- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Down’s syndrome (trisomy 21) is the most common chromosomal abnormality. In England in 2020, 1 in 377 babies were diagnosed with Down’s syndrome.1
Down’s syndrome has a variable spectrum and can be associated with delayed developmental milestones, congenital heart defects and gastrointestinal tract anomalies.2,3 It is impossible to predict or know the severity of manifestations before birth.
Antenatal screening for Down’s syndrome forms part of the NHS Fetal Anomaly Screening Programme (FASP) and is offered to all pregnant women between 10+0 and 20+0 weeks of pregnancy.4 Nearly two-thirds of babies with congenital anomalies were detected antenatally.1
The type of screening for Down’s syndrome offered is based on fetal gestation:4
- Women presenting between 10+0 weeks to 14+1 weeks gestation will be offered the combined test
- If a woman presents late with gestation between 14+2 and 20+0 weeks or if the nuchal translucency measurement as part of the combined test cannot be obtained, women are offered the quadruple test
Combined test
The NHS FASP first trimester combined screening test is the combined test. The combined test assesses the chance of the fetus having Down’s syndrome (trisomy 21), Edward’s syndrome (trisomy 18) or Patau’s syndrome (trisomy 13).5 It uses maternal and fetal measurements.
Maternal measurements
Maternal age
The chance of a woman having a baby with trisomy 21 increases with maternal age:1,5
- Maternal age of 20: 1 in 1500 chance
- Maternal age of 30: 1 in 900 chance
- Maternal age of 40: 1 in 100 chance
Free beta human chorionic gonadotropin (bhCG)
An increased level of bhCG in maternal blood in the first trimester is associated with Down’s syndrome. Conversely, a decreased level is associated with Edwards’ and Patau’s syndrome.5,6
Pregnancy-associated plasma protein-A (PAPP-A)
A decreased level of PAPP-A in maternal blood in the first trimester is associated with Down’s syndrome (trisomy 21), Edwards’ syndrome (trisomy 18) and Patau’s syndrome (trisomy 13).5,6
Fetus via ultrasound measurements
Nuchal translucency (NT)
Ultrasound is used to assess the thickness of the nuchal pad at the nape of the fetal neck. Increased NT is associated with Down’s syndrome.2,5
The nuchal translucency must be combined with the maternal blood sample and cannot be used alone to calculate the result.
If NT cannot be measured, at least one more attempt is offered ‘twice on the couch’ either on the same day or later, based on local guidelines. If NT still cannot be measured after a second attempt, women are offered the quadruple test.
Crown-rump length (CRL)
This is measured to check eligibility for the combined test (45.0-84.0mm) and is a more accurate measurement of fetal gestational age than the last menstrual period.5
If the CRL is <45mm, women are asked to attend another ultrasound scan to remeasure CRL and NT.
If the CRL is >84mm, a combined screening test can not be performed. The gestational age is calculated using head circumference, and the women may be offered a quadruple test if measurements suggest greater than 14+1 weeks gestation.
Quadruple test
The quadruple test only screens for Down’s syndrome and is offered during the second trimester (14+2 to 20+0 weeks) when NT measurement cannot be obtained after two attempts or if ultrasound measurements suggest gestation greater than 14+1 weeks.5
Table 2. Quadruple test measurement results associated with Down’s syndrome.5,7
| Measurements | Results associated with Down’s syndrome |
| Maternal age | Increased maternal age |
| Alpha-fetoprotein (AFP) | Low |
| Human chorionic gonadotropin (hCG) or free bhCG | High |
| Inhibin-A | High |
| Unconjugated oestriol (uE3) | Low |
The quadruple test has a lower detection rate and higher screen positive rate than the combined test, therefore, is less accurate.
Maternal factors can affect maternal blood markers (e.g. smoking). Therefore, a thorough history is required during the appointment and noted with samples for interpretation.
Screening results
The chance cut-off is 1 in 150 at term for both combined and quadruple tests:
- A lower chance test is less than or equal to 1 in 151
- A higher chance result is greater than or equal to 1 in 150 (between 1 in 2 and 1 in 150)
The cut-off is based on the chance at term, not chance at the time of screening test due to high unknown pregnancy loss between screening time and birth.
Following a higher chance result, women can choose to have:
- No further testing
- Non-invasive prenatal testing (NIPT)
- Prenatal diagnostic testing
Non-invasive prenatal testing (NIPT)
This non-invasive test is a blood test which assesses placental cell-free fetal DNA found in maternal blood and combines this with the mother’s background probability of a trisomy (mother’s age or the combined test results offered within the NHS) to obtain a likelihood ratio to predict whether or not the baby is more likely to have a chromosomal condition such as Down syndrome. A result is provided of the chance of a baby likely having Down’s syndrome, Edwards’ syndrome or Patau’s syndrome.
NHS screening recommends offering NIPT screening for trisomy conditions following a higher chance result of a combined or quadruple test. The detection rates for trisomy 21 using NIPT can be as high as 99%, depending on fetal fraction. Nevertheless, it should be considered a screening test only, and any positive test results need to be confirmed by an invasive prenatal diagnostic test (e.g. chorionic villus sampling or amniocentesis).
The test is suitable from 10 weeks of gestation onwards. The test is unsuitable for triplets or higher-order pregnancies if the mother has cancer, or a chromosomal or genetic condition (including Down’s syndrome). It is not recommended for mothers who have undergone a blood transfusion in the last 4 months or had transplant surgery, immunotherapy or stem cell therapy, as these factors are likely to interfere with results.
This test has the potential to screen for other chromosomal conditions and assess the baby’s sex, but this is not offered as part of the NHS pathway.
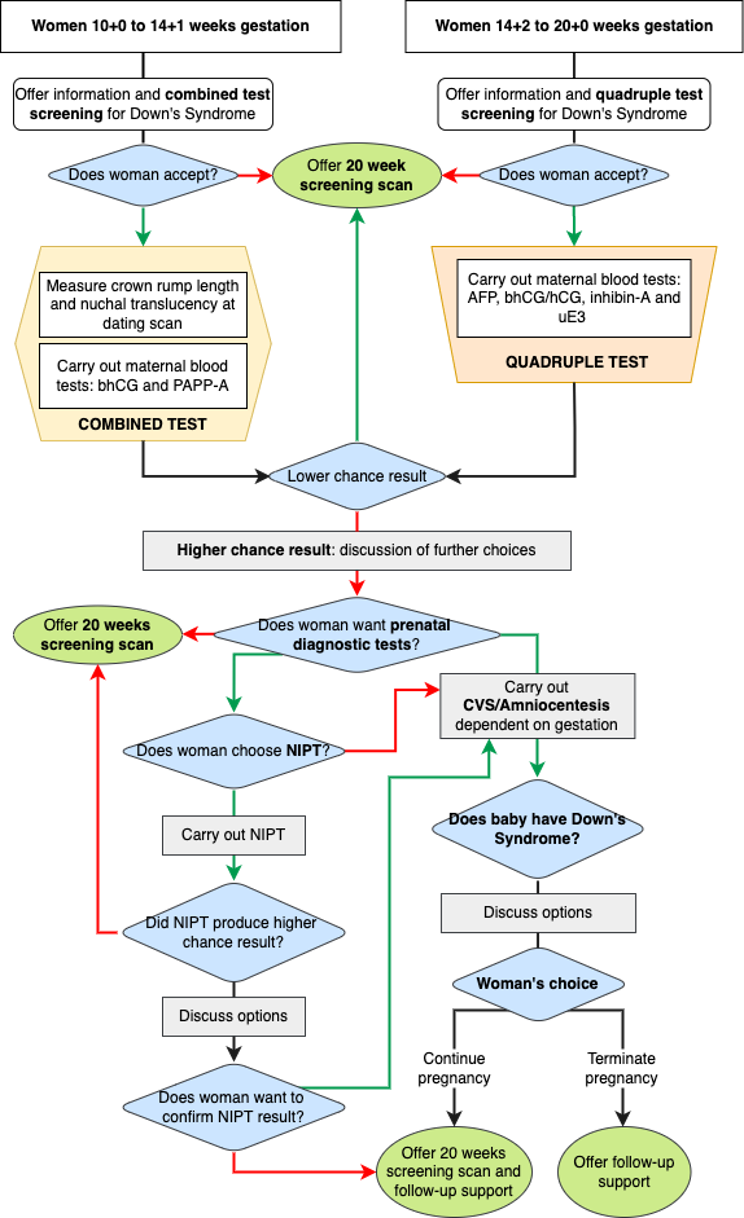
Prenatal diagnostic test
A prenatal diagnostic test is offered to all pregnant women with a higher chance test result for Down’s syndrome, Edwards’ syndrome or Patau’s syndrome, or if there are any unexpected ultrasound findings on an anomaly scan.
This testing is an invasive procedure and, dependent on fetal gestation, will be either chorionic villus sampling (CVS) or amniocentesis.
Women who are rhesus negative will be recommended to have an anti-D immunoglobulin injection after the procedure to prevent developing antibodies.9
Chorionic villus sampling (CVS)
CVS is indicated at 11-14 weeks gestation and involves the ultrasound-guided sampling of placental tissue by inserting a fine needle through the abdomen and into the uterus.9 A transabdominal approach is the most common method. However, transcervical CVS may be indicated based on placenta location, but there is a higher likelihood of vaginal bleeding post-procedure.9,10
A rapid CVS result is available around three days after the procedure, and the second CVS result is provided within two weeks.9 The second result focuses on the baby’s DNA and rules out placental mosaicism, which implies that the genetic makeup of the placenta is different to that of the baby. Mosaic results on the CVS sample warrant a further confirmatory amniocentesis.11
Amniocentesis
Amniocentesis can be performed >15 weeks of gestation and involves the ultrasound-guided insertion of a fine needle through the abdomen and into the uterus to take a sample of amniotic fluid.9 The amniotic fluid contains the baby’s cells and is a true reflection of the baby’s DNA. The ease of the procedure is dependent on the position of the baby and the placental location.
Risks
Women should be counselled that the procedures are uncomfortable; some have described it as period pain. Cramping is common after the procedure.
NHS England quotes a 1 in 200 miscarriage risk of CVS or amniocentesis. Miscarriage mostly occurs within three days of the procedure but can occur up to two weeks afterwards.9 However, this risk is negligible compared to women of the same risk profile not undertaking the procedure.12
There is a less than 1 in 1000 risk of a serious infection, and women are advised to return if they experience severe pain, high temperature, heavy vaginal bleeding or contractions.9
Prenatal diagnosis results
If the result is positive for the baby having Down’s syndrome, women are supported by an obstetrician and/or midwife who explain the results. A consultant paediatrician, consultant geneticist or genetic counsellor can offer additional support.
Women have the choice to continue with the pregnancy or end the pregnancy. This decision is very personal to the women. If the woman decides to continue with the pregnancy, specialised support is provided to discuss the woman’s care and preparation of care for the baby. Women who chose to continue should be signposted to support groups. If the woman decides to end the pregnancy, both medical/surgical options for termination of pregnancy should be offered.
Anomaly scan
The anomaly scan offered between 18+0 and 20+6 weeks screens for 11 physical conditions. Some conditions are associated with Down’s syndrome, such as congenital heart disease and abdominal wall defects.13
However, it must be explained to women that fetuses with trisomy 21 may not have abnormalities detectable on antenatal ultrasound. This is in contrast to trisomy 13/18, where the prevalence of structural anomalies is very high on prenatal ultrasound.
This scan is offered to women who do not want screening tests or prenatal diagnostic testing and wish to continue with the pregnancy.
Twin pregnancies
The test of choice is the combined test. In a monochorionic twin pregnancy, the chance result is the same for each baby and one ‘pregnancy’ chance result is reported. In a dichorionic baby, each baby’s chance result is reported.8 Emerging research suggests that NIPT can be offered to women with twin pregnancies, regardless of chorionicity, as a screening test.
Prenatal diagnostic testing is more complicated in twin pregnancies and should be performed in specialist tertiary units. The risk of miscarriage following CVS or amniocentesis is twice as high as in singleton pregnancies and may lead to miscarriage of both babies.14
Reviewer
Dr Smriti Prasad
Fetal Medicine Clinical Research Fellow
St George’s University Hospital NHS Trust
Editor
Dr Chris Jefferies
References
- National Congenital Anomaly and Rare Disease Registration Service. Congenital Anomaly Official Statistics Report, 2020. Reviewed February 18, 2023. Available from: [LINK]
- Geeky Medics. Down’s Syndrome. Published in 2022. Available from: [LINK]
- The University of Chicago Pediatrics Clerkship. Trisomy 21 (Down). Published in 2013. Available from: [LINK]
- Public Health England. NHS Fetal Anomaly Screening Programme (FASP): programme overview. Reviewed January 23, 2023. Available from: [LINK]
- NHS England. Screening for Down’s syndrome, Edwards’ and Patau’s syndrome. Reviewed January 23, 2023. Available from: [LINK]
- Palomaki GE et al. A summary analysis of Down syndrome markers in the late first trimester. Published in 2007. Available from: [LINK]
- Alldred SK et al. Cochrane Database System Review. Second trimester serum tests for Down’s Syndrome screening. Published in 2012. Available from: [LINK]
- NHS England. Screening for Down’s syndrome, Edwards’ syndrome and Patau’s syndrome: non-invasive prenatal testing (NIPT). Reviewed January 23, 2023. Available from: [LINK]
- Public Health England. Screening in pregnancy: CVS and amniocentesis information for parents. Reviews January 23, 2023. Available from: [LINK]
- Stergiotou et al. Transcervical chorionic villus sampling: a practical guide. Published in 2016. Available from: [LINK]
- Kalousek and Vekemans. Confined placental mosaicism. Published in 1996. Available from: [LINK]
- Salomon et al. Risk of miscarriage following amniocentesis or chorionic villus sampling: systematic review of literature and updated meta-analysis. Published in 2019. Available from: [LINK]
- Stoll et al. Associated congenital anomalies among cases with Down syndrome. Published in 2015. Available from: [LINK]
- Khalil et al. Noninvasive prenatal screening in twin pregnancies with cell-free DNA using IONA test: a prospective multicenter study. Published in 2021. Available from: [LINK]




