- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Breast cancer is the most common cancer in women.1 It is the second most common cancer worldwide.2
Every year in the UK around 50,000 new cases of breast cancer are diagnosed.3
Patients can present with a range of symptoms, but most often they will present with a painless breast lump. However, many breast cancers are initially detected by routine screening in asymptomatic patients. It can affect both males and females but is much less common in men.
Each year a full-time GP will likely diagnose 1-2 cases of breast cancer. It is an important diagnosis to make as early detection and intervention dramatically improves prognosis.3
Aetiology
Breast cancer occurs due to damaged DNA and genetic mutations. Exposure to oestrogen also has an effect on these mutations and hence it is more common in women.
There are some important genetic mutations to be aware of. BRCA1 and BRCA2 are anti-oncogenes that both code for tumour suppressor proteins which reduce the risk of breast cancer when functioning normally. Mutations in either of these genes, therefore, increases the risk of breast cancer as well as an increased risk of ovarian cancer.4,5 These mutations are often inherited in an autosomal dominant fashion and families may require genetic counselling as a result.5
Human epidermal growth factor receptor 2 (HER2 receptor) is a transmembrane glycoprotein that plays a key role in cell survival, proliferation and differentiation and thus is an important oncogene in breast cancer when it is overexpressed.6
The aetiology of breast cancer is multifactorial with many modifiable and non-modifiable risk factors (see below). But first, some basic breast anatomy to help us understand where these cancers arise from.
Breast anatomy
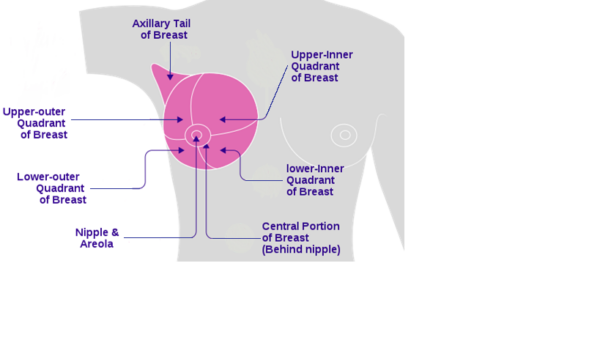
The female breast is found anterior to the pectoralis muscles and is composed of a network of lobules and ducts (see Figure 1). Lobules are the secretory units of the breast that are made up of many epithelial acini cells. These secrete milk into a series of ducts which eventually form the lactiferous ducts that empty onto the surface of the nipple. Adipose tissue and fibrous connective tissue support the lobes and lobules.
The lymphatics of the breast run in the sub-mammary space. There are different pathways that the lymphatics can drain through and there are between 20 to 40 lymph nodes. These can be grouped anatomically and can also be divided into surgical levels.7 For more information on how the axillary lymph nodes are grouped, please refer to the Geeky Medics guide to breast examination. Most importantly, surgeons must be able to locate the lymph nodes so that it can be determined if the cancer has metastasised to the local lymphatic system.

Classifications of breast cancer
Breast cancer is typically divided into two classifications: non-invasive and invasive. There are also rarer forms of breast cancer to be aware of.
Non-invasive breast cancer
These tumour cells have not invaded the basement membrane and can be referred to as premalignant or pre-cancerous. They may progress to an invasive form of breast cancer.9
They can arise from:
- The epithelial cells lining the ducts: this is called ductal carcinoma in situ (DCIS). There are four subtypes of DCIS: papillary, cribriform, solid, and comedo. Knowing the subtype of cancer can help predict the rate of transformation to invasive cancer.10
- The epithelial cells inside the lobules: this is called lobular carcinoma in-situ (LCIS) and is confined to the acini cells. LCIS predominantly occurs in pre-menopausal women and is more often found in both breasts compared to DCIS which is usually unilateral.
Invasive breast cancer
These tumour cells have invaded the basement membrane:
- Invasive ductal carcinoma (also called ‘no special type’): the most common type of breast cancer. It is called ‘no special type’ because when it is examined under the microscope the cancer cells have no particular features.
- Invasive lobular carcinoma
Rare breast cancers
There are two rare types of breast cancer that are important to know about, as they can easily be mistaken for other benign conditions:
- Inflammatory breast cancer: presents with an erythematous oedematous breast and is often mistaken for an infection (mastitis) or breast abscess. Note: patients will not have a fever, chills or elevated white cell count.11,12
- Paget’s disease of the nipple: presents with rough, dry, erythematous and ulcerated skin surrounding the nipple. It can look similar to eczema, however, it must be distinguished from this as Paget’s disease is often associated with an underlying in-situ or invasive cancer.
Other rare types of breast cancer – described as ‘special type’ as they have features under the microscope which allow us to classify them more specifically – include the following: mucinous; medullary; papillary; tubular; phyllodes; metaplastic; basal-like and primary breast lymphoma.
Risk factors
There are many risk factors associated with developing breast cancer, most of which increase the risk of most types of cancer.4,13,14 Increased exposure to oestrogen is one of the more important and specific risk factors for breast cancer.
Increased exposure to oestrogen
Increased exposure to oestrogen may be due to a range of factors including:
- Nulliparity and increasing age of first childbirth
- Early menarche (menstruation starting in girls under 12 years old): causing early exposure to oestrogen
- Late menopause (>55-years-old): increasing the length of exposure to oestrogen
- Hormone replacement therapy (HRT) with oestrogen and progestogen
- Obesity: increases oestrogen levels because more adipose tissue leads to increased expression of an enzyme called aromatase which increases the synthesis of oestrogen
Other risk factors
Other risk factors for breast cancer include:
- Age: risk increases with age
- Female gender
- Family history: first degree relative with breast cancer
- Previous breast cancer
- Genetics: BRCA1 and BRCA2 mutations
- Radiation therapy to the chest
- Not having breastfed
- Lifestyle: excessive alcohol and fat intake
There has been debate over whether the combined hormonal contraceptive pill increases the risk of breast cancer. Recent data suggests a dose-response relationship (i.e. earlier use of oral contraception increases the risk of breast cancer).15 Recent guidelines also suggest that there is a small increased risk of breast cancer when taking the pill, but this reduces over time after stopping it.16
Protective factors
Breastfeeding is a protective factor against breast cancer.
Clinical features
History
Most patients present with a painless lump in the breast or axilla. The patient may have noticed nipple discharge.
Bilateral clear or milky nipple discharge is usually benign and is not associated with breast cancer, although further investigation is required to rule out other causes.
If the nipple discharge is unilateral or bloody this is abnormal and needs investigating for breast cancer.17
If patients present late, they may have more systemic symptoms suggesting the disease has metastasised. These include weight loss, anorexia, bone pain, jaundice, fatigue and breathlessness.
Many women present with breast pain, but it is very rarely a symptom of breast cancer.
Clinical examination
It is always important to perform a thorough examination of both breasts and axillary lymph nodes when the patient presents with a breast lump or features suspicious of breast cancer. See the Geeky Medics guide to breast examination for more details. The main features that may be found on examination are a lump, nipple changes and/or skin changes.
Breast lumps
Breast lump features more commonly associated with breast cancer include:
- Hard with a gritty texture
- Ill-defined, irregular margins
- Tethered (attached to the surrounding breast tissue or skin) or fixed (attached to the chest wall)
- Most breast cancers arise in the upper outer quadrant of the breast 18 (see Figure 2).
- A suspicious lump felt in the axilla may indicate metastasis to the lymph nodes.
Nipple changes
Nipple changes associated with breast cancer include:
- Bleeding, discharge, inversion or deviation of the nipple.
- Paget’s disease, as explained earlier, can mislead clinicians as the rough, dry, erythematous, and ulcerated skin surrounding the nipple can be misdiagnosed as eczema (this requires a punch biopsy to distinguish between Paget’s and eczema).
Skin changes
Skin changes associated with breast cancer include:
- Rough, dry, erythematous, and ulcerated skin surrounding the nipple can be caused by Paget’s disease
- A cancerous breast lump beneath the skin can cause dimpling or puckering of the skin.
- Peau d’orange: the skin looks like the surface of an orange. This occurs when the lymphatic system that drains the skin is blocked by cancer cells causing the skin to become oedematous.20 This can be easily misdiagnosed as an infection.
Differential diagnosis
There is a wide range of potential differential diagnoses associated with a breast lump, which is illustrated in the table below.
Table 1. Differential diagnoses of breast lumps
|
Differential |
Clinical summary |
|
Fibroadenoma |
Benign overgrowth of collagenous mesenchyme of one breast lobule Firm, non-tender, highly mobile palpable lumps |
|
Breast cyst |
Palpable, benign, fluid-filled rounded lumps that are not fixed to surrounding tissue |
|
Intraductal papilloma |
Benign, warty lesion usually located just behind the areola Present as a small lump and a sticky, possibly blood-stained discharge may be noticed |
|
Breast abscess |
Most common in breastfeeding mothers Presents with malaise and fever accompanied by a throbbing pain The breast will be hot and red and may have tender ipsilateral lymphadenopathy in the axilla |
|
Fat necrosis |
Fibrosis and calcification of the breast tissue usually due to trauma and can present as an irregular craggy mass, skin tethering, nipple retraction, thus mimicking a cancer |
Investigations
Most patients will present to their GP with a breast lump, nipple or skin changes and will be referred urgently under the two-week wait (2WW) scheme for suspected cancer.
Once referred, the patient will be seen in a secondary care breast clinic for a triple assessment. This is a ‘one-stop’ clinic where all three parts of the assessment occur on the same day. This is so all the information can be gathered to be discussed at a multidisciplinary team meeting if needed.
The triple assessment consists of:
- Clinical history and examination by a breast surgeon
- Radiological imaging (see below)
- Core biopsy or fine-needle aspiration (see below)
Imaging
Ultrasound
Ultrasound imaging is typically used for younger women, usually under the age of 40 to investigate a breast lump. This is because younger women tend to have denser breast tissue, this makes mammography less sensitive for detecting breast cancers, so ultrasound is used instead.21
Mammogram
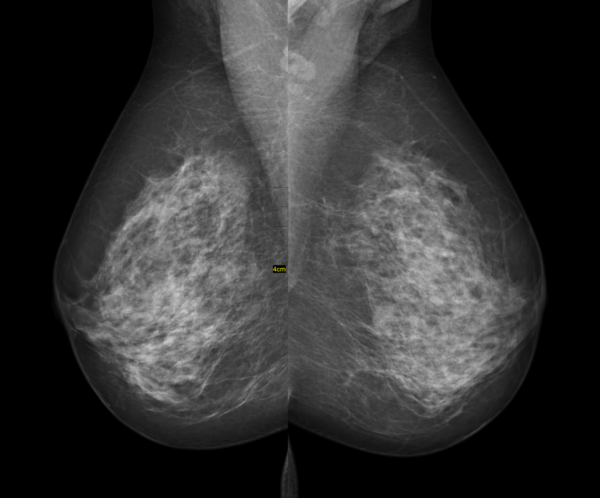
Mammograms are usually taken in two views (mediolateral oblique and craniocaudal) to image as much of the breast tissue as possible. This also allows the radiologist to see structures that would be superimposed in one view from another angle so they are less likely to miss smaller sinister masses.
Denser tissue appears whiter (e.g. fibrous tissue and calcifications) as they attenuate more X-rays, compared to fat which appears grey. See Figure 3 showing a bilateral mammogram in the mediolateral oblique view.
Histology and cytology
Fine needle aspiration
Fine needle aspiration (FNA) uses a single fine needle to collect cells allowing for cytology to examine isolated cells. This technique is often used for smaller more cystic lumps and is usually performed under ultrasound guidance.
Core biopsy
Core biopsy uses a wider needle often performed under ultrasound guidance. It takes a core of tissue, which provides much more information about the cancer and its involvement with surrounding tissues leading to a higher diagnostic yield compared to FNA.
Screening
There is a breast cancer screening program in the UK for women aged 50 to 70 in which a two-view mammogram is performed every 3 years.
Diagnosis
Staging
The TNM (tumour, node, metastasis) staging system is used to work out the stage of a breast cancer when all the information is collected. You can read more about the TNM staging system here.
Receptor status
Laboratory investigations also reveal the hormone receptor status of breast cancer. They look at whether the cancer is positive for progesterone receptors (PR+) and oestrogen receptors (ER+). These receptors have proliferative effects on the cells and are driven by their respective hormones. Thus, by knowing the receptor status of the cancer we can use targeted treatments that act on these receptors (see below in the medical management section of the article). Some patients are diagnosed with triple-negative breast cancer, which means they are negative for oestrogen, progesterone and HER2 receptors. This, unfortunately, limits treatment options and often has a poor prognosis.23
Management
There are both medical and surgical approaches to treating breast cancer, the exact combination of these depends on the stage of the cancer, its size, the age of the patient and the molecular signature of the cancer.
Medical management
Sometimes medical treatment alone is preferred for older patients in whom surgery is not appropriate, but it is often used in conjunction with surgical approaches.
Endocrine therapy
Endocrine medications essentially aim to reduce oestrogen activity to reduce tumour growth:
- Tamoxifen: used in premenopausal women with ER+ cancer, works by blocking oestrogen receptors
- Aromatase inhibitors (Letrozole, Anastrozole, Exemestane): only used in postmenopausal women with ER+ cancer. They work by blocking the enzyme aromatase which converts androgens into oestrogen.
Biologics
For cancers that express HER2, a drug called trastuzumab (also called Herceptin) is used, which is a monoclonal antibody that targets HER2.
Chemotherapy
Chemotherapy can be divided into neoadjuvant and adjuvant. Neoadjuvant chemotherapy is used prior to surgery to help shrink the cancer to allow for breast-conserving surgery. Adjuvant chemotherapy is used after surgery to try and prevent the recurrence of the cancer and increase survival.
Oncotype DX breast recurrence score assay: the patient’s breast cancer cells are sent for genetic testing, where a 21 gene panel is used to analyse the cells and produces a score between 0 and 100. The higher the score the more likely the cancer will recur. So, it is used to decide if adjuvant chemotherapy is warranted, helping to avoid patients from being subject to chemotherapy that they may not benefit from.24
Gonadotropin-releasing hormone agonists like goserelin can be used in premenopausal women to help protect their ovaries from premature ovarian failure which is a potential side effect of the chemotherapy.25
Radiotherapy
Radiotherapy is recommended to most patients with invasive cancer after wide local excision. It is also used to treat bone lesions from metastatic breast cancer.
Surgical management
Wide local excision
Wide local excision removes the breast cancer with a margin of healthy tissue around the cancer. This approach is used if the cancer is small. This surgical option is favoured as it conserves the breast.
Mastectomy
Mastectomy involves removing the entire breast and skin overlying it. This approach is used for larger breast cancers or multifocal cancers where a wide local excision would not be successful.
The approach used also depends on the size of the breasts. A small cancer but small breasts may require a mastectomy to safely remove the cancer, so it is patient dependant.
Sentinel node sampling
Axillary node sampling is performed intraoperatively with the aim of ruling out lymphatic involvement. The lymph nodes are located by injecting radioactive technetium into the nipple on the affected side before theatre. That technetium travels up the lymphatic vessels to the first lymph node also known as the sentinel lymph node. During theatre when the patient is anaesthetised, blue dye is injected around the nipple. This again travels along the lymphatic vessels to the sentinel lymph node. The sentinel lymph node is thus detected in two ways, the radioactive technetium using a Geiger counter, and visually with blue dye. The sentinel node is removed and sent to the lab for analysis. If it shows evidence of metastasis then surgical clearance of the axillary nodes is performed. Some hospitals have the ability to send the sentinel node to the lab during the operation so the patient can have axillary node clearance at the same time, thus avoiding a second operation.
Reconstruction
Breast reconstruction is an important part of the treatment and is discussed with the patient. It can be performed later or at the same time as the cancer removal.
Ovarian ablation
Ovarian ablation via surgery or radiotherapy is used to stop oestrogen synthesis. An oophorectomy is rarely performed because preventing oestrogen synthesis can be achieved through drugs or radiotherapy. It is most often used in women with a BRCA1 or BRCA2 mutation as this also predisposes them to ovarian cancer.
Complications
The most important complication of breast cancer is metastases, which can occur via three mechanisms:
- Direct spread: into skin and muscle, causing skin ulceration
- Lymphatic spread: the axillary nodes are the commonest initial site of metastasis
- Haematogenous spread: blood-borne metastasis often occurs to the lungs, bones, liver and brain
There are also important complications that can arise from the surgery. Notably, if the patient requires axillary node clearance due to lymphatic spread of the cancer there is a risk of damage to the brachial plexus and due to removal of the lymphatics, there is a risk of developing lymphoedema in the arm of the operated side.
Key points
- Breast cancer is the most common cancer in women and its aetiology is multifactorial.
- There are many risk factors, most important are those that increase exposure to oestrogen as well as important genetic mutations such as BRCA1 and BRCA2.
- Patients mostly present with a painless lump, but be aware of those rarer breast cancers that can be disguised as seemingly benign conditions.
- Patients will be referred under a two-week wait to a triple assessment clinic for a thorough workup to investigate their breast lump.
- Surgery is often the mainstay of treatment and is either a wide local excision for smaller breast cancers or a mastectomy for larger or multifocal cancers.
- Medications are used alongside surgical treatment. The type of medication used depends on the age of the patient and the molecular signature of the cancer.
- The most important complication of breast cancer is metastasis.
References
- Benson JR, Jatoi I. The global breast cancer burden. Published in 2012. Available from: [LINK]
- Ferley J, SoerjomataramI I, Ervik M, Dikshit R, Eser S. Cancer Incidence and Mortality Worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Published in 2013. Available from: [LINK]
- NICE CKS. Breast cancer recognition and referral. Published in November 2015. Available from: [LINK]
- Sun YS, Zhao Z, Yang ZN, et al. Risk Factors and Preventions of Breast Cancer. Published in 2017. Available from [LINK]
- Mehrgou A, Akouchekian M. The importance of BRCA1 and BRCA2 genes mutations in breast cancer development. Published in 2016. Available from [LINK]
- Albagoush SA, Limaiem F. HER2. Published in 2020. Available from [LINK]
- Grey’s Anatomy. The Anatomical Basis of Clinical Practice, 40th Section 7: Thorax, page 932 Lymphatic drainage. Published in 2008. ISBN 978-0-443-06684-9
- Don Bliss. Breast and Adjacent Lymph Nodes. License: [Public domain]. Available from: [LINK]
- Seijen MV, Lips EH, Thompson AM et al. Ductal carcinoma in situ: to treat or not to treat, that is the question. Published in 2019. Available from [LINK]
- Alkabban FM, Ferguson T. Cancer, Breast. Published in 2019. Available from: [LINK]
- Mamouch F, Berrada N, Aoullay Z, et al. Inflammatory Breast Cancer: A Literature Review. Published in 2018. Available from: [LINK]
- Ha KY, Glass SB, Laurie L. Inflammatory breast carcinoma. Published in 2013. Available from: [LINK]
- Momenimovahed Z, Salehiniya H. Epidemiological characteristics of and risk factors for breast cancer in the world. Published in 2019. Available from: [LINK]
- Seiler A, Chen MA, Brown RL et al. Obesity, Dietary Factors, Nutrition, and Breast Cancer Risk. Published in 2018. Available from: [LINK]
- Ji LW, Jing CX, Zhuang SL et al. Effect of age at first use of oral contraceptives on breast cancer risk: An updated meta-analysis. Published in 2019. Available from: [LINK]
- FSRH Clinical Effectiveness Unit. Combined Hormonal Contraception. Published in 2020. Available from [LINK]
- Sajadi-Ernazarova KR, Sugumar K, Adigun R. Breast Nipple Discharge. Published in 2020. Available from [LINK]
- Ji F, Xiao WK, Yang CQ, et al. Tumor location of the central and nipple portion is associated with impaired survival for women with breast cancer. Published in 2019. Available from [LINK]
- Adapted from: Cancer Research UK uploader. Breast cancer incidence by anatomical site (females).svg. License: CC BY-SA. Available from [LINK]
- Rinaldi RM, Sapra A, Bellin LS. Breast Lymphatics. Published in 2020. Available from [LINK]
- Malherbe K, Annamaraju P. Breast Ultrasound. Published in 2021. Available from [LINK]
- Dilmen N. 40 F, Bilateral digital mammography images of the breasts; mediolateral oblique view. License: CC BY-SA 3.0. Available from [LINK]
- Mehanna J, Haddad FG, Eid R et al. Triple-negative breast cancer: current perspective on the evolving therapeutic landscape. Published in 2019. Available from [LINK]
- Crolley VE, Marashi H, Rawther S, et al. The impact of Oncotype DX breast cancer assay results on clinical practice: a UK experience. Published in 2020. Available from [LINK]
- Moo TA, Sanford R, Dang C et al. Overview of Breast Cancer Therapy. Published in 2018. Available from [LINK]
Reviewer
Miss Chrissie Laban BSc, MRCS, MD, FRCS
Consultant Oncoplastic Breast Surgeon
Editor
Sherrie Samuels