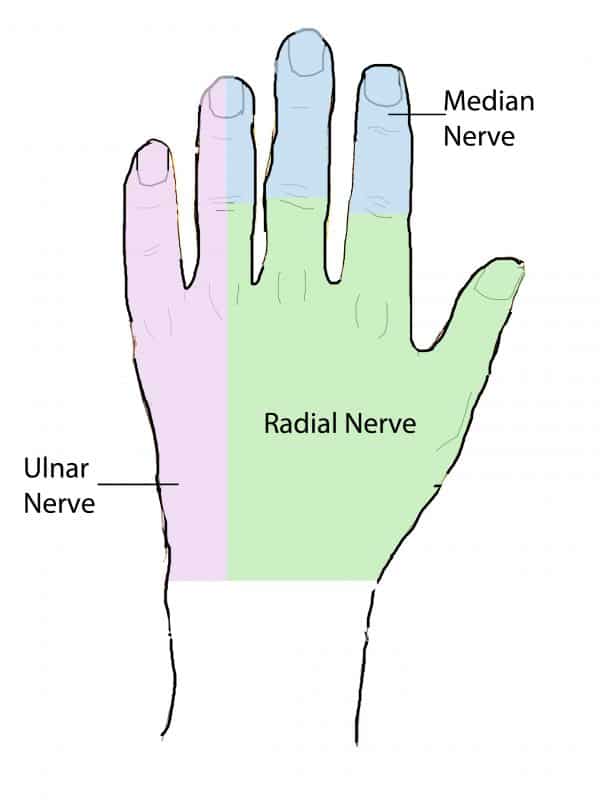
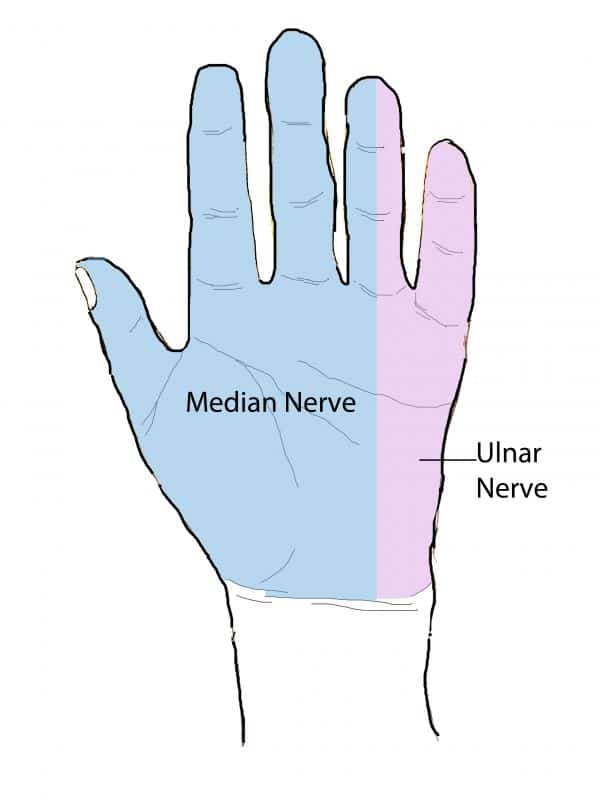
The ulnar nerve (C8-T1 nerve roots) arises from the medial cord of the brachial plexus and supplies all of the intrinsic muscles of the hand with a few exceptions. These are the muscles of the thenar eminence and the radial two lumbricals, which are supplied by the median nerve (C5-T1).
The median nerve supplies sensation to the radial three and a half fingers on the palmar aspect and the nail beds dorsally. This is through the proper digital nerves that run on either side of the fingers.
The median nerve also supplies the radial two-thirds of the palm through the palmar cutaneous branch. This nerve branches off before the median nerve passes through the carpal tunnel and is hence spared in carpal tunnel syndrome.
Sensation to the palmar and dorsal side of the ulnar one and half fingers is supplied by the sensory branches ulnar nerve. The radial nerve supplies sensation to the radial 3 and a half fingers and dorsal surface of the hand through its dorsal sensory branch.
For more information, see the Geeky Medics guide to the nerve supply of the upper limb.
Blood supply and drainage of the hand
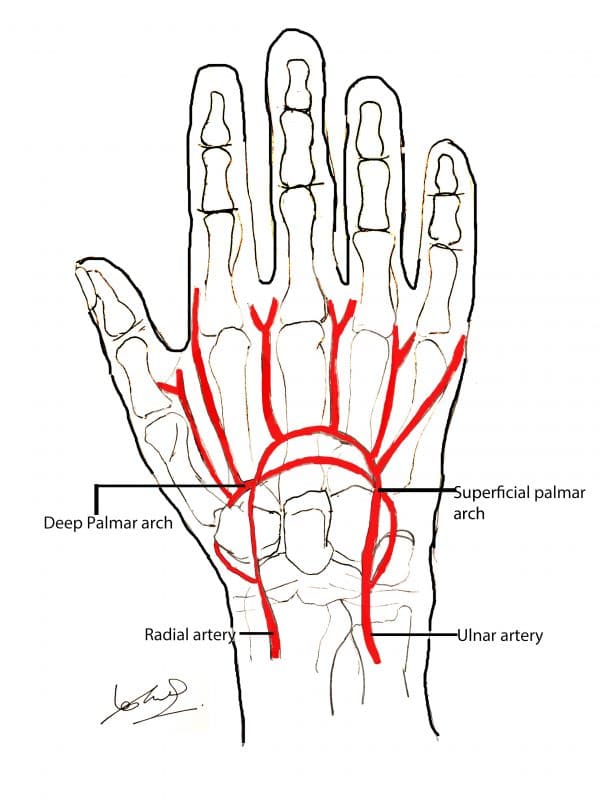
The superficial palmar arch is the main continuation of the ulnar artery. It receives a small superficial branch from the radial artery and supplies the fingers with blood via the common digital, and the distal ‘proper digital arteries’ which run on either side of the finger.
The thumb and radial side of the index finger are exceptions, as they receive branches directly from the radial artery before it forms the deep palmar arch in the hand.
The deep palmar arch is the main branch of the radial artery and supplies the deep hand structures.
Paired veins accompany the arterial arches and share the same names (i.e. radial and ulnar). The more superficial cephalic and basilic veins drain the dorsal venous network of the hand.
Clinical relevance
Carpal tunnel syndrome
If the median nerve becomes compressed within the carpal tunnel, there is paraesthesia in the radial three and a half fingers as well as thenar muscle wasting in late-stage disease.
Patients will often complain of tingling in the hand, and pain after using their affected hand. Treatment options include steroid injections, physiotherapy, and carpal tunnel release. For more information, see the Geeky Medics guide to carpal tunnel syndrome.
Ulnar paradox
Usually, the more proximal a nerve injury, the worse the resulting function of the body. The opposite is true when we consider the ulnar nerve. This is because one of the muscles that flexes the fingers (flexor digitorum profundus, which lies in the forearm) is partially innervated by it.
Hence a proximal injury will remove innervation to the forearm muscles and the hand muscles.
A distal injury only takes out the hand muscles; hence the still functioning finger flexors give the patient a clawed appearance in the ring and little finger.
With a proximal injury leading to an open palm, there is more capacity for functional grip and use of the hand.
Dupuytren’s contracture
The palmar aponeurosis is a thick area of fascia that is tightly attached to the skin. Dupuytren’s contracture is caused by a proliferation of type three collagen within the palmar fascia. It causes the palmar aponeurosis to thicken and contract, causing the little and ring finger to flex abnormally.
Treatment of Dupuytren’s contracture includes physiotherapy and splinting with steroid injections if still in its initial stages, and surgical excision of the bands for advanced cases.
Hand fractures
Fractures involving the bones of the hand can result in significant dysfunction. The decision on whether to treat conservatively or with surgery is dependent on both the appearance of the hand due to the injury, as well as the function of the hand as a motor and sensory unit.
If a fracture results in rotation of a finger to an unacceptable degree or is unstable due to its very nature (e.g. an oblique fracture or fracture involving the endplate of the bone within a joint), it is likely to require repair.
An example of a fracture that is usually managed conservatively, is the ‘boxer’s fracture’, a transverse fracture of the distal fifth metacarpal shaft.
Editor
Dr Chris Jefferies