- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
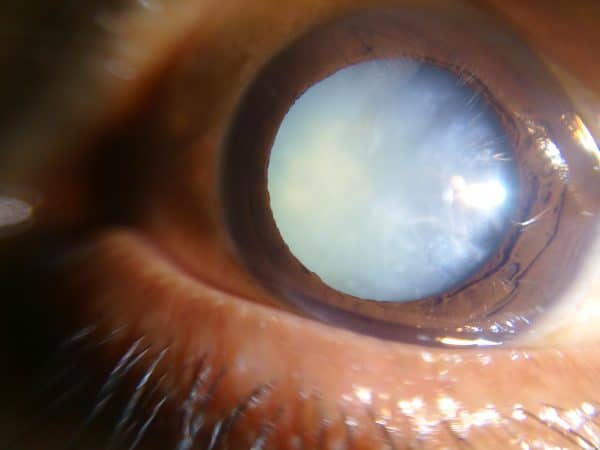
A cataract is an opacification or clouding of the lens. It is the most common cause of blindness worldwide.
Cataracts can affect people of all ages, but they are particularly prevalent in elderly patients. Cataracts are found in 75% of people over 65 years old.1
Aetiology
Anatomy
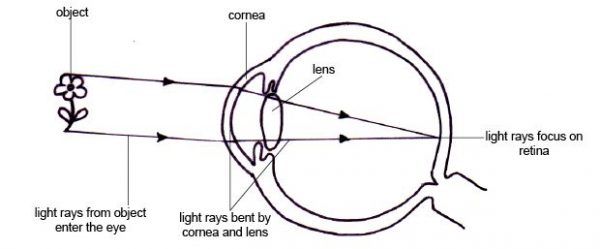
The lens helps to focus light onto the retina.
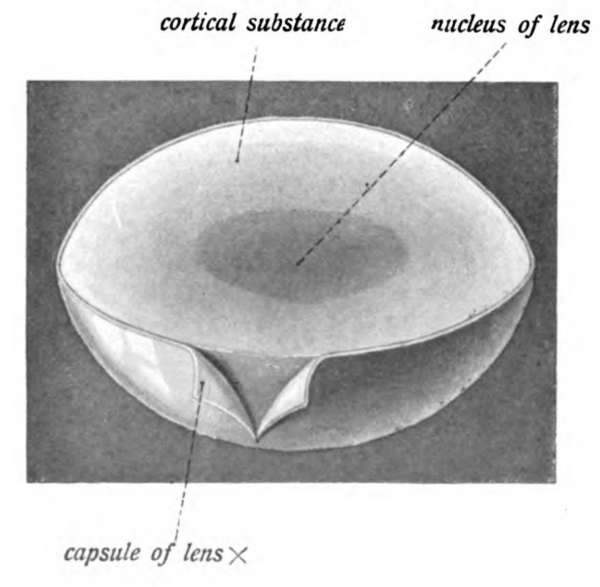
There are three main anatomical structures of the lens relevant to cataracts:
- Lens nucleus: middle aspect of the lens
- Lens cortex: outer aspect of the lens
- Lens capsule: the membrane surrounding the lens
Types of cataracts
There are three main types of cataracts, classified according to the part of the lens affected.
Nuclear cataracts
Nuclear cataracts are caused by sclerosis of the lens nucleus and are common in old age.
Symptoms include myopia (short-sightedness) and colours appearing dull.
Myopia occurs as sclerosis changes the lens refractive index. Patients experiencing this symptom will often say that they previously needed reading glasses, but no longer require them.
Cortical cataracts
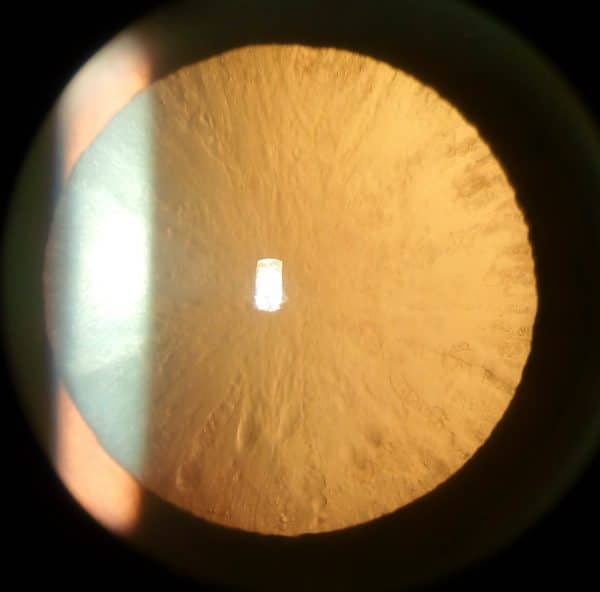
Cortical cataracts are caused by opacifications of the lens cortex.
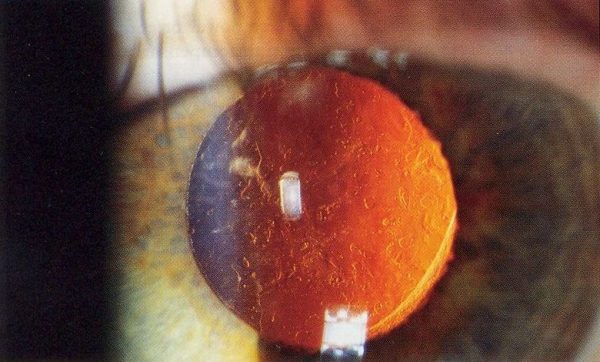
On ophthalmoscopy, the opacifications look like the spokes of a wheel around the edge of the lens (Figure 3). Vision is often unaffected.
Posterior subcapsular cataracts
Posterior subcapsular cataracts are caused by opacifications in the posterior aspect of the lens capsule. These typically affect younger patients and individuals taking steroids.
Patients complain of glare when looking at lights (this can cause issues when driving at night). Posterior subcapsular cataracts often progress more rapidly than other types of cataracts.
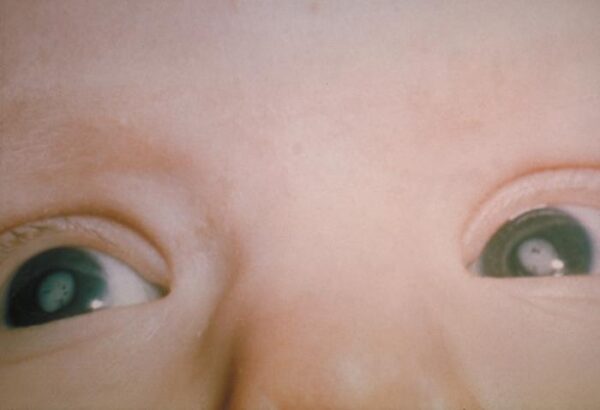
Congenital cataracts
Congenital cataracts are present from birth. They are associated with infection (typically congenital rubella syndrome) and genetic predisposition.
These are often diagnosed during the newborn examination due to the absence of the fundal reflex.
Patients must be urgently referred to ophthalmology, as surgical management may be required in the first 6 weeks of life to prevent amblyopia (permanent visual loss due to the brain neglecting the eye).
Risk factors
Most cataracts are associated with age-related changes.
Other risk factors for cataracts include:
- Diabetes
- Steroid use
- UV exposure
- Smoking
- Ocular trauma
- Genetic predisposition
Clinical features
History
Typical symptoms of cataracts include:
- Progressive blurring of vision
- Glare when looking at lights
- Colours appearing dull
For more information on ophthalmic history taking, see the Geeky Medics guide here.
Clinical examination
Typical clinical findings on eye examination include:
- Reduced red reflex (elicited by shining a light into the eye)
- Clouded lens
Differential diagnoses
Differential diagnoses to consider in the context of cataracts include:
- Open-angle glaucoma
- Macular degeneration
Investigations
Cataracts are a clinical diagnosis made following history and clinical examination.
Slit-lamp examination with dilated pupils can be used to support the diagnosis.
Management
Conservative management
Cataracts often begin small with mild symptoms and progress over several years.
NICE recommends refraining from surgical management until symptoms affect lifestyle.
Controlling risk factors such as diabetes, smoking, steroid use, and UV exposure may slow down the development of cataracts.
Surgical management
Phacoemulsification with an intraocular lens implant is the most common cataract surgery.
The opacified lens is broken down using ultrasound and the fragments are aspirated. A new lens is then implanted. This is often conducted under local anaesthetic.
Prior to surgery, ocular biometry is conducted to measure the corneal curvature and the shape of the eye. It is used to choose a suitable replacement lens.
Complications
If not managed appropriately, cataracts can cause loss of vision.
Surgical complications
Complications following surgical management of cataracts include:
- Posterior capsule opacification is common. Patients present months to years after cataract surgery complaining that it seems like their cataract is returning. It is treated with a capsulotomy, where lasers are used to make a hole in the capsule to allow light to pass through.
- Endophthalmitis is an infection of the aqueous and/or vitreous humour. It is a rare, severe complication and can result in visual loss. Endophthalmitis is treated with intraocular antibiotic injections.
Key points
- A cataract is an opacification of the lens. It is a common cause of vision loss.
- Cataracts typically present with a progressive blurring of vision.
- Controlling risk factors such as diabetes, smoking, steroid use, and UV exposure may slow down the development of cataracts.
- Surgical management involves phacoemulsification and intraocular lens implant.
- Surgical complications include posterior capsule thickening and endophthalmitis.
- Congenital cataracts must be urgently referred to ophthalmology to prevent the development of amblyopia.
Editor
Dr Chris Jefferies
References
- Oxford handbook of clinical specialties tenth edition. Ophthalmology chapter page 446-447. Published in 2016.
- Sunshine Connelly (description by Ruth Lawson). Lens function. [CC BY]. Available from: [LINK].
- Johannes Sobotta. Lens anatomy (modified by Jonathan Malcolm). Published 2nd November 2013. Licence: Public Domain. Available from: [LINK].
- Imran Kabir Hossain. Cortical cataract. Published 31st May 2017. [CC BY]. Available from: [LINK]
- Imran Kabir Hossain. Dense white mature cataract. Published 11th April 2017. [CC BY]. Available from: [LINK].
- Rakesh Ahuja. Posterior capsular opacification post-cataract surgery (seen on retro-illumination). Published 10th September 2006. [CC BY] Available from: [LINK].
- Congenital cataract. Published 29th May 206. Licence: Public Domain. Available from: [LINK].
- The Duke Elder exam of ophthalmology: a comprehensive guide for success. Page 111-117. Published July 2019.
- EyeWiki, Cataract. Last edited January 2020. Available from: [LINK].