- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Bronchiectasis is a chronic respiratory disease characterised by permanent bronchial dilation, due to irreversible damage to the bronchial wall.1
In the UK, the prevalence of bronchiectasis is 3 per 1000, and 60% of diagnoses are in patients over the age of 70. The prevalence of bronchiectasis in the UK has increased by 60% over the last 20 years.2,3
Patients with mild bronchiectasis often have normal life expectancies. The mortality risk increases in patients with more frequent exacerbations and worse lung function.4
Aetiology
Pathophysiology
The pathogenesis of bronchiectasis is poorly understood. An initial insult to the bronchi (e.g. infection) results in immune cells being recruited to the bronchi. These immune cells secrete cytokines and proteases, leading to inflammation in the bronchi.
This inflammation damages the muscle and elastin found in the bronchial walls, leading to bronchial dilation.
In most people, this bronchial dilation is reversible after the resolution of the initial insult to the bronchi. However, in patients with bronchiectasis, several factors prevent the bronchial dilation from reversing (e.g. impaired mucociliary clearance and dysregulated immunity).7
Dilated bronchi are predisposed to persistent microbial colonisation, as mucus traps in the dilated bronchi (figure 1).
Therefore, bronchiectasis patients get caught in a vicious cycle, whereby their airways are colonised by micro-organisms, which increases bronchial inflammation, worsening their bronchiectasis, leading to increased susceptibility to airway colonisation.8

Causes of bronchiectasis
There is a wide range of possible underlying causes of bronchiectasis, which are summarised below.
Post-infectious (most common cause):
- Recurrent childhood lower respiratory tract infections (e.g. influenza, pertussis and measles)
- Pulmonary tuberculosis
- Allergic bronchopulmonary aspergillosis (ABPA)
Pulmonary disease:
- Chronic obstructive pulmonary disease
- Asthma (especially in patients with frequent exacerbations and neutrophilic asthma)5
Congenital:
- Cystic fibrosis
- Primary ciliary dyskinesia
- Alpha-1 antitrypsin deficiency (also causes emphysema)
Connective tissue disease:
- Rheumatoid arthritis
- Systemic lupus erythematosus (SLE)
- Sarcoidosis
Idiopathic (40% of bronchiectasis)6
Risk factors
Risk factors for bronchiectasis include:
- Age (>70 years)
- Female gender
- Smoking history
Clinical features
History
Typical symptoms of bronchiectasis include:10
- Daily cough, producing copious amounts of mucopurulent sputum (haemoptysis is present in 50% of patients)
- Exertional dyspnoea, which may progress to resting dyspnoea
- Fatigue
- Rhinosinusitis symptoms (such as nasal discharge, nasal obstruction and facial pressure): due to underlying mucociliary impairment
Other important areas to cover in the history include:
- History of childhood lower respiratory tract infections: you may forget to ask this if the patient is elderly
- Family history: ask about congenital conditions (such as cystic fibrosis) and autoimmune conditions (such as rheumatoid arthritis)
- Smoking history: quantify in pack-years (1 pack-year = smoking 20 cigarettes a day for a year)
Clinical examination
A full respiratory examination should be performed in suspected cases of bronchiectasis.
Typical clinical findings in bronchiectasis include:
- Finger clubbing: due to increased secretion of growth factors, leading to increased growth of extracellular matrix in the nails11
- Course crepitations, present in expiration and inspiration: caused by sudden opening and closing of the airways12
- Rhonchi (low-pitched noises, which sound like snoring): caused by the movement of secretions in the large airways
- High-pitched inspiratory squeaks and pops: unclear aetiology

Differential diagnoses
The main presenting complaint of bronchiectasis (chronic productive cough) has important differential diagnoses.
Table 1 outlines these differential diagnoses, and the features which differentiate them from bronchiectasis.
Table 1. Differential diagnoses of bronchiectasis
|
Differential diagnosis |
Features differentiating from bronchiectasis |
|
Reduced breath sounds Absence of high-pitched inspiratory squeaks CT chest may be normal |
|
|
Diurnal variation in symptoms and peak flow History of atopy Lung function tests: bronchodilator reversibility |
|
|
Pneumonia |
More acute presentation (over days, rather than months or years) Chest X-ray: consolidation |
|
Chronic sinusitis |
Vesicular breath sounds Radiological investigations: normal |
Investigations
Bedside investigations
Relevant bedside investigations include:
- Pulse oximetry: aim for 94-98% initially, but the target saturations may be reduced in advanced disease (this is a risk-benefit judgement made by a senior clinician)
- Sputum culture: common organisms isolated include Pseudomonas aeruginosa and Haemophilus influenza. Pseudomonas is particularly common, as it forms biofilms which protect it from the immune system and antibiotics.14
- Lung function tests: typically show an obstructive pattern (FEV1/FVC ratio < 70%), but may be normal
- Echocardiogram: bronchiectasis may impair ventricular function and lead to pulmonary hypertension15
Laboratory investigations
Relevant laboratory investigations include:
- Full blood count: may show elevated white blood cell count, including neutrophilia
- CRP: may be elevated during acute exacerbations
- Autoimmune screen (if suspecting an autoimmune condition): includes anti-CCP, ANA and ANCA
- Specific IgE to Aspergillus fumigatus: if suspecting ABPA
- Genetic testing (done in specialist units): to diagnose congenital disorders, such as cystic fibrosis and primary ciliary dyskinesia
Imaging
Relevant imaging investigations include:
- Chest X-ray: required to exclude other pathologies. Chest X-ray may be normal in mild bronchiectasis. Signs in severe disease include tram lines and ring shadows.
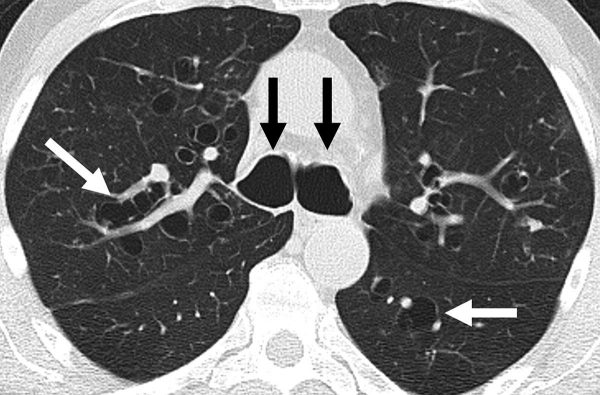
- High-resolution CT chest (figure 3): gold-standard imaging test. Shows bronchial dilation, with or without airway thickening.16
- Bronchoscopy (figure 4): used in patients with localised bronchiectasis, as this may be caused by foreign body aspiration or an endobronchial lesion.17
Management
Conservative management
Conservative management options for bronchiectasis include:
- Pulmonary rehabilitation: refer the patient to a respiratory physiotherapist, who will teach the patient airway clearance techniques (which offload mucus from the airways)
- Smoking cessation: see the Geeky Medics guide on smoking cessation
- Annual influenza vaccination and one-off pneumococcal vaccination
Medical management
Medical management options for bronchiectasis include:
- Mucoactive agents (e.g. nebulised saline and carbocisteine): aid the clearance of sputum, for patients who have difficulty expectorating sputum (such as frail, elderly patients)17
- Long-term antibiotics (e.g. azithromycin three times a week): may be used in patients who have three or more exacerbations per year, after consultation with a respiratory specialist1
- Bronchodilators: offer a long-acting bronchodilator (e.g. formoterol) in patients with activity-limiting dyspnoea
- Specific treatments for underlying conditions: CFTR modulator therapies (e.g. Trikafta) can be used in cystic fibrosis
- Long-term oxygen therapy: if saturations on room air are <88% or PaO2 on room air is <7.3kPa
Surgical management
Surgical management options for bronchiectasis include:
- Lung resection: for localised bronchiectasis, not controlled by optimum medical management
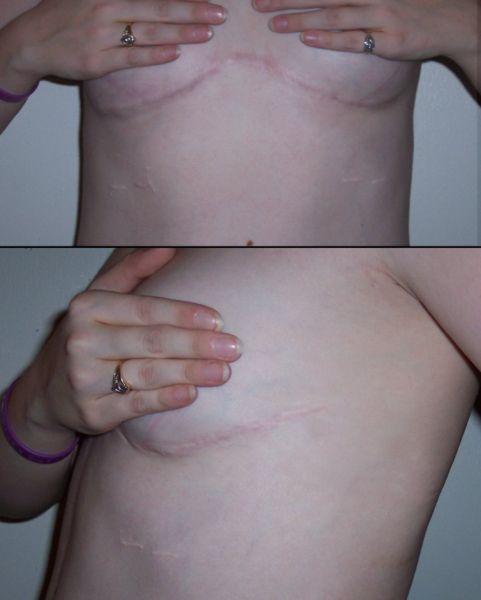
- Lung transplant (figure 5): for patients younger than 65, with rapid deterioration despite optimum medical management17
Complications
Disease-related complications of bronchiectasis include:
- Respiratory failure: due to failure of gas exchange in the lungs
- Massive haemoptysis (>250ml per day): often due to rupture of a bronchial artery into a bronchus21
- Anxiety and depression: due to impaired quality-of-life
Treatment-related complications of bronchiectasis include:
- Macrolides: long QT syndrome, tinnitus and hearing loss
- Lung transplant: immediate complications (e.g. blood loss), early complications (e.g. transplant rejection) and late complications (e.g. post-transplantation lymphoproliferative disorder)
Key points
- Bronchiectasis is a chronic respiratory disease characterised by permanent bronchial dilation, due to irreversible damage to the bronchial wall.
- Bronchiectasis is commonly caused by respiratory infections, but can be caused by systemic conditions.
- The main symptoms are chronic productive cough (with mucopurulent sputum) and dyspnoea.
- A diagnosis of bronchiectasis is based on radiological findings, with high-resolution CT chest being the gold-standard diagnostic investigation.
- Management includes respiratory physiotherapy, mucoactive agents and long-term antibiotics.
- The main complication of bronchiectasis is respiratory failure.
Reviewer
Dr Neeraj Shah
Respiratory medicine registrar
Editor
Dr Chris Jefferies
Feedback
Please click here to fill out the feedback form, which should take less than 1 minute of your time. Feedback is vital as it allows authors to improve their articles, leading to even better content on Geeky Medics!
References
- National Institute for Health and Care Excellence. Bronchiectasis: Clinical Knowledge Summary. Published in 2020. Available from: [LINK]
- Snell et al. Epidemiology of bronchiectasis in the UK: Findings from the British Lung Foundation’s “Respiratory Health of the Nation” project. Respiratory Medicine. Published in 2019. Available from: [LINK]
- Quint J et al. Changes in the incidence, prevalence and mortality of bronchiectasis in the UK from 2004-2013: a population-based cohort study. European Respiratory Journal. Published in 2016. Available from: [LINK]
- Loebinger M et al. Mortality in bronchiectasis: a long-term study assessing the factors influencing survival. European Respiratory Journal. Published in 2009. Available from: [LINK]
- Contarini M et al. Bronchiectasis: a case-based approach to investigation and management. European Respiratory Review. Published in 2018. Available from: [LINK]
- Swenson C et al. What is bronchiectasis? American Journal of Respiratory and Critical Care Medicine. Published in 2017. Available from: [LINK]
- Chalmers J et al. Bronchiectasis. Nature Reviews Disease Primers. Published in 2018. Available from: [LINK]
- Cole PJ. Inflammation: a two-edged sword – the model of bronchiectasis. European Journal of Respiratory Disease. Published in 1986. Available from: [LINK]
- National Heart, Lung and Blood Institute. Bronchiectasis Diagram. License: [Public domain]. Available from: [LINK]
- BMJ Best Practice. Bronchiectasis. Published in 2020. Available from: [LINK]
- Sarkar M et al. Digital Clubbing. Lung India. Published in 2012. Available from: [LINK]
- Sarkar M et al. Auscultation of the respiratory system. Annals of Thoracic Medicine. Published in 2015. Available from: [LINK]
- Desherinka D. Finger clubbing. Licence: [CC BY-SA]. Available from: [LINK]
- Finch S. A comprehensive analysis of the impact of Pseudomonas aeruginosa colonization on prognosis in adult bronchiectasis. Annals of the American Thoracic Society. Published in 2015. Available from: [LINK]
- Gencer M. Impact of bronchiectasis on right and left ventricular function. Respiratory Medicine. Published in 2006. Available from: [LINK]
- Tiddens HWM et al. The radiological diagnosis of bronchiectasis: what’s in a name? European Respiratory Review. Published in 2020. Available from: [LINK]
- Hill AT et al. British Thoracic Society Guideline for bronchiectasis in adults. Thorax. Published in 2019. Available from: [LINK]
- Mcgfowler. Bronchiectasis CT Scan. Licence: [CC BY-SA]. Available from: [LINK]
- Cancer Research UK. Bronchoscopy. License: [Public domain]. Available from: [LINK]
- ImGz. Clamshell Incision. Licence: [CC BY-SA]. Available from: [LINK]
- Camacho JR and Prakash UBS. 46-year-old man with chronic haemoptysis. Mayo Clinic Proceedings. Published in 1995. Available from: [LINK]