- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Cervical screening (previously known as a smear test) frequently appears in OSCEs, and you’ll be expected to demonstrate excellent communication and practical skills. This guide provides a step-by-step approach to performing cervical screening in an OSCE setting, with an included video demonstration.
Cervical screening involves an initial test for the human papillomavirus (HPV). If HPV is detected on the cervical screening sample, cytology is performed to assess for dyskaryosis. For more information, see the Geeky Medics guide to cervical cancer and cervical intraepithelial neoplasia (CIN).
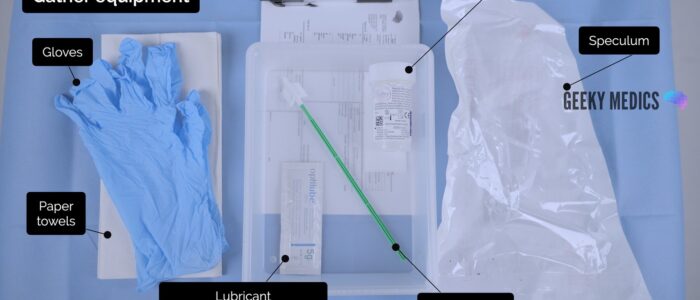
Gather equipment
Gather the appropriate equipment:
- Gloves
- Speculum
- A light source
- Endocervical brush
- Sample pot (liquid-based cytology)
- Paper towels
- Lubricant*
*Use of lubricant should be avoided when taking a cervical smear sample due to the risk of contamination. However, if lubricant is required, only a carbomer-free product that is recommended by the manufacturer of the cervical screening kit should be used (e.g. OptiLube Zero a.k.a. CerviLube for Hologic ThinPrep).10
Introduction
Wash your hands and don PPE if appropriate.
Introduce yourself to the patient including your name and role.
Confirm the patient’s name and date of birth.
Explain what the procedure will involve using patient-friendly language: “Today I need to perform a cervical screening test. This looks for the presence of a virus called HPV (human papillomavirus). If HPV is found, the lab will perform another test on the sample (cytology) to look for any abnormal cells caused by the virus. If abnormal cells are seen, you may need further investigations.
The procedure will involve me inserting a small plastic device called a speculum into the vagina. This will allow me to visualise the neck of the womb (your cervix). I will then place a very small brush into the vagina and take a sample of cells from the neck of the womb. It shouldn’t be painful, but it will feel a little uncomfortable. You can ask me to stop at any point. You may experience some light vaginal bleeding after the procedure.”
Explain the need for a chaperone: “One of the female ward staff members will be present throughout the examination, acting as a chaperone, would that be ok?”
Gain consent to proceed with the examination: “Do you understand everything I’ve said? Do you have any questions? Are you happy for me to carry out the procedure?”
Ask the patient if they have any pain or if they think they may be pregnant before proceeding with the clinical examination. Establish their last menstrual period (cervical screening is not recommended during menstruation).
Provide the patient with the opportunity to pass urine before the examination.
Explain to the patient that they’ll need to remove their underwear and lie on the clinical examination couch, covering themselves with the sheet provided.
Provide the patient with privacy to undress and check whether it is okay to re-enter the room before doing so.
Preparation
1. Wash your hands
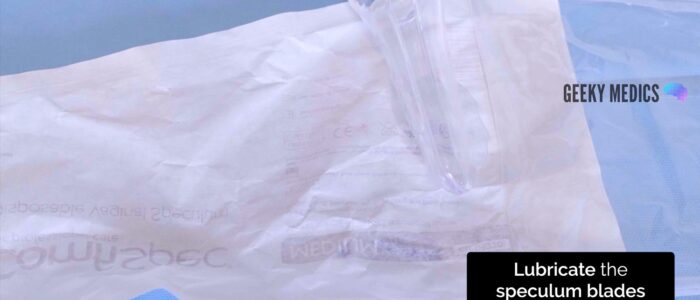
2. Open the speculum packaging whilst avoiding touching the speculum or the inner surface of the packaging
3. Open the lubricant (if being used) onto the inner surface of the speculum packaging
Position the patient
1. Re-check consent and that the patient is happy to proceed with the procedure: “I’m going to move on and examine your genitals. Are you happy for me to do this?”
2. Position the patient in the modified lithotomy position: “Draw your ankles up towards your buttocks, keep your feet flat on the bed, and then let your legs fall open”
Vulval inspection
It is good practice to inspect the vulva for any abnormalities
1. Don a pair of non-sterile gloves and an apron
2. Expose the patient’s external genitalia and ensure there is adequate lighting
Inspect the vulva
Inspect the vulva for abnormalities:
- Ulcers: typically associated with genital herpes
- Abnormal vaginal discharge: causes include candidiasis, bacterial vaginosis, chlamydia and gonorrhoea
- Scarring: may relate to previous surgery (e.g. episiotomy) or lichen sclerosus (scarring with associated abnormal architecture)
- Vulvovaginal atrophy: most commonly occurs in postmenopausal women
- White lesions (leukoplakia): may be patchy or in a figure-of-eight distribution around the vulva and anus, associated with lichen sclerosus
- Other lesions: causes include folliculitis, molluscum, genital warts and vulval malignancy
- Masses: causes include Bartholin’s cyst and vulval malignancy
- Varicosities: varicose veins secondary to chronic venous disease or obstruction in the pelvis (e.g. pelvic malignancy)
- Female genital mutilation: total or partial removal of the clitoris and/or labia and/or narrowing of the vaginal introitus
Female genital mutilation
The WHO defines female genital mutilation (FGM) as “all procedures that involve partial or total removal of the external female genitalia, or other injury to the female genital organs for non-medical reasons”.5
Over 200 million girls and women worldwide have undergone FGM.5 Women attending maternity, family planning, gynaecology, and urology clinics (among others) should be asked routinely about the practice of FGM.6 In the UK, healthcare professionals must report cases of FGM in girls under the age of 18 to the police.7
Bartholin’s cyst
Bartholin’s glands are responsible for producing secretions which maintain vaginal moisture and are typically located at 4 and 8 o’clock in relation to the vaginal introitus. These glands can become blocked and/or infected, resulting in cyst formation. Typical findings on clinical examination include a unilateral, fluctuant mass, which may or may not be tender.
Lichen sclerosus
Lichen sclerosus is a chronic inflammatory dermatological condition that can affect the anogenital region in women. It presents with pruritis and clinical examination typically reveals white thickened patches. Destructive scarring and adhesions develop causing distortion of the normal vaginal architecture (shrinking of the labia, narrowing of the introitus, obscuration of the clitoris).
Abnormal vaginal discharge
There are several causes of abnormal vaginal discharge including:
- Bacterial vaginosis: a thin, profuse fishy-smelling discharge without pruritis or inflammation
- Candidiasis: a curd-like, non-offensive discharge with associated pruritis and inflammation
- Chlamydia and gonorrhoea (symptomatic): a purulent vaginal discharge with or without associated inflammation
- Trichomoniasis: an offensive yellow, frothy vaginal discharge with associated pruritis and inflammation
Inserting the speculum
Warn the patient that you are going to insert the speculum and ask if it is still okay for you to do so.
If the patient consents to continuing the procedure, prepare to insert the speculum. If using an approved lubricant (see equipment section for details), apply a small amount of product over the exterior sides of the speculum only, taking care to avoid the tip. This is to avoid contaminating and invalidating the sample.
Then, proceed to insert the speculum:
1. Carefully separate the labia using the thumb and index finger of your non-dominant hand
2. With the blades closed, gently insert the speculum. Usually, the speculum is inserted with the handle pointing sideways (at 9 or 3 o’clock)
3. Once inserted, rotate the speculum so that the handle is facing upwards
4. Open the speculum blades until an optimal view of the cervix is achieved
5. Tighten the locking nut to fix the position of the blades
Inspection of the cervix and vaginal walls
Inspect the cervix for:
- The cervical os: if open and the patient is pregnant, this may indicate an inevitable or incomplete miscarriage
- Erosions around the os: most commonly associated with ectropion; however, early cervical cancer can have similar appearances
- Cervical masses: typically associated with cervical malignancy
- Scarring: from a previous colposcopy procedure (e.g. LLETZ)
Inspect the cervix and vagina for:
- Ulceration: most commonly associated with genital herpes
- Atrophy: in post-menopausal patients
- Foreign body: for example, a retained tampon or condom
- Abnormal discharge: several possible causes, including bacterial vaginosis, vaginal candidiasis, trichomonas, chlamydia and gonorrhoea
Cervical ectropion
Cervical ectropion is a condition in which columnar epithelial cells (usually only located inside the cervical canal) are present on the outside of the vaginal cervix. Normally, the only cells on the outside of the vaginal cervix are squamous epithelial cells.
The areas of columnar epithelial cells appear red against the normal pink colour of the cervix and are often located around the external os. They are more prone to bleeding due to the presence of a network of delicate fine blood vessels, and patients often present with post-coital bleeding.
Cervical cancer
Cervical cancer is caused by persistent infection with human papillomavirus (HPV). Before the development of cervical cancer, the cells of the cervix can become dysplastic, a condition that is known as cervical intraepithelial neoplasia (CIN).
Cervical screening can identify patients infected with HPV and those who have gone on to develop CIN, allowing early treatment to prevent progression to invasive cervical cancer. Many women do not have symptoms in the early stages of cervical cancer, but symptoms can include vaginal bleeding (intermenstrual, post-coital), increased vaginal discharge and vaginal discomfort. Clinical examination typically reveals white or red patches on the cervix in early disease or a cervical ulcer or tumour in more advanced disease.
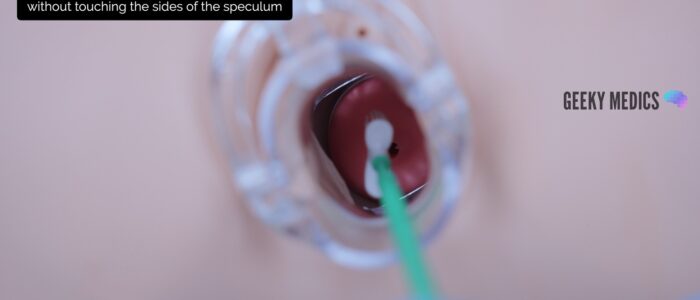
Cervical screening sample
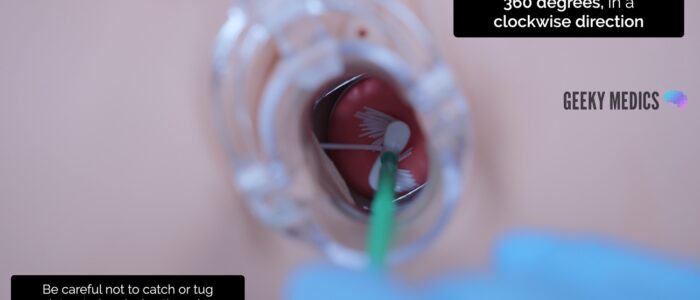
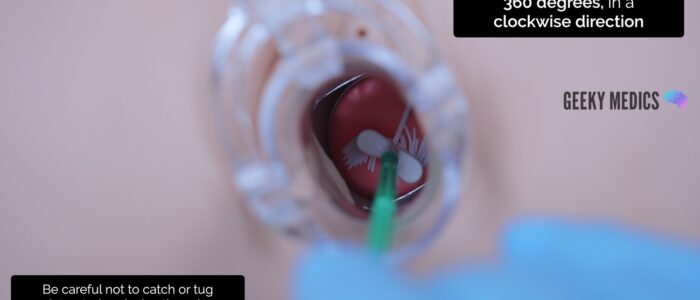
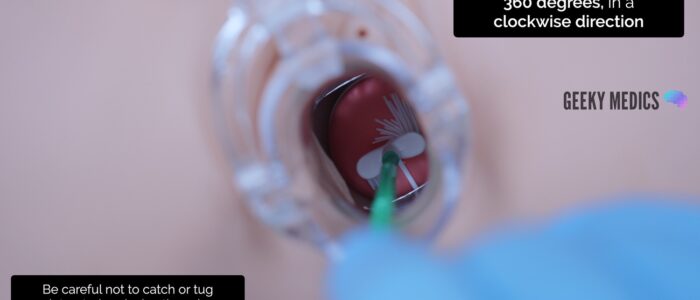
1. Insert the endocervical brush through the speculum into the endocervical canal, avoiding touching the sides of the speculum with the brush
2. Rotate the brush 360 degrees, in a clockwise direction, 5 times
3. Remove the endocervical brush, avoiding touching the speculum as you do so
4. Immediately transfer the sample to the liquid-based cytology container (follow local cytology guidelines for transferring the sample from the brush into the container)
5. Label the sample
Transferring the sample into the cytology container
It is important to follow local guidelines for transferring the cervical screening sample into the cytology container. Methods may include:
- Sweeping the brush against the sides and the base of the container (the ‘mash and bash’ technique), then discarding the entire brush
- Breaking off the tip of the brush and placing this into the container
Removing the speculum
1. With your non-dominant hand, hold the blades of the speculum whilst you loosen the locking nut with your dominant hand. This ensures the blades do not snap shut when the locking nut is loosened.
2. Gently remove the speculum whilst slowly closing the blades and inspecting the walls of the vagina
3. Cover the patient with the sheet, explain that the procedure is now complete and provide the patient with privacy so they can get dressed. Provide paper towels for the patient to clean themselves.
4. Dispose of the used equipment into a clinical waste bin
To complete the procedure…
Thank the patient for their time.
Dispose of PPE appropriately and wash your hands.
Complete the cytology request form.
Discuss the results process with the patient, including the average wait time for results and how the results will be communicated.
Document the procedure in the medical notes, including the details of the chaperone.
Summarise your findings.
Example summary
“Today I performed a routine cervical screening test on Mrs Smith, a 28-year-old female.“
“There were no abnormalities noted on inspection of the vulva and speculum examination revealed a healthy cervix with a closed external os. I was able to obtain an adequate sample for cervical screening.”
“In summary, these findings are consistent with a normal speculum examination. I have completed the cytology request form and labelled the sample appropriately.”
“I have explained the process for receiving results to the patient.”
Further assessments and investigations
Further assessments and investigations are not usually performed following routine cervical screening. If the cervix appears suspicious for cervical cancer, the patient must be referred urgently for assessment without waiting for the cervical screening results.
If the patient has specific symptoms, they will require further assessment. This may include:
- Urinalysis: including β-HCG to rule out pregnancy
- Bimanual vaginal examination: to palpate for masses and cervical motion tenderness
- Vaginal swabs/endocervical swabs: if there are concerns about infection (bacterial/viral)
- Ultrasound abdomen and pelvis: to further investigate pelvic pathology
Reviewers
Dr Ashley Jefferies
Community Sexual and Reproductive Health Registrar
Mr Isaac Magani
Consultant Obstetrician and Gynaecologist
References
- Medimage. Adapted by Geeky Medics. Bartholin’s cyst. Licence: CC BY-SA.
- Mikael Häggström. Adapted by Geeky Medics. Lichen sclerosus. Licence: CC0.
- Mikael Häggström. Adapted by Geeky Medics. Vaginal candidiasis. Licence: CC0.
- Mikael Häggström. Adapted by Geeky Medics. Uterine prolapse. Licence: CC0.
- WHO. Female Genital Mutilation. Key facts. Available from: [LINK].
- Erskine K; Collecting data on female genital mutilation. BMJ. 2014 May 13348:g3222. doi: 10.1136/bmj.g3222. Available from: [LINK].
- Department of Health and Social Care. FGM: mandatory reporting in healthcare. 2017. Available from: [LINK].
- GynaeImages. Adapted by Geeky Medics. Cervical ectropion. Licence: CC BY-SA.
- Haeok Lee, Mary Sue Makin, Jasintha T Mtengezo and Address Malata. Adapted by Geeky Medics. CIN-1. Licence: CC BY.
- ThinPrep Pap Test Lubricant Compatibility List. Hologic. Available from: [LINK].