- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
The term brain tumour refers to an intracranial tumour affecting the brain, meninges, pituitary gland, pineal gland, cranial nerves and/or skull.
In 2015, brain tumours accounted for three percent of total cancers, however, their incidence has been rising.
In adults, the highest incidence occurs in those aged between 85 – 89 years old.
In children less than 15 years old, brain tumours are the second most common cancer (acute lymphoblastic leukaemia is the most common).
Secondary brain tumours are three times more common than primary brain tumours.
Clinical features of brain tumours
A brain tumour’s presentation is typically progressive and subacute in nature.
Signs and symptoms typically relate to the area of the central nervous system affected by the tumour.
Signs related to raised intracranial pressure (ICP) are common, these include:
- Headache (worse on waking, lying down, bending forward or coughing)
- Nausea and vomiting
- Papilloedema
- Coma: a late-stage feature of brain tumours, secondary to raised intracranial pressure
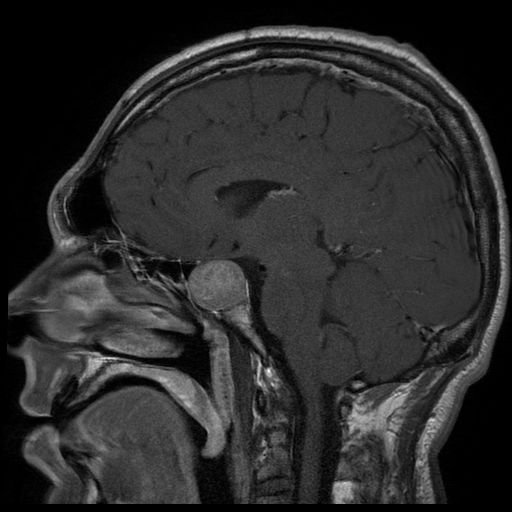
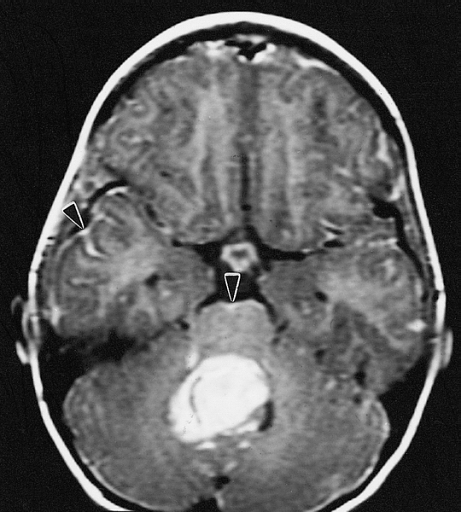
Meningioma
A meningioma is a slow-growing tumour that forms from the arachnoid cell cap found on the meninges.
The peak incidence occurs at 45 years of age, and there is a 2:1 female to male ratio.
Meningiomas are usually benign and surgically viable. They rarely metastasise into the body.
Clinical features
The clinical presentation is dependent on tumour size and location (can lead to mass effect symptoms).
Many patients are asymptomatic with the meningioma detected on brain imaging performed for another indication.
Clinical features may include:
- Headache
- Seizures
- Spastic weakness or numbness in both legs
- Gait abnormalities
- Visual loss if the optic nerve is compressed
Investigations
Relevant investigations include:
- MRI with gadolinium contrast +/- CT
- Angiography

Management
Management is usually conservative unless symptoms develop. Follow-up imaging is used to monitor the meningioma.
If intervention is required, options include surgical excision and/or radiotherapy. Chemotherapy has little benefit.
Prognosis
Meningiomas have a good prognosis with a 91% five-year survival rate.
Pituitary adenoma
Pituitary adenomas occur in the pituitary gland and are responsible for 15% of primary brain tumours.
They can be functional and secrete hormones. Larger tumours (>1cm) are usually non-functional and cause symptoms by mass effect. Most are benign.
Pituitary macroadenomas are the most common cause of hypopituitarism.
Clinical features
Functional pituitary adenomas can cause a variety of clinical presentations including:
- Cushingoid symptoms
- Acromegaly
- Diabetes insipidus
- Hyperpituitarism
- Amenorrhea/galactorrhoea/impotence
Clinical features related to the mass effect of the tumour may include:
- Bitemporal hemianopia: due to compression of the optic chiasm
- Hydrocephalus
- Diplopia
Investigations
Relevant investigations include:
- Endocrine laboratory tests
- MRI with gadolinium contrast +/- CT
Management
Management of pituitary tumours may include:
- Dopamine agonists to treat prolactinomas
- Surgery
- Radiation therapy
Complications
Pituitary apoplexy is a serious complication occurring when a haemorrhage causes a rapid increase in the size of the lesion and surrounding vasogenic oedema.
Due to the mass effect, surrounding tissue necrosis occurs. This can result in sudden onset visual loss, headache and hydrocephalus.
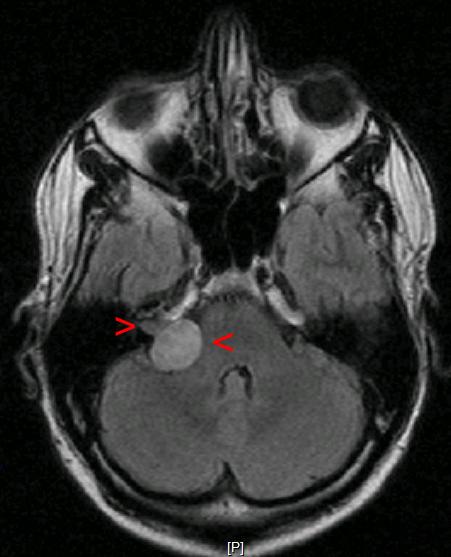
Acoustic neuroma
An acoustic neuroma is a benign tumour of vestibulocochlear Schwann cells (a.k.a. vestibular schwannoma).
Acoustic neuromas account for approximately 5% of intracranial tumours and usually present in people over 30 years old.
Bilateral acoustic neuromas are seen in younger patients and in those with neurofibromatosis type 2.
Clinical features
Typical symptoms of acoustic neuroma include:
- Unilateral sensorineural hearing loss (SNHL) and/or tinnitus: 90% of patients present with progressive SNHL, whereas only 5% present with sudden SNHL
- Dizziness and disequilibrium (vestibular dysfunction)
Other symptoms can include:
- Facial pain and numbness: trigeminal (CN V) nerve compression
- Facial weakness: facial (CN VII) nerve compression
- Headaches, nausea and vomiting: suggestive of raised intracranial pressure
Other important areas to cover in the history include:
- Past medical history or family history of similar tumours (if considering NF2)
Investigations
Relevant investigations include:
- Audiometry: to confirm sensorineural hearing loss
- MRI with gadolinium contrast +/- CT
Management
Management of small tumours may be conservative with annual follow up imaging.
If intervention is required, tumours can be removed surgically or with stereotactic radiosurgery.
Complications
Complications include:
- Post-operative facial palsy
- CSF fluid leakage after surgery: reduced since the introduction of microsurgical techniques
For more information, see the Geeky Medics guide to acoustic neuroma.
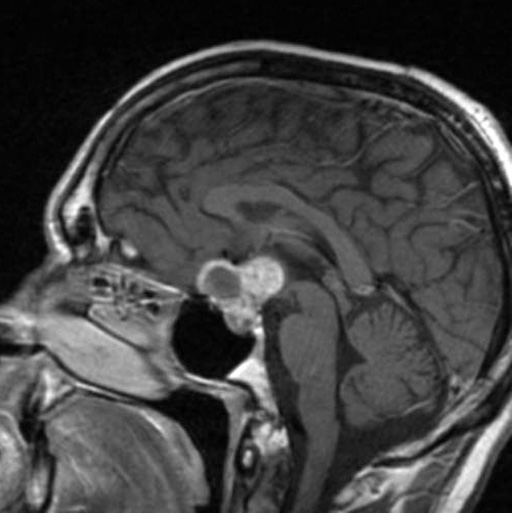
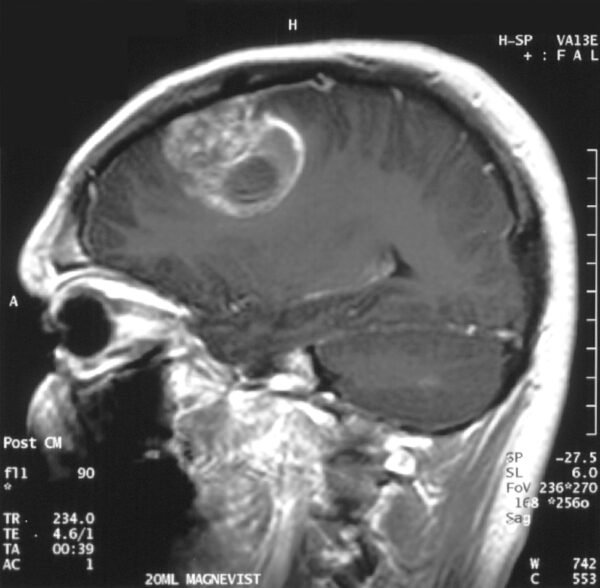
Craniopharyngioma
Craniopharyngiomas arise in the pituitary stalk and can affect the hypothalamus and pituitary. They are derived from residual cells of Rathke’s pouch.
They are responsible for 6-13% of all childhood brain tumours and 1-3% of all adult brain tumours. There is a bimodal onset at age 5-14 and 50-70.
Clinical features
Clinical features may include:
- Growth failure in children
- Diabetes insipidus
- Sexual dysfunction in adults
- Hydrocephalus
- Bitemporal hemianopia
- Pituitary insufficiency
- Headache
Investigations
Relevant investigations include:
- MRI with gadolinium contrast +/- CT
- Endocrine laboratory investigations
Management
Management options for craniopharyngioma include:
- Surgical removal: the treatment of choice
- Radiotherapy can be considered
- Chemotherapy is usually of no benefit
Primary CNS lymphoma
Primary CNS lymphoma is usually diffuse large B cell lymphoma. It accounts for <1% of all non-Hodgkin’s lymphoma subtypes.
Clinical features
Clinical features include:
- Seizures
- Headache
- Altered mental status
- Systemic symptoms: fever, night sweats, unintentional weight loss
- Diplopia
- Vertigo
- Dysphagia
Investigations
Relevant investigations include:
- MRI +/- CT
- HIV testing: CD4 count, viral load
- Lumbar puncture: may show increased WCC and/or cytology positive for lymphoma
- Epstein-Barr virus PCR: may identify Epstein-Barr virus if it is present
Management
Management options for primary CNS lymphoma include:
- Chemotherapy: usually methotrexate, cytarabine may be used in addition
- Radiation therapy: whole-brain radiation therapy alongside chemotherapy
- Steroids: dexamethasone
- Surgery: tumours are typically not resectable. However, if mass effect is present, resection may be considered as a life-sparing procedure.
Prognosis
The prognosis is usually poor. In patients co-diagnosed with AIDS, median survival is four months with radiotherapy. With methotrexate-based chemotherapy, median survival is 10-18 months.
Medulloblastoma
Medulloblastoma is the most common malignant tumour in children. It is thought to arise from cerebellar stem cells between the brainstem and cerebellum near the fourth ventricle.
Medulloblastoma tends to seed within CSF pathways giving rise to its high metastatic propensity. Metastatic disease is classified by the Chang system.
Clinical features
Clinical features include:
- Hydrocephalus: worsening headaches and decreased level of consciousness
- Cerebellar signs: incoordination of limbs, gait abnormalities
- Mass effect symptoms: speech and vision abnormalities, unilateral weakness, headache, drowsiness and nausea/vomiting
- Extraocular muscle palsies: typically presents as diplopia
Investigations
Relevant investigations include:
- Lumbar puncture (LP): performed post-operatively and useful for staging
- MRI +/- CT including spinal imaging
Management
Management options for medulloblastoma include:
- Surgical removal of the tumour
- Radiotherapy
- Chemotherapy
Prognosis
The five-year survival for standard-risk patients is approximately 70%.
Glioma
Glioma is an umbrella term for a variety of different tumour subtypes. These include astrocytomas, glioblastoma multiforme (GBM), pilocytic astrocytoma (PCA), ependymomas and oligodendrogliomas.
Gliomas account for 50% of primary brain tumours in adults and they are more common in men and in industrial countries. The exception is PCA, which is the commonest benign tumour in children.
The mean age of onset is 55 and they account for 20% of all intracranial tumours. All gliomas metastasise via the cerebrospinal fluid.
Clinical features
Clinical features include:
- Headache
- Vomiting
- Seizures
- Focal neurological deficit including visual loss
- Cranial nerve dysfunction
Investigations
Relevant investigations include:
- MRI with gadolinium contrast
Management
Surgery
For all gliomas, complete excision of the tumour is often challenging. This is because the margins between the tumour and the brain are rarely clear. Biopsies taken can be used to help make a histological diagnosis.
Carmustine implants can also be inserted; these are alkylating agents, which can help reduce the rate of tumour spread (however, they do carry a risk of serious cerebral oedema).
Radiotherapy
Targeted radiotherapy can be used to shrink tumours or to destroy any residual tumour cells after excision.
Chemotherapy
Temozolomide has been shown to increase survival when given alongside surgery and/or radiotherapy.
Prognosis
Overall, the prognosis is poor as gliomas are rarely curable. As an example, GBMs have a mean life expectancy of one year.
PCAs are an exception, with more than 95% of patients surviving five years.
Reviewer
Konstantinos Lilimpakis
Neurosurgical Clinical Fellow
Editors
Samantha Strickland
Dr Chris Jefferies
References
- DN Louis, A Perry, G Reifenberger, A von Deimling, D Figarella-Branger, W KCavenee et al (2016) ‘The 2016 World Health Organization Classification of Tumours of the Central Nervous System: a summary’, Acta Neuropathologica, 131(6), pp. 803-820.
- Whittle IR, Smith C, Navoo P, Collie D (2004), Meningiomas, Lancet, 363, pp. 1535-1543.
- BMJ Best Practice (2017) Overview of brain tumours BMJ Best Practice. Available from: [LINK]
- Cancer Research UK (2018) Brain, other CNS and intracranial tumours incidence statistics’, Cancer Research UK. Available from: [LINK]
- National Institute for Health and Care Excellence (2006) ‘Improving outcomes for people with brain and other central nervous system tumours’, NICE guideline (CSG10)
- Grant R (2004) ‘Overview: brain tumour diagnosis and management/Royal College of Physicians guidelines’, J Neurol Neurosurg Psychiatry 75(2), pp. 18-23
- Hamilton W, Kernick D (2007) ‘Clinical features of primary brain tumours: a case-control study using electronic primary care records’, Br J Gen Pract 57(542), pp. 695-699
- Glitzy queen00. Contrast enhanced meningioma. License: [Public domain]
- Hellerhoff. Pituitary adenoma. License: [CC-BY]
- MRT-Bild. Akustikusneurinom Mrt. License: [Public domain]
- Hellerhoff. Craniopharyngoma. License: [CC-BY]
- The Armed Forces Institute of Pathology. Medulloblastoma. License: [Public domain]
- Christaras A. Glioblastoma. License: [CC-BY]