- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
A bimanual vaginal examination may need to be performed in a number of different clinical scenarios, including unexplained pelvic pain, irregular vaginal bleeding, abnormal vaginal discharge and as part of the assessment of a pelvic mass. Bimanual vaginal examination frequently appears in OSCEs, and you’ll be required to demonstrate excellent communication and practical skills.
This guide demonstrates how to perform a bimanual vaginal examination in an OSCE setting, with an included video demonstration.
Gather equipment
Gather the appropriate equipment:
- Gloves
- Lubricant
- Paper towels
Introduction
Wash your hands and don PPE if appropriate.
Introduce yourself to the patient including your name and role.
Confirm the patient’s name and date of birth.
Explain what the examination will involve using patient-friendly language: “Today, I need to carry out a vaginal examination. This will involve me using one hand to feel your tummy and the other hand to place two fingers into your vagina. This will allow me to assess the vagina, womb and ovaries. It shouldn’t be painful, but it will feel a little uncomfortable. You can ask me to stop at any point.”
Explain the need for a chaperone: “One of the female ward staff members will be present throughout the examination, acting as a chaperone, would that be ok?”
Gain consent to proceed with the examination: “Do you understand everything I’ve said? Do you have any questions? Are you happy for me to carry out the examination?”
Ask the patient if they have any pain or if they think they may be pregnant before proceeding with the clinical examination.
Provide the patient with the opportunity to pass urine before the examination.
Explain to the patient that they’ll need to remove their underwear and lie on the clinical examination couch, covering themselves with the sheet provided.
Provide the patient with privacy to undress and check whether it is okay to re-enter the room before doing so.
Abdominal examination
A brief abdominal examination should always be performed before moving on to a bimanual vaginal examination. This may be less thorough than a full abdominal examination but should at least include inspection and palpation of the abdomen to identify any pain or masses.
Reposition the patient
1. Re-check consent and that the patient is happy to proceed with the examination: “I’m going to move on and examine your genitals. Are you happy for me to do this?”
2. Position the patient in the modified lithotomy position: “Draw your ankles up towards your buttocks, keep your feet flat on the bed, and then let your legs fall open”.
Vulval examination
A vulval examination should be performed before moving on to the bimanual examination. This is to look for any vulval pathology or lymphadenopathy.
1. Don a pair of non-sterile gloves and an apron
2. Expose the patient’s external genitalia and ensure there is adequate lighting
Palpate the inguinal lymph nodes
1. Palpate the inguinal lymph nodes to identify lymphadenopathy, which may be associated with:
- Acute infections (e.g. chlamydia, herpes)
- Malignancy (e.g. vulval cancer)
Inspect the vulva
1. Inspect the vulva for abnormalities:
- Ulcers: typically associated with genital herpes
- Abnormal vaginal discharge: causes include candidiasis, bacterial vaginosis, chlamydia and gonorrhoea
- Scarring: may relate to previous surgery (e.g. episiotomy) or lichen sclerosus (scarring with associated abnormal architecture)
- Vulvovaginal atrophy: most commonly occurs in postmenopausal women
- White lesions (leukoplakia): may be patchy or in a figure-of-eight distribution around the vulva and anus, associated with lichen sclerosus
- Other lesions: causes include folliculitis, molluscum, genital warts and vulval malignancy
- Masses: causes include Bartholin’s cyst and vulval malignancy
- Varicosities: varicose veins secondary to chronic venous disease or obstruction in the pelvis (e.g. pelvic malignancy)
- Female genital mutilation: total or partial removal of the clitoris and/or labia and/or narrowing of the vaginal introitus
2. Inspect for evidence of vaginal prolapse (a bulge visible protruding from the vagina). Asking the patient to cough as you inspect can exacerbate the lump and help confirm the presence of prolapse.
Female genital mutilation
The WHO defines female genital mutilation (FGM) as “all procedures that involve partial or total removal of the external female genitalia, or other injury to the female genital organs for non-medical reasons”.5
Over 200 million girls and women worldwide have undergone FGM.5 Women attending maternity, family planning, gynaecology, and urology clinics (among others) should be asked routinely about the practice of FGM.6 In the UK, healthcare professionals must report cases of FGM in girls under the age of 18 to the police.7
Bartholin’s cyst
Bartholin’s glands are responsible for producing secretions which maintain vaginal moisture and are typically located at 4 and 8 o’clock in relation to the vaginal introitus. These glands can become blocked and/or infected, resulting in cyst formation. Typical findings on clinical examination include a unilateral, fluctuant mass, which may or may not be tender.
Lichen sclerosus
Lichen sclerosus is a chronic inflammatory dermatological condition that can affect the anogenital region in women. It presents with pruritis and clinical examination typically reveals white thickened patches. Destructive scarring and adhesions develop causing distortion of the normal vaginal architecture (shrinking of the labia, narrowing of the introitus, obscuration of the clitoris).
Abnormal vaginal discharge
There are several causes of abnormal vaginal discharge including:
- Bacterial vaginosis: typical findings include a thin, profuse fishy-smelling discharge without pruritis or inflammation
- Candidiasis: typical findings include a curd-like, non-offensive discharge with associated pruritis and inflammation
- Chlamydia and gonorrhoea (symptomatic): typical findings include purulent vaginal discharge
- Trichomoniasis: typical findings include offensive yellow, frothy vaginal discharge with associated pruritis and inflammation
Vaginal examination
Warn the patient you are going to examine the vagina by inserting two fingers and ask if they’re still ok for you to do so.
If the patient consents to continue the examination:
1. Lubricate the gloved index and middle fingers of your dominant hand
2. Carefully separate the labia using the thumb and index finger of your non-dominant hand
3. With your palm facing laterally, gently insert the gloved index and middle finger of your dominant hand into the vagina
Vaginal walls
Palpate the walls of the vagina for any irregularities or masses.
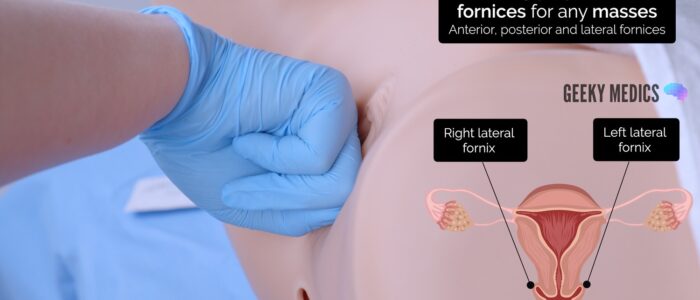
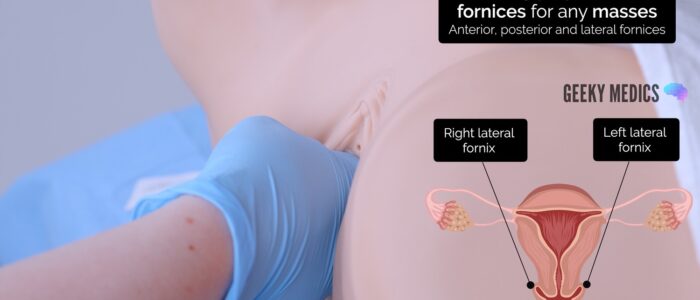
Vaginal fornices
The fornices are the superior portions of the vagina, extending into the recesses created by the vaginal portion of the cervix.
Gently palpate the fornices for any masses.
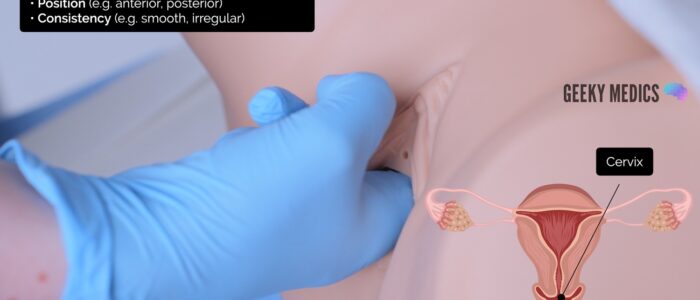
Cervix
Examine the surface of the cervix to assess:
- Position (e.g. anterior or posterior)
- Consistency (e.g. irregular, smooth)
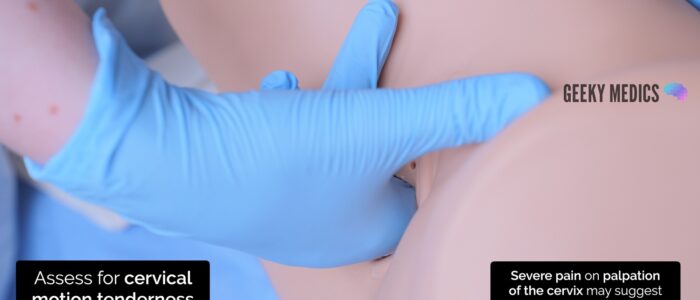
Examine for cervical motion tenderness:
1. Place your non-dominant hand on the abdomen in the suprapubic region
2. Using your two fingers inside the vagina, gently move the cervix in all four directions while observing the patient for any pain
Pain on palpation of the cervix may suggest pelvic inflammatory disease.
Uterus
Bimanually palpate the uterus:
1. Place your non-dominant hand on the abdomen in the suprapubic region
2. Push upwards with the internal fingers while palpating the lower abdomen with your non-dominant hand. You should be able to feel the uterus between your hands.
You should then assess the various characteristics of the uterus:
- Position: the uterus may be anteverted or retroverted
- Size: the uterus should be approximately orange-sized
- Shape: may be distorted by masses such as large fibroids
- Surface characteristics: note if the uterus feels smooth or nodular
- Tenderness: may suggest inflammation (e.g. pelvic inflammatory disease)
Uterine position
The position of the uterus can be described as:
- Anteverted: the uterus is orientated anteriorly towards the bladder. This is the most common position of the uterus.
- Retroverted: the uterus is orientated posteriorly towards the spine. This is a less common uterine position.
Ovaries and uterine tubes
The term adnexa refers to the area that includes the ovaries and fallopian tubes.
Bimanually palpate the adnexa:
1. Position your internal fingers in the left lateral fornix of the vagina
2. Position your external hand onto the left iliac fossa
3. Perform deep palpation of the left iliac fossa whilst moving your internal fingers upwards and laterally (towards the left)
4. Feel for any palpable masses, noting their size and shape (e.g. ovarian cyst, ovarian tumour, fibroid) or tenderness
5. Repeat the adnexal assessment on the right
Finish examination
1. Withdraw your fingers and inspect the glove for blood or abnormal discharge
2. Cover the patient with the sheet, explain that the examination is complete and provide the patient with privacy so they can get dressed. Provide paper towels for the patient to clean themselves.
3. Dispose of the used equipment into a clinical waste bin.
To complete the examination…
Thank the patient for their time.
Dispose of PPE appropriately and wash your hands.
Summarise your findings.
Document the examination in the medical notes, including the details of the chaperone.
Example summary
“Today, I examined Mrs Smith, a 28-year-old female. On general inspection, the patient appeared comfortable at rest. There were no objects or medical equipment around the bed of relevance.“
“Abdominal examination was unremarkable and there were no abnormalities noted on inspection of the vulva. Bimanual examination revealed an anteverted uterus of normal size and shape. There were no masses palpated in the vaginal canal or adnexa.”
“In summary, these findings are consistent with a normal vaginal examination.”
“For completeness, I would like to perform the following further assessments and investigations.”
Further assessments and investigations
- Urinalysis: including β-HCG to rule out pregnancy
- Speculum examination: to visualise the vaginal canal and cervix
- Vaginal swabs/endocervical swabs: if there are concerns about infection (bacterial and viral)
- Ultrasound abdomen and pelvis: to visualise any masses palpated and to assess endometrial thickness
Reviewers
Dr Ashley Jefferies
Community Sexual and Reproductive Health Registrar
Mr Isaac Magani
Consultant Obstetrician and Gynaecologist
References
- Medimage. Adapted by Geeky Medics. Bartholin’s cyst. Licence: CC BY-SA.
- Mikael Häggström. Adapted by Geeky Medics. Lichen sclerosus. Licence: CC0.
- Mikael Häggström. Adapted by Geeky Medics. Vaginal candidiasis. Licence: CC0.
- Mikael Häggström. Adapted by Geeky Medics. Uterine prolapse. Licence: CC0.
- WHO. Female Genital Mutilation. Key facts. Available from: [LINK].
- Erskine K; Collecting data on female genital mutilation. BMJ. 2014 May 13348:g3222. doi: 10.1136/bmj.g3222. Available from: [LINK].
- Department of Health and Social Care. FGM: mandatory reporting in healthcare. 2017. Available from: [LINK].