- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
A heart murmur is a sound produced due to turbulent blood flow within the heart. This article will cover the clinical features of common heart murmurs and the underlying aetiology. For more information on cardiac auscultation, see the Geeky Medics OSCE guides to cardiovascular examination and paediatric cardiovascular examination.
The cardiac cycle
The cardiac cycle refers to a series of physiological events making up a single heartbeat. The cycle involves contraction (systole) and relaxation (diastole) of the atria and ventricles to effectively pump blood.
The cardiac cycle starts with the atria and ventricles in diastole. Blood enters the right atrium (from the vena cava) and the left atrium (from the pulmonary vein). At this point, the mitral and tricuspid valves are open. This allows blood to flow freely into the right ventricle and left ventricle from the atria. The aortic and pulmonary valves are shut, which prevents an abnormal backflow of blood into the ventricles from the aorta and pulmonary artery.
The next stage of the cycle is atrial systole, contraction of the atria to finish “filling” the ventricles with blood.
Ventricular systole occurs as the ventricles contract, increasing the pressure within the ventricles. The increased pressure causes the closure of the mitral and tricuspid valves, this prevents regurgitation of blood from the ventricles into the atria.
At this point, the volume of blood within the ventricles remains constant as the aortic and pulmonary valves have not yet opened. This phase of ventricular systole is called isovolumetric contraction.
Eventually, the pressure within the ventricles exceeds the pressure in the pulmonary artery and aorta causing the pulmonary and aortic valves to open. Blood is ejected from the ventricles during ventricular ejection phase.
The ventricles then begin to relax following contraction (ventricular diastole). The drop in pressure within the ventricle causes the aortic and pulmonary valves to close, to prevent backflow (regurgitation) of blood into the ventricles.
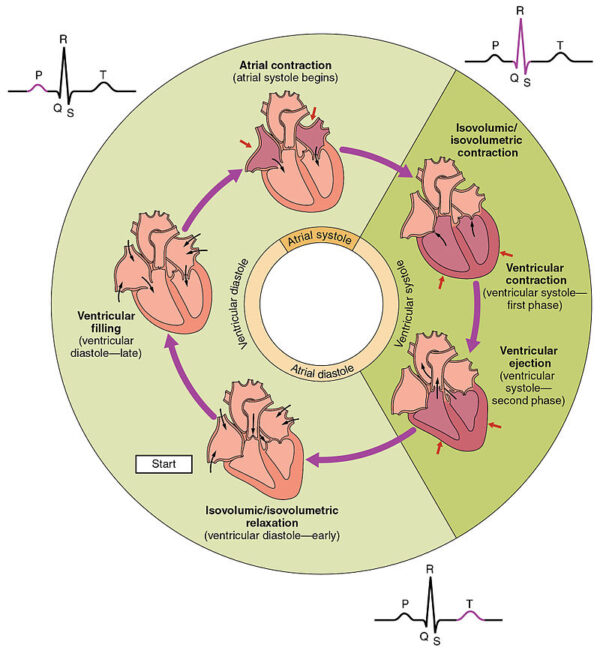
For more information, see the Geeky Medics guides to the cardiac cycle and electrical conduction system of the heart.
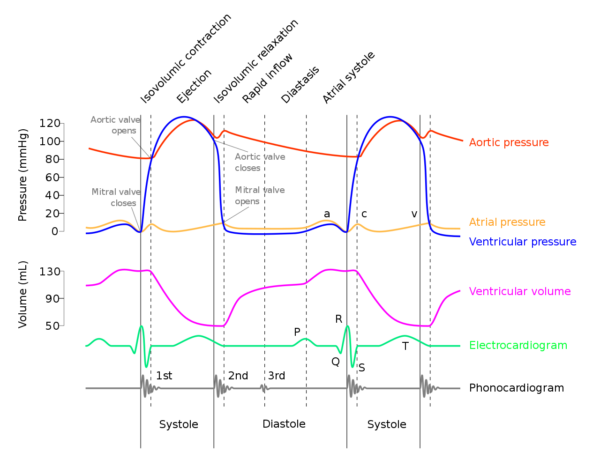
Normal heart sounds
Normal heart sounds are caused by the closure of heart valves.
First heart sound (S1)
The first heart sound (S1) is caused by the closure of the mitral and tricuspid valves. It marks the start of ventricular systole, and a peripheral pulse is felt at the same time (or shortly after) S1.
Second heart sound (S2)
The second heart sound (S2) is caused by the closure of aortic and pulmonary valves. It marks the end of ventricular systole and the start of diastole.
The pulmonary valve may close just after the aortic valve. Closure of the pulmonary valve just after the aortic valve is prolonged during inspiration, or in defects which cause more blood to be pumped out of the right ventricle.
Therefore, S2 may not always be heard as one discrete sound but may be muffled or have two discrete sounds (split S2).
Heart sounds and the cardiac cycle
How to approach heart murmurs
It is important to have a structured approach to interpreting heart murmurs during a cardiovascular examination.
If a murmur is heard during auscultation, consider the following questions:
- When during the cardiac cycle is the murmur heard?
- What are the characteristics of the murmur? What is the intensity (Table 1)?
- Is the murmur heard loudest using the bell or the diaphragm of the stethoscope?
- Where is the murmur heard the loudest?
- Do any manoeuvres exaggerate the murmur?
- Heard loudest on inspiration or expiration?
- Does the murmur radiate?
Table 1. The Levine scale for grading cardiac murmurs according to intensity.3
| Grade | Description |
| One | Very faint. Heard by an expert in optimum conditions |
| Two | Heard by a non-expert in optimum conditions |
| Three | Easily audible, no thrill |
| Four | A loud murmur, with a thrill |
| Five | Very loud, often heard over a wide area, with thrill |
| Six | Extremely loud, heard without a stethoscope |
A thrill is a palpable vibration caused by turbulent blood flow through a heart valve. Thrills may be felt when palpating the anterior chest wall during cardiovascular examination.
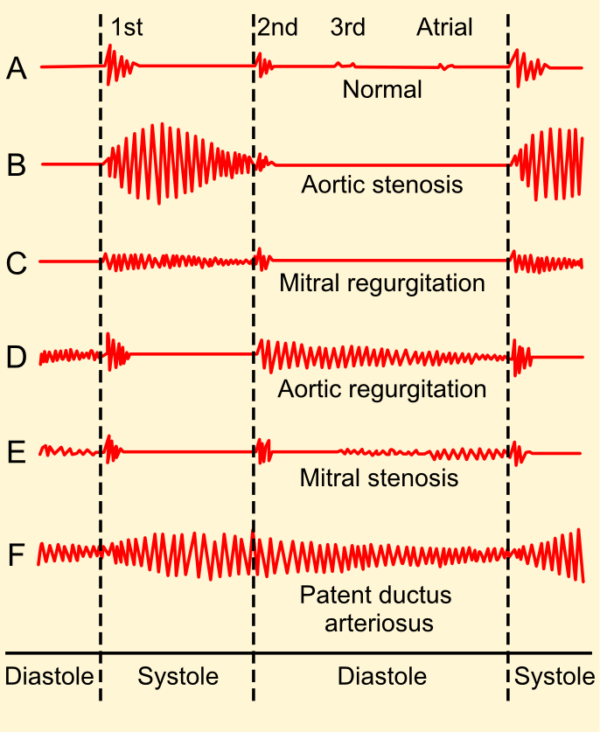
Aortic stenosis
Aortic stenosis (AS) refers to a tightening of the aortic valve at the origin of the aorta.
Aortic stenosis is associated with an ejection systolic murmur heard loudest over the aortic valve. The murmur is described as having a ‘crescendo-decrescendo’ quality (it appears as diamond-shaped on a phonogram). The murmur of aortic stenosis commonly radiates to the carotid arteries.
Aetiology
Causes of aortic stenosis include:
- Calcification of the aortic valves: this is the most common cause of AS in developed countries, typically occurring in elderly adults.
- Congenital abnormality of the aortic valve: the aortic valve is normally composed of three cusps (known as a tricuspid valve), but in some cases, individuals have only two cusps (known as a bicuspid valve) which predisposes them to the development of AS as well as aortic regurgitation.
- Rheumatic heart disease: a rare cause of AS in developed countries.
Clinical features
Typical features of an aortic stenosis murmur include:
- Ejection systolic murmur heard loudest over the aortic area
- Radiates to the carotid arteries
- Loudest on expiration and when the patient is sitting forwards
Other clinical features of aortic stenosis may include:
- Slow rising pulse with narrow pulse pressure
- Non-displaced, heaving apex beat (if present indicates left ventricular hypertrophy)
- Reduced or absent S2 (a sign of moderate-severe aortic stenosis)
- Reverse splitting of S2: aortic valve closes after pulmonary valve (due to the longer time required for blood to exit the left ventricle)
For more information, see the Geeky Medics guide to performing a focussed aortic stenosis examination.
Mitral regurgitation
Mitral regurgitation (MR) occurs when there is backflow (regurgitation) of blood from the left ventricle into the left atria (through the mitral valve) during ventricular systole.
Mitral regurgitation is associated with a pansystolic murmur heard loudest over the mitral area and radiating to the axilla.
Aetiology
Mitral regurgitation can be either acute or chronic.
Causes of mitral regurgitation include:
- Infective endocarditis
- Acute myocardial infarction with rupture of papillary muscles
- Rheumatic heart disease
- Congenital defects of the mitral valve
- Cardiomyopathy
Clinical features
Typical features of mitral regurgitation murmur include:
- A pansystolic murmur heard loudest over the mitral area
- Radiation of the murmur to the axilla
- Loudest on expiration in the left lateral decubitus position
Other clinical features may include:
- Displaced, hyperdynamic apex beat
Aortic regurgitation
Aortic regurgitation (AR) occurs when there is a backflow of blood from the aorta into the left ventricle during ventricular diastole.
Aortic regurgitation is associated with an early diastolic murmur heard loudest at the left sternal edge
Aetiology
Aortic regurgitation can be either acute or chronic. Chronic AR is often asymptomatic.
AR can occur due to a disease process affecting the valve itself, or due to dilatation of the aortic root.
Diseases affecting the valve include:
- Congenital bicuspid aortic valve
- Rheumatic heart disease
- Infective endocarditis
Causes of aortic root dilatation include:
- Aortic dissection: can result in acute aortic regurgitation
- Connective tissue diseases (e.g. Marfan’s syndrome)
- Aortitis
Clinical features
Typical features of an aortic regurgitation murmur include:
- Decrescendo early diastolic murmur
- Heard loudest at the left sternal edge (the direction that the turbulent blood flows) sometimes heard loudest over the aortic area
- Austin Flint murmur: a low pitched rumbling mid-diastolic murmur heard best at the apex. This is caused by the regurgitated blood through the aortic valve mixing with blood from the left atrium, during atrial contraction. An Austin Flint murmur is a sign of severe aortic regurgitation.
Other clinical features of aortic regurgitation may include:
- Collapsing pulse (a ‘water hammer pulse’ with wide pulse pressure)
- Displaced, hyperdynamic apex beat
Eponymous clinical signs of aortic regurgitation
There are many eponymous clinical signs associated with aortic regurgitation. These include:
- Corrigan’s sign: visible distention and collapse of carotid arteries in the neck
- De Musset’s sign: head bobbing with each heartbeat
- Quincke’s sign: pulsations are seen in the nail bed with each heartbeat when the nail bed is lightly compressed
- Traube’s sign: ‘pistol shot’ sound heard when stethoscope placed over the femoral artery during systole and diastole
- Muller’s sign: uvula pulsations are seen with each heartbeat
Mitral stenosis
Mitral stenosis (MS) involves narrowing of the mitral valve, which results in decreased filling of the left ventricle during systole and increased left atrial pressure (due to incomplete left atrial emptying).
Mitral stenosis is associated with a low-pitched, rumbling, mid-diastolic murmur heard loudest over the apex.
Aetiology
Rheumatic heart disease is the most common cause of mitral stenosis.
Other rarer causes include:
- Congenital
- Left atrial myxoma
- Connective tissue disorders
- Mucopolysaccharidosis
Clinical features
Typical features of a mitral stenosis murmur include:
- Low-pitched, rumbling mid-diastolic murmur with an opening click (click heard in mid-diastole when the mitral valve opens)
- Murmur is heard loudest over the apex
- Loudest in left lateral decubitus position on expiration
Other clinical features of mitral stenosis may include:
- A low-volume pulse which may be irregularly, irregular (atrial fibrillation is common in mitral stenosis)
- Loud first heart sound with tapping apex beat (due to a palpable closing of the mitral valve)
- A malar flush (plum-red discolouration of the cheeks)
Mitral valve prolapse
A mitral valve prolapse occurs when the mitral valve leaflets prolapse into the left atrium during systole.
Mitral valve prolapse is associated with a combination of a mid-systolic click and mid to late-systolic murmur.
Aetiology
Mitral valve prolapse is the most common valvular abnormality with a prevalence of approximately 5%.
The exact underlying cause of mitral valve prolapse is unknown. Primary (classic) mitral valve prolapse is caused by myxomatous degeneration of the mitral valve and is associated with connective tissue diseases. Secondary (non-classic) mitral valve prolapse occurs when a ‘normal’ valve prolapses.
Clinical features
Typical features of a mitral valve prolapse murmur include:
- Mid-systolic click (prolapse of the mitral valve into the left atrium)
- Followed by a mid or late-systolic murmur
- Heard loudest at the apex
- Loudest in expiration
Tricuspid regurgitation
Tricuspid regurgitation occurs when there is the backflow of blood from the right ventricle into the right atrium during ventricular systole. This causes an increase in right atrial pressure and elevated venous pressures.
Tricuspid regurgitation is associated with a pansystolic murmur heard loudest over the tricuspid region.
Aetiology
Causes of tricuspid regurgitation include:
- Right ventricular dilatation (e.g. secondary to pulmonary stenosis or pulmonary hypertension)
- Rheumatic fever
- Infective endocarditis (intravenous drug users are at high risk of endocarditis affecting the tricuspid valve)
- Carcinoid syndrome
- Congenital (e.g. atrial septal defect, Ebstein anomaly)
Ebstein anomaly
The Ebstein anomaly (i.e. congenital isolated tricuspid regurgitation) is an abnormal attachment of tricuspid valve leaflets which causes the tricuspid valve to displace downwards into the right ventricle.
Clinical features
Typical features of a tricuspid regurgitation murmur include:
- Pansystolic murmur
- Heard loudest over the tricuspid region
- Loudest during inspiration
Other clinical features of tricuspid regurgitation may include:
- Large ‘v-waves’ visible in the jugular veins: caused by the right atrial filling of blood against a closed tricuspid valve
- Visible/palpable hepatic pulsations
- Signs of right-sided heart failure: right ventricular heave, peripheral oedema, hepatomegaly, ascites
Pulmonary stenosis
Pulmonary stenosis (PS) refers to the narrowing of the pulmonary valve. It is commonly associated with other congenital heart defects.
Aetiology
Causes of pulmonary stenosis include:
- Congenital: Turner’s, Noonan’s and Williams syndromes. Tetralogy of Fallot (pulmonary stenosis, right ventricular hypertrophy, ventricular septal defect and an overriding aorta).
- Rheumatic fever
- Carcinoid syndrome
Clinical features
Typical features of a pulmonary stenosis murmur include:
- Ejection systolic murmur heard loudest over pulmonary area
- Loudest during inspiration
- Radiates to left shoulder/left infraclavicular region
- In severe pulmonary stenosis, the murmur is longer and may obscure the sound of A2
Other clinical features of pulmonary stenosis may include:
- Prominent ‘a waves’ in the jugular veins
- Widely split S2: blood from the ventricles takes longer to pass through a narrow pulmonary valve, so pulmonary valve closure occurs much later than aortic valve closure
- P2 may be soft and inaudible
- Right ventricular dilatation can lead to a right ventricular heave, tricuspid regurgitation and peripheral signs of right-sided heart failure (e.g. peripheral oedema, ascites etc)
Pulmonary regurgitation
Pulmonary regurgitation (PR) occurs when there is backflow of blood from the pulmonary artery into the right ventricle during ventricular diastole. Pulmonary regurgitation is rare.
Aetiology
Causes of pulmonary regurgitation include:
- Pulmonary hypertension
- Infective endocarditis
- Congenital valvular heart disease
Clinical features
Pulmonary regurgitation is usually asymptomatic.
Typical features of a pulmonary regurgitation murmur include:
- Early decrescendo murmur heard loudest over the left sternal edge
- Loudest during inspiration
- Usually due to pulmonary hypertension: known as a Graham Steell murmur when associated with mitral stenosis
Tricuspid stenosis
Tricuspid stenosis (TS) refers to narrowing of the tricuspid valve.
Tricuspid stenosis is associated with a soft diastolic murmur heard loudest at 3rd – 4th intercostal space at the left sternal edge
Aetiology
Causes of tricuspid stenosis include:
- Rheumatic fever (most common)
- Congenital disease
- Infective endocarditis
Clinical features
Typical features of a tricuspid stenosis murmur include:
- Mid-diastolic murmur (rarely audible)
- Loudest at 3rd – 4th intercostal space at the left sternal edge
- Loudest during inspiration
Other clinical features of tricuspid stenosis may include:
- Raised JVP with giant ‘a waves’
- Peripheral oedema, ascites
Summary
Table 2. Overview of different heart murmurs.
| Lesion | Cardiac cycle | Character | Breathing | Location | Radiation |
| Aortic stenosis | Systolic | Ejection systolic | Expiration | 2nd intercostal space right sternal edge | Carotid arteries |
| Pulmonary stenosis | Systolic | Ejection systolic | Inspiration | 2nd intercostal space left sternal edge | Left shoulder/infra-clavicular |
| Mitral regurgitation | Systolic | Pansystolic | Expiration | Apex | Axilla |
| Tricuspid regurgitation | Systolic | Pansystolic | Inspiration | Left sternal edge | |
| Mitral valve prolapse | Mid systolic + opening click | Expiration | Apex | ||
| Aortic regurgitation | Early diastolic | Decrescendo | Expiration | Left sternal edge (or 2nd intercostal space right sternal edge) | Left sternal edge |
| Pulmonary regurgitation | Early diastolic | Decrescendo | Inspiration | 2nd intercostal space left sternal edge | |
| Mitral stenosis | Mid/late diastolic | Expiration | Apex | ||
| Tricuspid stenosis | Mid/late diastolic | Inspiration | Left sternal edge |
Editor
Dr Chris Jefferies
References
- OpenStax College. Diagram describing the phases of the human cardiac cycle. License: [CC-BY]. Available from: [LINK]
- adh30/DanielChangMD/DestinyQx. Wiggers diagram. License: [CC-BY-SA]. Available from: [LINK]
- Innes, A, Dover, A, Fairhurst, K. Macleod’s Clinical Examination – 14th Edition. Published in 2013.
- Madhero88. Phonocardiograms from normal and abnormal heart sounds. License: [CC-BY-SA]. Available from: [LINK]