- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Completing a death certificate, formally called a Medical Certificate of Cause of Death (MCCD), is a common OSCE station and something you will need to be able to do as a junior doctor. This guide will cover what to do when a patient has died, and you are asked to complete a death certificate.
What to do when a patient has died
Assess the patient and confirm the death, clearly documenting this in the notes (see our guide).
Discuss the death with the consultant in charge of the patient’s care – this will help to clarify the cause to be written on the certificate.
Liaise with the bereavement office to organise an appropriate time to attend with the patient’s medical notes to complete the death certificate and other paperwork.
Perform a full external examination of the patient’s body in the mortuary to ensure no implantable devices are present.
Death certificate example
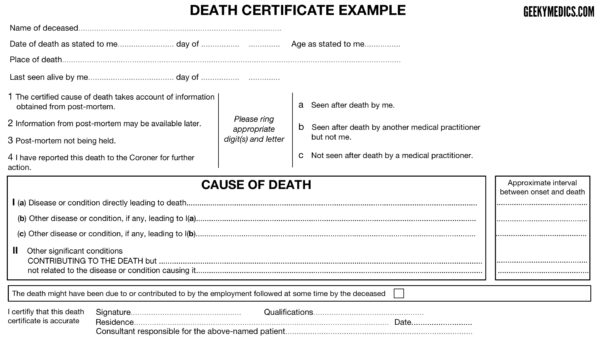
We have included an example of a blank death certificate below. You can also download a PDF copy for OSCE practice.
Completing the death certificate
Personal details of the deceased
Age
You should record the age of the deceased in completed years or, if under one year, in completed months.
Place of death
You should record to the best of your knowledge the precise place of death (e.g. the name of the hospital, or a private address).
Circumstances of certification
Last seen alive by me
Record the date you last saw the deceased alive.
Information from post-mortem
Indicate if the cause of death takes into account information gained from a post-mortem.
Seen after death
Indicate who saw the deceased after death.
Part I – Cause of death
Consider the main causal sequence of conditions that lead to death.
The disease or condition that led directly to death should be documented on the 1a line. You should then work your way back through the other diseases that led to the eventual cause of death until you reach the underlying cause of death which initiated this chain of events. The lowest completed line in part 1 should, therefore, contain the underlying cause of death.
Some deaths may have only one condition that lead directly to death, such as a subarachnoid haemorrhage. In these cases, it’s acceptable to complete only line 1a.
When stating the cause of death, be as specific as possible given the information you have. An example might be stating “Adenocarcinoma of the right main bronchus” rather than “Lung cancer”.
In some circumstances, there can be two separate conditions that led directly to death and in these cases, you should enter them both on the same line and then in brackets state that these are joint causes of death.
A few things that you CAN NOT write as a 1a:
- “Failures” as a sole 1a (e.g. heart/kidney/liver/respiratory failure). However, it is ok to use congestive cardiac failure.
- Asphyxia
- Asthenia
- Cachexia
- Cardiac arrest
- Coma
- Exhaustion
- Old age/frailty as a sole cause of death: this can only be used in patients over 80 years old.
Part II – Conditions that may have contributed to the death
Part II allows you to document other conditions that were not part of the main causal sequence of death but likely played a role in hastening the death. An example might be ischaemic heart disease in a patient who died of pneumonia.
It is NOT somewhere where you should list the patient’s entire past medical history.
Cause of death list
The Royal College of Pathologists publishes a cause of death list listing acceptable conditions which may be included on the death certificate. It is important to remember this is not an exhaustive list. The cause of death list also provides guidance on when a death should be referred to the Coroner.
Other details at the bottom of the certificate
You should sign the death certificate and print your name in block capital letters beside it. Your GMC number should also be included beside or under your name.
Document your GMC approved qualifications (e.g. MBBS Medicine and Surgery).
The residence is typically the hospital’s address (not your own personal address).
If the patient died in hospital, document the consultant’s name on the little line at the bottom of the certificate (this is easily missed).
Counterfoil
There is a counterfoil on the left-hand side which gets left in the death certificate book.
You need to document the patient’s name, the cause of death (Part 1) and conditions potentially contributing to death (Part 2).
You also need to document your personal details again.
Other tips
_____ day of ______ refers to the “5th” day of “April 2015” (sounds simple, but I know someone who wrote “Tuesday” in an OSCE).
1a should be the disease, illness or complication which led to death and not a mode of dying.
Circle either 1, 2 or 3 and a, b or c with regards to a post-mortem.
The back of the death certificate
There are two boxes on the back of the death certificate that you may need to complete in certain circumstances:
Box A
If you have referred a death to the coroner put your initials here. If you have discussed the case with the coroner and they have said no referral is required, then you DO NOT need to complete this box.
Box B
If you may be in a position to provide more information about the cause of death in the future then you need to initial this box. This is the case when there are pending investigations not yet back or performed (e.g. histology, microbiology culture results, genetic analysis, post-mortem information). A request for this information will be sent to the consultant responsible for the patient.
Reasons to refer to the Coroner
There are several situations in which a patient’s death should be referred to the Coroner including:
- The death was due to poisoning including by an otherwise benign substance
- The death was due to exposure to, or contact with a toxic substance
- The death was due to the use of a medicinal product, the use of a controlled drug or psychoactive substance
- The death was due to violence, trauma or injury
- The death was due to self-harm
- The death was due to neglect, including self-neglect
- The death was due to a person undergoing any treatment or procedure of a medical or similar nature
- The death was due to an injury or disease attributable to any employment held by the person during the person’s lifetime
- The person’s death was unnatural but does not fall within any of the above circumstances
- The cause of death is unknown
- The registered medical practitioner suspects that the person died while in custody or otherwise in state detention
- There was no attending registered medical practitioner, and there is no other registered medical practitioner to sign a medical certificate cause of death in relation to the deceased person
- The attending medical practitioner is not available within a reasonable time of the person’s death to sign the certificate of cause of death
- The identity of the deceased person is unknown
The Notification of Deaths Regulations (2019)
In the UK, the Notification of Deaths Regulations (2019) set out the circumstances in which a death should be reported to the Coroner. The Ministry of Justice has published guidance for doctors on the regulations which provide more detail on when a death should be reported to the coroner.
How to refer to the Coroner
Coroners are often lawyers and occasionally doctors, or dual-qualified. Talk to the bereavement team within the hospital for advice on how to contact the local Coroner’s office.
Cases
We have included several scenarios to allow you to practice completing death certificates. You may want to print out some copies of the blank death certificate to use for each scenario.
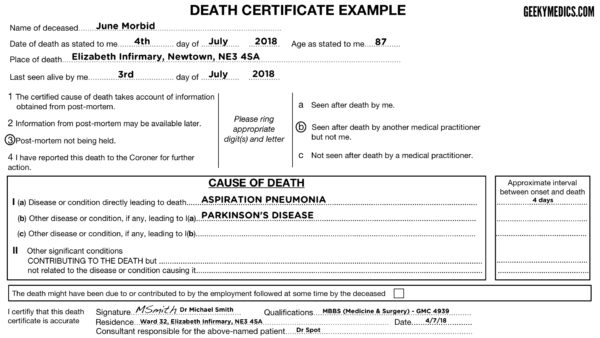
Case 1
Mrs June Morbid was an 87-year-old lady, whom you last attended to yesterday on the ward round with the consultant (Dr Spot). She had advanced Parkinson’s disease and was admitted 4 days previously with aspiration pneumonia. Unfortunately, the pneumonia did not respond to antibiotic treatment and the decision to palliate was made by the consultant after discussion with the family. Mrs Morbid peacefully passed away last night with her family around her, and her death was verified by your colleague on the night shift. You have been asked to fill in the death certificate after your ward round.
Cremation form 4
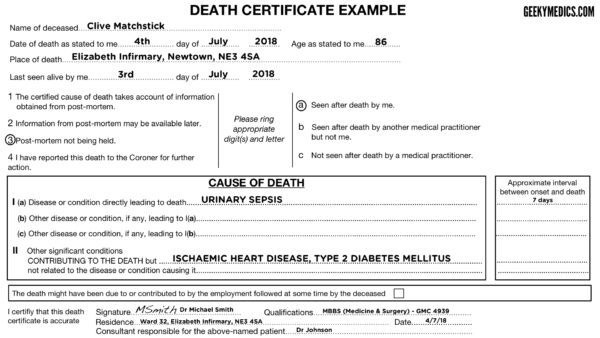
Case 2
Mr Clive Matchstick (86-years-old) was admitted to the ward a week ago from a local nursing home having vomited and whilst in hospital, he developed urinary incontinence and sepsis. He was treated for urosepsis, under the care of Dr Johnson, but unfortunately, he passed away. You confirmed his death this morning and you had also reviewed him last night before going home. He has a past history of ischaemic heart disease, type 2 diabetes mellitus, Charcot’s deformity of the left foot and amputation of the big toe on the right foot.
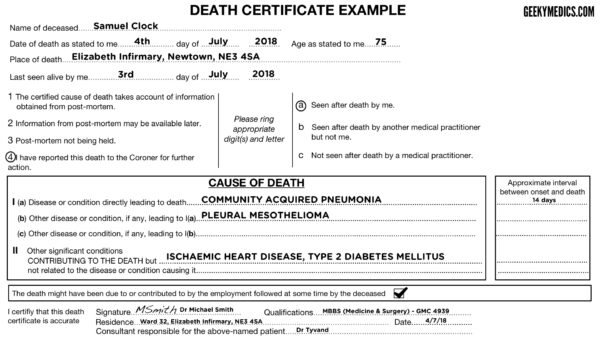
Case 3
Mr Samuel Clock (75-years-old) had been an in-patient on the ward you are working on for 2 weeks. He was being treated for community-acquired pneumonia (CURB-65 score of 4). His condition had progressively worsened when you reviewed him with his consultant Dr Tyvand last night and the decision was made to switch to a palliative approach of management. He passed away this morning, with his wife by his side. You confirmed his death on the ward. He has a past medical history of ischemic heart disease, hypertension, mesothelioma, type 2 diabetes and benign prostate hypertrophy.
This is a trick question…
This is a situation where the medical practitioner should have a conversation with the Coroner prior to issuing any certificate of cause of death as a post-mortem will most likely be required. Mesothelioma is almost always attributed to asbestos exposure and therefore falls into the category of a disease that is related to an occupation which may have contributed to the death. The damage most often occurs 20 – 60 years after asbestos exposure. It would be very unlikely that you would issue a death certificate, but if the Coroner instructed that you could do so, it might look a bit like this.
References
- The Royal College of Pathologists. Cause of death list. 2020. Available from: [LINK]
- HM Passport Office. Completing a medical certificate of cause of death (MCCD). 2022. Available from: [LINK]
- Ministry of Justice. Guidance for registered medical practitioners on the Notification of Deaths Regulations. 2022. Available from: [LINK]