- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
A chest drain (a.k.a. intercostal drain) involves inserting a plastic tube into the pleural cavity to drain air or fluid.
This guide provides a step-by-step approach to inserting a chest drain in an OSCE setting, it is NOT intended to be used to guide patient care.
Indications
Pleural effusion
Indications for inserting a chest drain for a pleural effusion include:
- Large benign effusion
- Malignant pleural effusion to improve symptoms and aid diagnosis, and prior to pleurodesis
- Empyema and complicated parapneumonic effusion
- Symptomatic pleural effusions which haven’t responded to medical treatment
Pneumothorax
Indications for inserting a chest drain for a pneumothorax include:
- Large primary spontaneous pneumothorax causing breathlessness
- Large secondary spontaneous pneumothorax in patients >50 years
- Traumatic pneumothorax (including haemopneumothorax)
- Persistent pneumothorax following simple aspiration
- Pneumothorax in any ventilated patient
Procedure-specific
Other indications for inserting a chest drain include:
- Talc pleurodesis
- Post-thoracic cavity procedures (e.g. medical thoracoscopy and thoracic, oesophageal, or cardiac surgery)
Gather equipment
Clean a procedure trolley using a disinfectant wipe.
Gather the equipment required for the procedure and place it on the clean bottom shelf of the trolley:
- Antiseptic solution with applicator (e.g. chlorhexidine applied with ChloraPrep™)
- Sterile drapes, gown, and gloves
- Sterile field (e.g. wound care pack)
- Sterile gauze
- 5-10ml local anaesthetic, such as 1% lidocaine
- 23G (blue) or 25G (orange) needle
- 21G (green) needle
- 10ml syringe x2
- Seldinger chest drain kit (12F suitable for most indications)
- Chest drain drainage bottles & tubes
- Sterile water for chest drain bottle
- Straight needle suture (non-absorbable 0 or 1/0 silk)
- Scalpel (if not included in chest drain kit)
- Transparent dressing
- Appropriate containers to collect fluid for microbiology, cytology, and biochemistry results (if a diagnosis is required)
- Ultrasound machine with sterile ultrasound probe sheath (for effusions)
Pre-procedure
Check for contra-indications
Check for any relative contra-indications prior to performing the procedure:
- Uncooperative patient
- Local skin infection at the site of fluid
- Bleeding disorder, anticoagulants, or coagulopathy (including INR >1.5 or platelets <50)
- No safe site for chest drain identified on thoracic ultrasound (effusion) or x-ray (pneumothorax)
- Unavailability of ultrasound operator (for pleural effusion)
As these are relative contra-indications, if any are present, a senior decision maker should determine whether the risk outweighs the benefit of the procedure, or whether there is a way to mitigate these risks.
For example, if a patient is taking anticoagulants but requires a chest drain, it would be down to a senior decision maker to determine whether to proceed immediately, proceed after a period without anticoagulants, or make alternative arrangements.
Review imaging
Ensure there is a recent chest x-ray or CT thorax which shows pleural effusion or pneumothorax and note which side.
For pneumothorax, assess the chest x-ray for a suitable location for the chest drain (generally the “triangle of safety” – see preparation).
For pleural effusion, make sure that you have an ultrasound operator who is competent in thoracic ultrasound (in the United Kingdom this would be someone with at least level 1 competency in thoracic ultrasound).
Introduction
Wash your hands using alcohol gel. If your hands are visibly soiled, wash them with soap and water.
Don PPE if appropriate.
Introduce yourself to the patient including your name and role.
Confirm the patient’s name and date of birth.
Briefly explain what the procedure will involve using patient-friendly language.
Example explanation
“We can see from the x-ray of your chest that there is a large amount of fluid/air in your lung cavity. To reinflate your lungs, we need to drain the air/fluid by inserting a tube into the chest, so that you can breathe easier.”
“We do this by first inserting a needle between two of your ribs, then replacing this with a plastic tube. We use a local anaesthetic to reduce the discomfort of the procedure and can also prescribe painkillers. The drain usually stays in place for a day or two, but occasionally requires up to 1-2 weeks to fully drain the air/fluid.”
“There are always risks when we perform an invasive procedure like this, but we believe that the benefits outweigh the risks. The most common potential complications include bleeding, pain, infection, air or blood being introduced into the lung cavity, damage to the nearby organs, and failure of the procedure.”
Gain written consent to proceed with chest drain insertion.
Check if the patient has any allergies (e.g. latex, local anaesthetic).
Ask the patient if they have any pain before continuing with the clinical procedure.
Preparation
Positioning
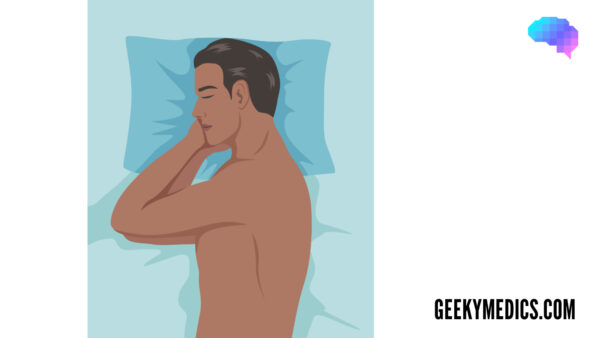
There are three common patient positions for chest drain insertion, depending on the planned area of insertion and the mobility and comfort of the patient:
- Patient lying on their back, semi-reclined, with their hand on the side of insertion behind their head.
- Patient sitting upright and leaning forwards on the edge of their bed, with their bedside table locked in front of them, with two pillows for the patient to rest their arms on.
- Patient lying on their side, with their head on a pillow and both of their hands underneath their head.
Identify the chest drain insertion site
For pneumothorax, ultrasound is not usually required, and you should insert the drain in the triangle of safety if the x-ray confirms it is safe to do so.
For pleural effusions, ask the ultrasound operator to perform an initial scan. The operator should assess the side with the effusion and mark or make note of the best place to aspirate. Ideally, this should be within the triangle of safety.
A simple way to mark the area is to push a pen lid into the skin, twisting while trying to avoid causing the patient discomfort. This marking will still be visible after cleaning the skin.
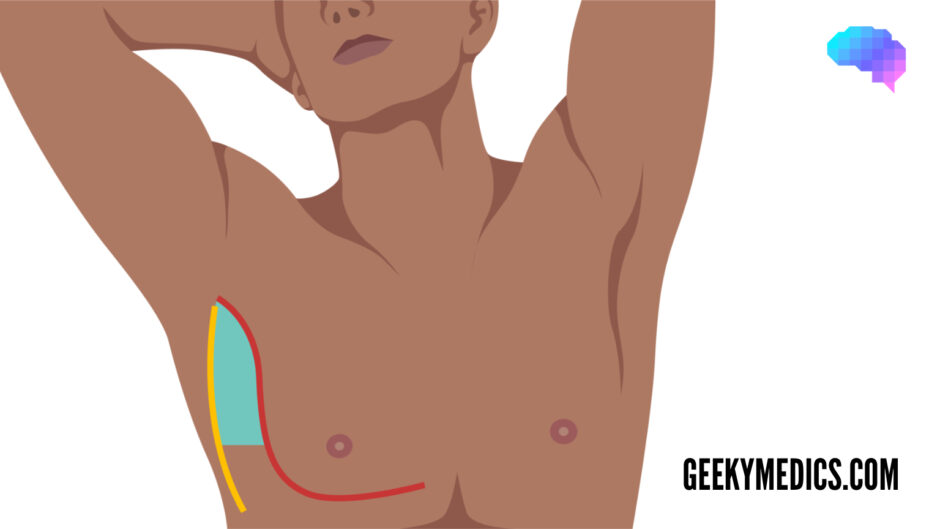
The triangle of safety
The triangle of safety is an area of the axilla with the lowest rate of complications when performing an invasive pleural procedure such as a pleural tap or chest drain.
Needles inserted outside of this area have a higher chance of perforating the lung, pericardium, heart, and liver, and thus must be performed after careful review of imaging and/or under ultrasound guidance (for effusions).
The triangle of safety is bordered by three anatomical landmarks:
- Pectoralis major
- Latissimus dorsi
- 5th intercostal space (roughly at the level of the nipple)
Set up the sterile field
1. Wash your hands and don an apron.
2. Remove the outer packaging from the sterile field.
3. Place the sterile field on the clean top shelf of the trolley, opening the pack from the corners without touching the inner surface of the field.
4. Use an aseptic non-touch technique (ANTT) to place the chest drain kit, antiseptic solution, sterile drapes, needles, syringe, sterile ultrasound probe cover (for effusions), sterile gauze, suture, and sterile dressing onto the sterile field.
5. Pour sterile water into the chest drain bottle up to the marking.
6. Wash your hands again.
7. Don sterile gloves and clean a ~20cm area of the patient’s skin around the site of insertion.
8. Apply sterile drapes to the patient, ensuring that only the cleaned area is visible.
9. Check the expiry date of the local anaesthetic and ask your ultrasound operator, or an assistant, to open the vial. Use a needle and syringe to draw this up without sterile equipment touching a non-sterile surface.
10. For pleural effusions: place your hand inside the sterile ultrasound probe sheath so that you can grab the probe from your operator, holding onto it as you allow the rest of the sheath to cover the probe wire. Place the elastic bands supplied with the sheath underneath the probe to prevent and hand it to your ultrasound operator, who should now also be wearing sterile gloves.
Infiltrate local anaesthetic
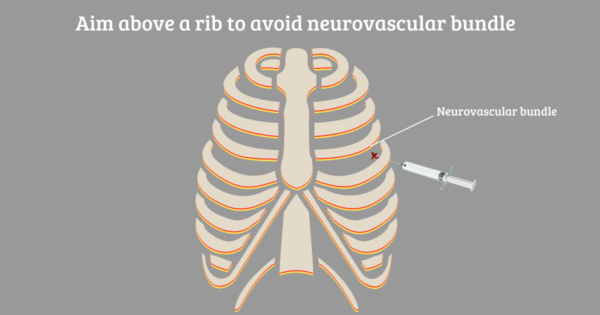
1. Check the skin mark and feel the area to make sure that you are inserting the needle above a rib, to avoid causing damage to the neurovascular bundle.
2. For pleural effusions: at this stage, your ultrasound operator can re-check the needle insertion site to ensure the fluid has not shifted.
3. Insert the 23-25G needle with local anaesthetic into the skin at a shallow angle (~15 degrees). As you inject between the dermis and epidermis you should see a small, raised area called a “dermal bleb”.
4. Leave this to take effect for 30 seconds.
5. Using the 21G (green) needle, infiltrate the intercostal muscles with the remaining local anaesthetic, making sure to aspirate before you inject to check that you are not in a blood vessel.
6. After anaesthetising, check that the positioning is correct by slowly inserting the green needle while aspirating, stopping when air or fluid starts to fill the syringe. If you are unable to aspirate pleural contents, do not proceed with drain insertion.
Insert the chest drain
1. Attach the introducer needle from the chest drain kit to a 10ml syringe.
2. Using the same tract from which you just successfully aspirated, advance the introducer needle while aspirating, stopping 0.5cm after air or fluid first starts to fill the syringe. Tip: the bevel of the needle should face upwards for pneumothorax and downwards for effusion, making it easier to direct the guidewire (and therefore the drain) upwards to drain air, and downwards to drain fluid.
3. Take note of the depth of the needle when it enters the pleural space.
4. Remove the syringe, and quickly place your thumb over the open end of the needle hub.
5. Gently pass the Seldinger guidewire down the hub of the needle, directing upwards for pneumothorax, and downwards for effusion. Ensure plenty of guidewire has entered the pleural cavity.
6. Gently remove the needle, keeping hold of the guidewire.
7. Make a small skin incision with a scalpel at the insertion site, pointing the sharp edge away from the wire. Tip: from this point, until the guidewire is removed, you need to make sure that you are always holding the guidewire. Hold it next to the skin when the dilator is out, and at the end of the dilator or drain when inserting them. Failure to do so could result in serious complications.
8. Warn the patient that they may experience a pushing and pulling sensation.
9. Pass the dilator over the guidewire, twisting gently when you reach the skin, until the dilator has passed 1cm beyond the depth at which the needle began to aspirate pleural contents (which you noted in step 3).
10. Remove the dilator. If you are using a >12F drain, you may have a larger dilator to insert to dilate the tract further.
11. Pass the drain over the guidewire and through the skin to a depth of 5-10cm, ensuring that the last drainage hole is well within the pleural space.
12. Remove the wire and hold your thumb over the end of the drain.
13. Attach the three-way tap from the chest drain kit to the end of the drain.
14. Using a syringe, aspirate from the three-way tap to ensure the drain is working, then close the three-way tap.
Securing and connecting the drain
1. Insert the straight needle suture into the skin next to the drain at a shallow angle, coming out of the skin after around 1cm.
2. Cut the needle off the suture and wrap the suture around the chest drain 2-3 times, tying this off tightly to ensure the drain stays in place during patient movement.
3. Apply a transparent dressing over the drain so that the insertion site is visible.
4. Attach the drain to the chest drain bottle tubing.
5. Open the three-way tap so that the air or fluid is draining freely. The fluid level should “swing” with respiration.
To complete the procedure…
Explain to the patient that the procedure is now complete.
Thank the patient for their time.
Dispose of PPE and other clinical waste into an appropriate clinical waste bin.
Prescribe appropriate analgesia, prophylactic anticoagulation, and 6-8 hourly 30ml saline flushes.
Inform the patient that the underwater seal draining bottle must stay below the level of the chest drain insertion site.
Inform the nursing staff that you have inserted a chest drain, that it is on free drainage, and ask them to perform a set of vital signs.
If draining fluid from a large effusion, ensure no more than 1200-1500mL is drained in 24 hours to prevent re-expansion pulmonary oedema. This can be achieved by partially opening the 3-way tap so that fluid drains slowly, or by ensuring that no more than 400mL is drained every 8 hours.
Investigations
Request a post-procedure chest x-ray and check this yourself for drain position, ensuring this is performed within a few hours of the procedure.
If the patient has an effusion which requires diagnosis, decant the pleural fluid into separate containers depending on the required investigations:
- Biochemistry: LDH & protein: 2-5ml in a plain container or serum blood collection tube depending on local policy.
- Microbiology: fluid culture & sensitivities: 5ml in a plain container. If a pleural infection is likely, send 5ml in both blood culture bottles also.
- Cytology: cytological examination and differential cell count: aim for 30ml in a plain container to assess for malignant cells.
Documentation
Place the consent form in the patient’s notes.
Document details of the procedure in the patient’s notes including:
- Your personal details including your name, job role and GMC number
- The date and time the procedure was performed
- That you have gained written consent
- The indication for chest drain
- The length of the chest drain inserted
- Type of suture used
- Colour of the fluid drained
- Instructions on when to open and close the three-way tap
- Any complications
- What investigations have been requested, and who is responsible for checking the results
Reviewer
Dr Praveen Bhatia
Respiratory Consultant
Editor
Dr Chris Jefferies
References
- British Thoracic Society. BTS Clinical Statement on Pleural Procedures. June 2022. Available from: [LINK]
- British Thoracic Society. BTS Guideline for Pleural Disease. June 2022. Available from: [LINK]
- Thorax. Pleural procedures and thoracic ultrasound: British Thoracic Society pleural disease guideline 2010. August 2010. Available from: [LINK]
- MedCourse. Aim above a rib to avoid the neurovascular bundle. Licence: [CC BY-SA].