- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Breast examination frequently appears in OSCEs and you’ll be expected to pick up the relevant clinical signs using your examination skills. This breast examination OSCE guide provides a clear step-by-step approach to examining the breast, with an included video demonstration.
Introduction
Wash your hands and don PPE if appropriate.
Introduce yourself to the patient including your name and role.
Confirm the patient’s name and date of birth.
Briefly explain what the examination will involve using patient-friendly language: “Today I’ve been asked to perform a breast examination. The examination will involve me first inspecting the breasts, then placing a hand on the breasts to assess the breast tissue. Finally, I’ll examine the glands of your neck and armpit.”
Explain the need for a chaperone: “One of the female ward staff members will be present throughout the examination, acting as a chaperone, would that be ok?”
Check if the patient understands everything you’ve said and allow time for questions: “Does everything I’ve said make sense? Do you feel you understand what the examination will involve? Do you have any questions?”
Gain consent to proceed with the examination: “Are you happy for me to carry out the breast examination?”
Position the patient sitting upright on the side of the bed.
Ask the patient to undress down to the waist to adequately expose their breasts for the examination. Provide the patient with privacy to get undressed and offer a blanket to allow exposure only when required.
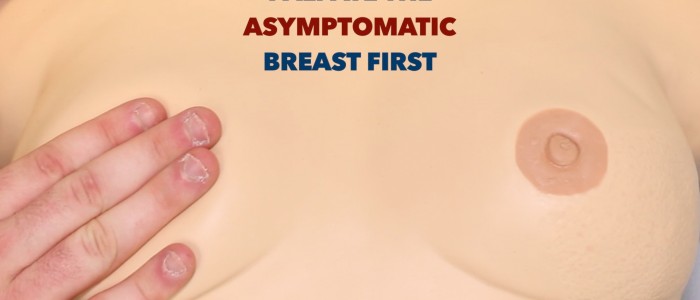
If the patient has presented due to concerns about a lump, ask about its location. This can be helpful during initial inspection and when palpating the breasts as you should always begin palpation on the asymptomatic breast.
Ask the patient if they have any pain before proceeding with the clinical examination.
Inspection
With the patient sitting on the side of the bed ask them to place their hands on their thighs to relax the pectoral muscles.
Inspect the breasts looking for:
- Scars: these may indicate previous breast surgery such as lumpectomy (small scar) or mastectomy (large diagonal scar).
- Asymmetry: this can be helpful in identifying abnormalities via comparison, however, it should be noted that breast asymmetry is a normal feature in most women.
- Masses: note any visible lumps that will require further assessment.
- Nipple abnormalities: these can include nipple inversion and discharge.
- Skin changes: including scaling, erythema, puckering and peau d’orange.
Nipple abnormalities
Nipple inversion is a normal finding in a significant proportion of women (e.g. congenital or weight-loss associated nipple inversion). However, if nipple inversion develops without a clear precipitant, the possibility of underlying pathology should be considered. Possible pathological causes of nipple inversion include breast cancer, breast abscess, mammary duct ectasia and mastitis.
Nipple discharge is benign is most cases (e.g. pregnancy, breast-feeding) however less commonly it can be associated with mastitis or underlying breast cancer (rare).
Skin changes associated with breast pathology
Scaling of the nipple and/or areola associated with erythema and pruritis are typical features of Paget’s disease of the breast (see the example image). Paget’s disease is associated with underlying in-situ or invasive carcinoma of the breast.
Erythema of the breast tissue has a wide range of causes including infection (e.g. mastitis or breast abscess), trauma (e.g. fat necrosis) and underlying breast cancer.
Puckering of breast tissue is typically associated with invasion of the suspensory ligaments of the breast by an underlying malignancy that results in ligamentous contraction which draws the skin inwards.
Peau d’orange (dimpling of the skin resembling an orange peel) occurs due to cutaenous lymphatic oedema. The dimples represent tethering of the swollen skin to hair follicles and sweat glands. Peau d’orange is typically associated with inflammatory breast cancer.
Hands pushing into the hips
Repeat inspection with the patient pressing their hands into their hips to contract the pectoralis muscles.
If a mass is visible, observe if it moves when the pectoralis muscle contracts which suggests tethering to the underlying tissue (e.g. invasive breast malignancy).
The manoeuvre may also accentuate puckering if a mass invading the suspensory ligaments of the breast is also tethered to the pectoralis muscle.
Arms above the head whilst leaning forward
Finally, complete your inspection by asking the patient to place their hands behind their head and lean forward so that the breasts are pendulous.
This position exposes the entire breast and will exaggerate any asymmetry, skin dimpling or puckering.
Breast palpation
Adjust the head of the bed to 45° and ask the patient to lie down. Begin palpation on the asymptomatic breast first and then repeat all examination steps on the contralateral breast. Ask the patient to place the hand on the side being examined behind their head to fully expose the breast.
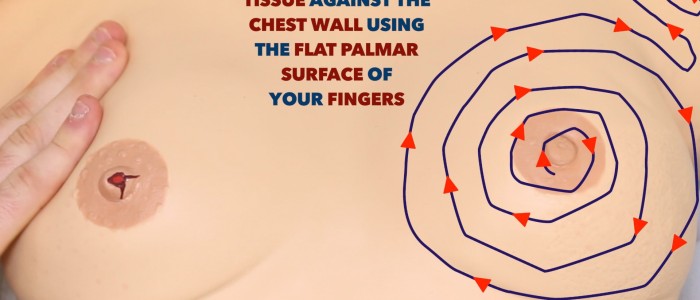
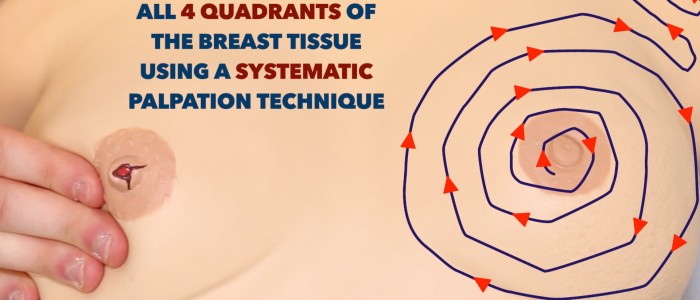
A systematic approach to palpation is essential to ensure all areas of the breast are examined. There are several different techniques all of which are equally appropriate if you perform them correctly:
- Clock face method: view the breast as a clock face and examine each ‘hour’ from the outside towards the nipple.
- Spiral method: begin palpation at the nipple and work outwards in a concentric circular motion.
- Quadrants method: divide the breast into quadrants and examine each thoroughly.
Use the flats of your middle three fingers to compress the breast tissue against the chest wall, as you feel for any masses. If a mass is detected, assess the following characteristics:
- Location
- Size
- Shape
- Consistency
- Mobility
- Fluctuance
- Overlying skin changes
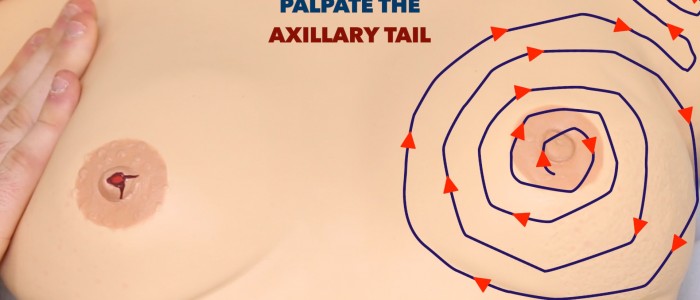
Axillary tail
The axillary tail is a projection of breast tissue that begins in the upper outer quadrant of the breast and extends into the axilla. The majority of breast cancers develop in the upper outer quadrant so it’s essential this area is examined thoroughly.
Characteristics of a breast lump
If you palpate a mass during a breast examination assess the following characteristics.
Location
Which quadrant of the breast is the mass located within?
How far away from the nipple is the mass located?
Size and shape
What are the approximate dimensions of the mass?
What shape is the mass?
Consistency
What is the consistency of the mass on palpation? (e.g. smooth/firm/stony/rubbery)
Overlying skin changes
Are there any changes to the skin overlying the mass? (e.g. erythema/puckering)
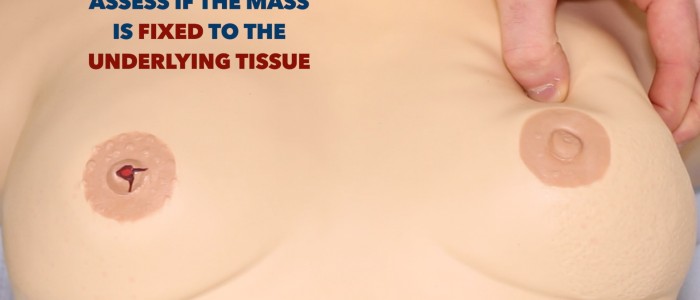
Mobility
Assess the degree of mobility the mass has:
- Does it move freely?
- Does it move with the overlying skin?
- Does it move with pectoral contraction?
Fluctuance
Hold the mass by its sides and then apply pressure to the centre of the mass with another finger. If the mass is fluid-filled (e.g. cyst) then you should feel the sides bulging outwards.
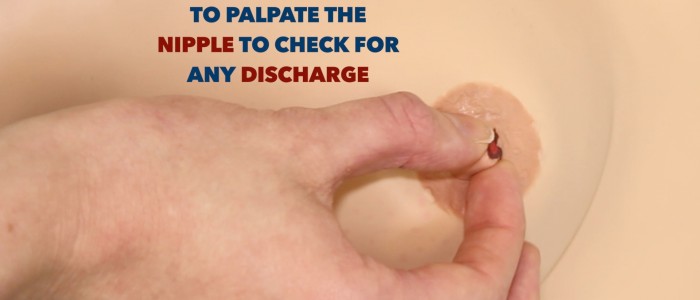
Nipple-areolar complex
Use the flats of your middle three fingers to compress the areolar tissue towards the nipple as you inspect for any nipple discharge.
If there is a history of nipple discharge, but none is visible, ask the patient to attempt to express discharge from the nipple (if they are comfortable to do so) and assess the characteristics of the discharge:
- Colour (e.g. blood-stained, green, yellow)
- Consistency (e.g. thick, watery)
- Volume
Nipple discharge
Milky discharge: normal during pregnancy and when breastfeeding (bilateral). Galactorrhoea (nonpuerperal lactation) is pathological and caused by the presence of a prolactinoma.
Purulent discharge: thick yellow, green or brown discharge with an offensive smell. Possible causes include mastitis and central breast abscess.
Watery and bloody discharge: several possible causes however ductal carcinoma in situ is the most important diagnosis to consider.
Elevate the breast
Lift the breast with your hand to inspect for evidence of pathology not visible during the initial inspection (e.g. dimpling, skin changes).
Lymph nodes
Palpate the regional lymph nodes which are responsible for lymphatic drainage of the breast to identify evidence of breast cancer metastases. Enlarged, hard, irregular lymph nodes are suggestive of metastatic spread.
Axillary lymph nodes
1. Ensure the patient is positioned lying down on the examination couch at 45°.
2. Ask if the patient has any pain in either shoulder before moving the arm.
3. Begin by inspecting each axilla for evidence of scars, masses, or skin changes.
4. When examining the right axilla, hold the patient’s right forearm in your right hand and instruct them to relax it completely, allowing you to support the weight. This allows the axillary muscles to relax.
5. Palpation should then be performed with the left hand. The reverse is applied when examining the left axilla.
6. Examination of axilla should cover the pectoral (anterior), central (medial), subscapular (posterior), humoral (lateral), and apical groups of lymph nodes. An example of a systematic routine you could follow is listed below:
- With your palm facing towards you, palpate behind the lateral edge of the pectoralis major (pectoral/anterior).
- Turn your palm medially and with your fingertips at the apex of the axilla palpate against the wall of the thorax (central/medial) using the pulps of your fingers.
- Facing your palm away from you now, feel inside the lateral edge of latissimus dorsi (subscapular/posterior).
- Palpate the inner aspect of the arm in the axilla (humoral/lateral).
- Reach upwards into the apex of the axilla with fingertips (warn the patient this may be uncomfortable).
7. Repeat assessment on the contralateral axilla.
Other lymph nodes
Finally, examine the following groups of lymph nodes:
- Cervical lymph nodes
- Supraclavicular lymph nodes
- Infraclavicular lymph nodes
- Parasternal lymph nodes
See our lymphoreticular examination for more details.
To complete the examination…
Explain to the patient that the examination is now finished and provide them with privacy to get dressed.
Thank the patient for their time.
Dispose of PPE appropriately and wash your hands.
Summarise your findings.
Example summary
“Today I examined Mrs Smith, a 64-year-old female. On general inspection, the patient appeared comfortable at rest and there were no objects or medical equipment around the bed of relevance.”
“Closer inspection of the chest did not reveal any scars or breast abnormalities.”
“Palpation of the breast did not reveal any masses and there was no regional lymphadenopathy.”
“In summary, these findings are consistent with a normal breast examination.”
“For completeness, I would like to perform the following further assessments and investigations.”
Further assessments and investigations
Suggest further assessments and investigations to the examiner:
- Mammography: typically used in patients over the age of 35.
- Ultrasound: typically used in patients under the age of 35 due to increased density of breast tissue making mammography less effective.
- Biopsy: fine-needle aspiration or core biopsy may be considered if a breast lump needs further histological assessment.
References
- Hic et nunc. Adapted by Geeky Medics. Breast cancer. Licence: CC BY-SA.
- Lily Chu, National Naval Medical Center Bethesda. Adapted by Geeky Medics. Paget’s disease of the nipple.
- Université Laval. Adapted by Geeky Medics. Peu d’orange. Licence: CC BY-SA.
- LizArranda. Adapted by Geeky Medics. Congenital nipple inversion. Licence: CC BY-SA.