- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Uveitis describes inflammation of the uveal tract, comprising the iris, ciliary body, and choroid.
Anterior uveitis (inflammation of the iris and ciliary body) is the most common form, accounting for 50% of cases. It typically presents as a painful, photophobic red eye.
In the UK, there are 25-50 cases of uveitis per 100,000 persons, with a mean age onset of 31.
Aetiology
Uveitis is caused by an inflammatory response however the exact pathophysiology is unclear.
The majority (50%) of cases are idiopathic. However, uveitis may occur as part of a systemic disease process:
- HLA-B27 genotype-associated disease: inflammatory arthropathies (ankylosing spondylitis, reactive arthritis, psoriatic arthritis) and inflammatory bowel diseases (Crohn’s disease, ulcerative colitis)
- Other autoimmune/inflammatory diseases: interstitial nephritis, sarcoidosis, vasculitis
- Infections: toxoplasmosis (most common), herpes simplex, herpes zoster, cytomegalovirus, tuberculosis, lyme disease, HIV and syphilis
- Traumatic
- Iatrogenic: surgery, medications (bisphosphonates, sulphonamides, rifabutin, cidofovir)
- Cancer: leukaemia, lymphoma, malignant melanoma
Uveitis can be classified by location as well as onset (sudden, insidious), duration (limited, persistent) and course (acute, recurrent, chronic).
Anatomy
The eye is made up of three layers:
- Outer: cornea and sclera
- Middle: uvea
- Inner: retina
The uveal tract comprises the iris, ciliary body, and choroid (Figure 1). For more information, see the Geeky Medics guide to the anatomy of the eye.
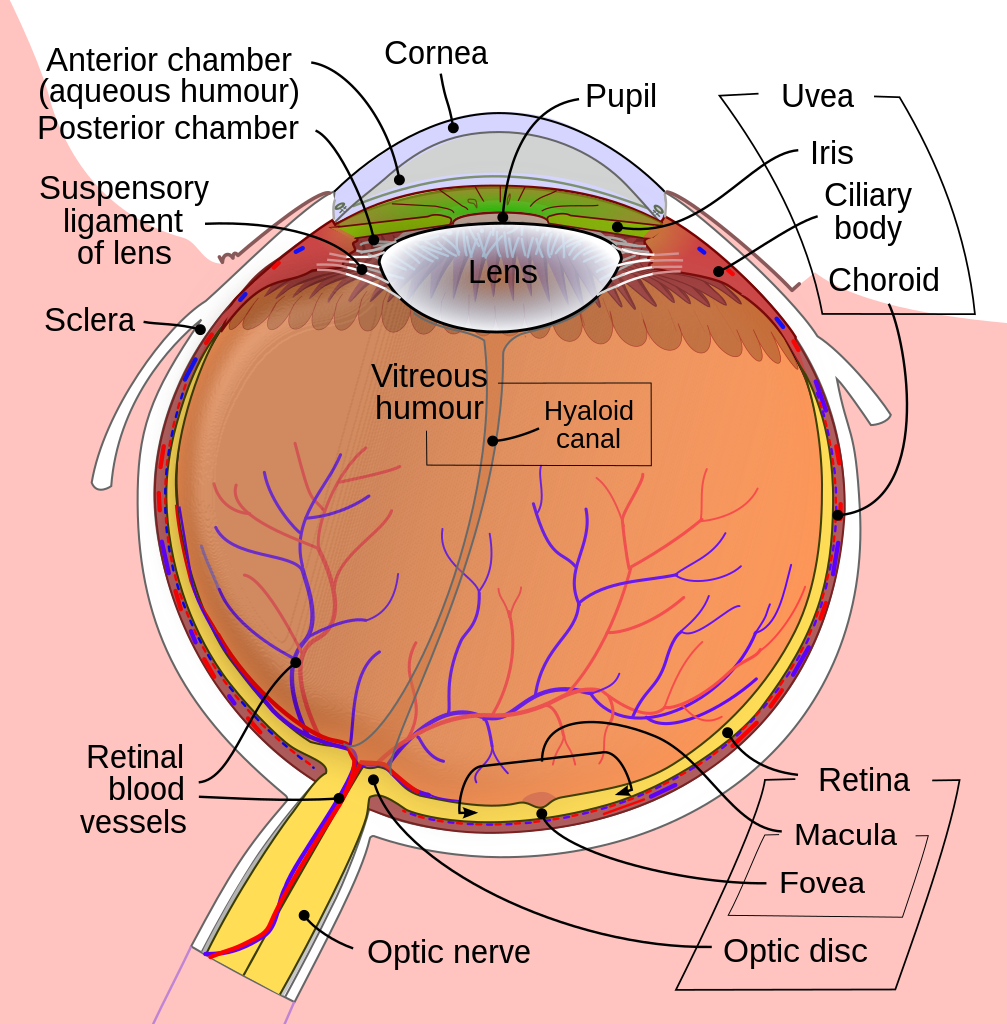
Anterior uveitis is inflammation of the iris and ciliary body. Anterior uveitis is synonymous with iritis, which only affects the iris and iridocyclitis, which affects the iris and ciliary body.
Risk factors
Risk factors for uveitis include:
- Aged over 20 (accounts for >90% of uveitis)
- Previous history of uveitis
- HLA-B27 positive
Clinical features
History
For acute anterior uveitis, symptoms can develop quickly over a few hours or more gradually over several days.
A bilateral presentation is commonly seen in systemic conditions, whereas idiopathic or herpetic uveitis is unilateral. These can then progress to be bilateral.
Typical symptoms of acute anterior uveitis include:
- Painful eye
- Red eye
- Photophobia
- Tearing
There may also be associated systemic features including:
- Joint pain
- Back pain
- A flare-up of inflammatory bowel disease
- Infective symptoms (fever, malaise, anorexia)
Chronic uveitis or intermediate and posterior uveitis can present more atypically with painless decreased vision.
Clinical examination
Uveitis can be difficult to evaluate without a slit lamp however a pen torch examination can give clues towards this diagnosis.
Typical clinical findings on general examination may include:
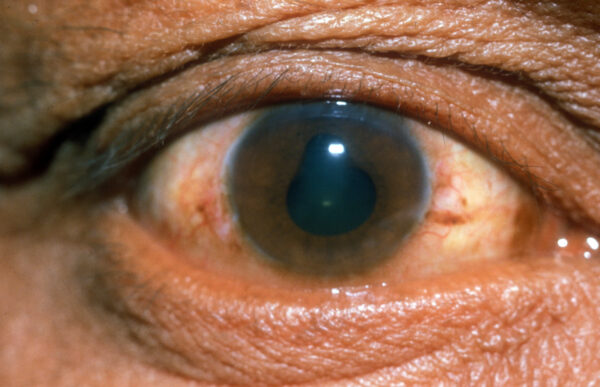
- Ciliary injection: dilated conjunctival vessels concentrated around the border of the cornea
- An irregular pupil: due to posterior synechiae (attachment of the iris to the lens capsule)
- Cloudy cornea and hazy view of the iris: due to cells in the aqueous humour and corneal oedema
- Hypopyon: an inferior settled layer of ‘pus’ (white cells and debris)
Clinical findings on slit lamp examination may include:
- Circumferential redness (ciliary flush) at the corneal limbus (junction of the cornea and sclera) due to an inflamed ciliary body
- Inflammatory cells in the anterior chamber
- Smokey/foggy appearance of the anterior chamber (referred to as “flare”)
- Adhesions between the lens and pupil, which distort the shape of the pupil (posterior synechiae)
Differential diagnoses
There is a wide differential for painful red eye. These include:
- Acute angle closure glaucoma: confirmed with tonometry, may have a mid-dilated fixed pupil
- Scleritis/episcleritis: can present with similar symptoms but differentiated with slit lamp examination
- Infective keratitis: cornea damage would be seen with fluorescein drops under cobalt blue light
- Infectious conjunctivitis: similar presentation however, photophobia would not be present
- Corneal foreign body/trauma: cornea damage would be seen with fluorescein staining, may present with or without uveitis
- Endophthalmitis: a much greater degree of inflammatory cells seen in anterior and posterior chambers
- Post-surgical anterior segment inflammation
For more information on differential diagnoses, see the Geeky Medics guide to the painful red eye.
Investigations
Bedside investigations
Relevant bedside investigations include:
- Urinalysis: to investigate for systemic vasculitis
Laboratory investigations
Laboratory investigations depend on the suspected underlying cause of uveitis. If it is the first presentation and unilateral, a systemic workup is usually not required.
Bilateral disease or systemic features require further investigation.
Relevant laboratory investigations include:
- Baseline blood tests: FBC, U&E, LFTs
- Inflammatory markers: CRP & ESR
- HLA-B27 testing
- Antinuclear antibodies (ANA)
- Serum ACE
- Infectious disease screen: tuberculosis, syphilis, toxoplasmosis, lyme disease, HIV
Imaging
Imaging investigations depend on the suspected underlying cause.
Relevant imaging investigations may include:
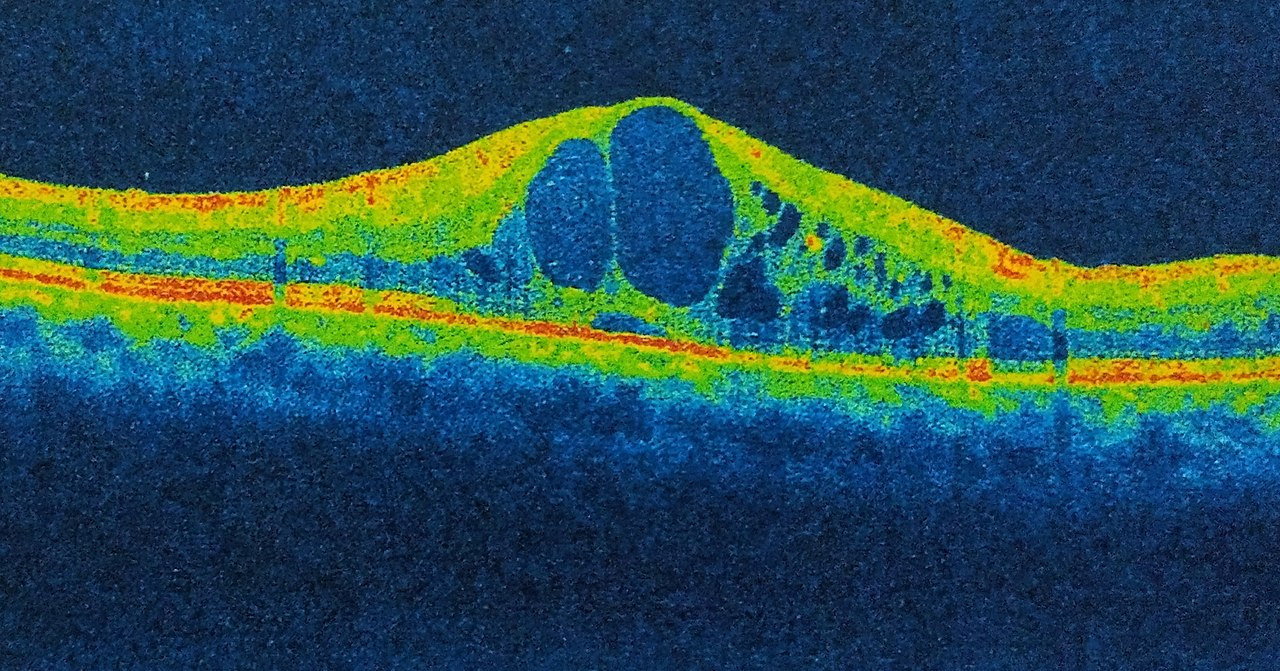
- Optical coherence tomography (OCT): to assess for macular oedema
- Chest X-ray: tuberculosis, sarcoidosis
- Spinal X-ray: ankylosing spondylitis
Diagnosis
Uveitis is a clinical diagnosis. The severity can be assessed using the Standardization of Uveitis Nomenclature (SUN) working group grading scheme.
The severity of uveitis is based on the appearance of the anterior chamber (number of inflammatory cells and grading of flare).
Management
Suspected uveitis should be referred to an ophthalmologist for assessment within 24 hours.
Treatment aims to control inflammation, prevent visual loss and minimise long-term complications of the disease and its treatment.
Treatment options include:
- Topical steroid drops to reduce inflammation (frequency depending on severity)
- Pupil dilating drops (e.g. cyclopentolate) to alleviate symptoms of photophobia
- Treatment of the underlying cause (e.g. antimicrobials for infections)
In severe cases, systemic treatment may be required:
- Systemic steroids: oral, intravenous, peri-ocular or intra-ocular may be required
- Systemic immunosuppressants (e.g. methotrexate, mycophenolate, adalimumab)
Complications
Most cases of uveitis are mild and temporary.
However, in severe cases, there may be vision loss. The most common causes for this are macular oedema and secondary cataract. There may also be an acute rise in intraocular pressure (IOP) either by inflammation of the trabecular meshwork or inflammatory closure of the drainage angle of the eye.
Prognosis
Anterior uveitis can be a self-limiting condition. With effective treatment, there are usually good visual outcomes. Relapse after the first episode is common in young patients (18-35 years).
Key points
- Anterior uveitis is inflammation of the iris and ciliary body
- 50% of cases are idiopathic; however, anterior uveitis may be associated with spondyloarthropathies, inflammatory bowel disease and infections
- Typical symptoms are a painful red eye which is photophobic
- Anterior uveitis is a clinical diagnosis based on history and slit lamp examination
- Investigations (including blood tests, urinalysis and imaging) should be considered if there is a suspected underlying systemic condition
- Acute anterior uveitis is a sub-acute condition and requires prompt review by ophthalmology
- The mainstay of treatment is with steroid eye drops, however, systemic steroids may be required for severe cases
- Most cases of anterior uveitis are mild and temporary, with good visual outcomes
Reviewer
Dr Nick Woo
ST5 in Ophthalmology
Editor
Dr Chris Jefferies
References
Reference texts
- BMJ Best Practice. Uveitis – Symptoms, diagnosis and treatment. 2021. Available from:[LINK]
- Salmon. Chapter 12, Uveitis. Kanski’s Clinical Ophthalmology 9th edition. 2020.
- MSD Manual Professional Edition. Overview of Uveitis – Eye disorders. Available from: [LINK]
- DynaMed. Anterior Uveitis. 2018. Available from: [LINK]
- NICE CKS. Uveitis. 2021. Available from: [LINK]
Image references
- Figure 1. Rhcastilhos, Jmarchn. Schematic diagram of the human eye. License: [CC BY-SA]
- Figure 2. International Centre for Eye Health. Posterior Synechiae – a sign of uveitis. License: [CC BY-NC]
- Figure 3. Imrankabirhossain. Cystoid macular edema (CME). License: [CC BY-SA]