- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
This guide provides a structured approach to interpreting ascitic fluid results in an OSCE setting.
What is ascites?
Ascites is the accumulation of ascitic fluid in the peritoneal cavity.
Many diseases can cause ascites, but the most common cause is portal hypertension, which is usually due to liver cirrhosis.
Ascites does not typically become clinically detectable until there are at least 500mLs of fluid present.
If large amounts of fluid accumulate, the abdomen can become very distended and tense, causing the patient to feel short of breath (due to diaphragmatic splinting).
Analysis of ascitic fluid can help determine the underlying cause and identify signs of infection.
A sample of fluid is typically obtained using a needle and syringe (known as an “ascitic tap” or “paracentesis”) and sent for analysis.
Clinical features of ascites
Typical clinical features of ascites include:
- Abdominal distension
- Abdominal discomfort
- Weight gain
- Shortness of breath
- Reduced appetite
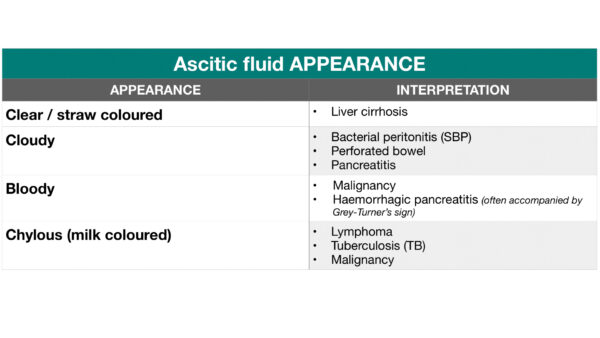
The appearance of ascitic fluid
The appearance of ascitic fluid can be useful in narrowing the differential diagnosis. The table below summarises how the typical appearance of ascitic fluid varies depending on the underlying aetiology.
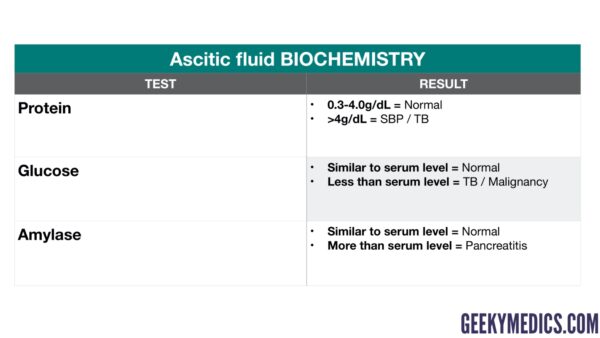
Ascitic fluid biochemistry
Biochemical analysis of ascitic fluid can provide useful insights which can help narrow the differential diagnosis. The table below summarises the typical patterns of biochemical findings which are associated with specific underlying disease processes.
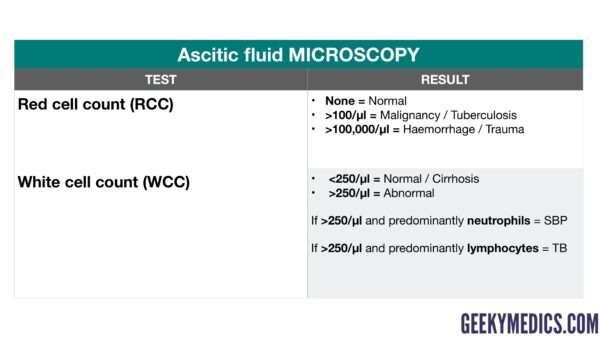
Ascitic fluid microscopy
Ascitic fluid microscopy provides valuable information about the number and type of red and white cells within the fluid which can help narrow the differential diagnosis.
Serum ascitic albumin gradient (SAAG)
The serum ascitic albumin gradient (SAAG) indirectly measures portal pressure and can be used to determine if ascites is due to portal hypertension.
SAAG calculation
SAAG = (serum albumin) – (ascitic fluid albumin)
Interpretation
A high SAAG (>1.1g/dL) suggests the ascitic fluid is a transudate.
A low SAAG (<1.1g/dL) suggests the ascitic fluid is an exudate.
Causes of a high SAAG
A high SAAG (i.e. transudate) suggests the presence of portal hypertension, which may be caused by:
- Cirrhosis
- Hepatic failure
- Venous occlusion (e.g. Budd Chiari syndrome)
- Fulminant hepatic failure
- Alcoholic hepatitis
- Kwashiorkor malnutrition
Causes of a low SAAG
Causes of a low SAAG (i.e. exudate) include:
- Malignancy
- Infection
- Pancreatitis
- Nephrotic syndrome
Lactate dehydrogenase
Another way of differentiating between an exudate and a transudate is to assess the ascitic fluid’s lactate dehydrogenase (LDH) level:
- LDH <225 U/L = transudate
- LDH > 225U/ L = exudate
This method has largely been replaced by the use of SAAG.
Editor
Andrew Gowland




