- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Coronavirus disease 2019 (COVID-19) is a contagious respiratory disease, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).1
In the year since the first case of COVID-19 was reported, there were over 82 million COVID-19 cases and over 1.8 million deaths worldwide.2
Aetiology
SARS-CoV-2 is primarily transmitted through respiratory air droplets, which are expelled when an infected person talks, coughs and sneezes.3
SARS-CoV-2 can also be transmitted through saliva and by touching contaminated surfaces, although it significantly decays on surfaces within 72 hours.4
The virus has been detected in other bodily fluids, but not at adequate viral loads to be considered infectious.5
The mean incubation time (time from exposure to symptom onset) is five days, but it can be as long as 14 days.6
Infectivity begins one to three days before symptom onset and can last for 10 days in mild-moderate cases, and even longer in severe cases.7 There are several variants of SARS-CoV-2, and more variants continue to be discovered. Some variants are more infectious than others.8
Pathophysiology
SARS-CoV-2 enters nasal epithelial cells via the ACE-2 receptor and then migrates to the upper respiratory tract. This triggers an immune response, including the release of interferons (IFN-β and IFN-γ) from infected cells.9
In most patients, the immune response halts the spread of the virus at the upper respiratory tract, and so most patients only develop mild symptoms. However, in approximately 20% of patients, the virus progresses to the lower respiratory tract.10
Infected pneumocytes release inflammatory cytokines (such as IL-6 and IL-8), which attract immune cells to the lungs (including T helper cells).11
The exaggerated immune response to SARS-CoV-2 results in diffuse alveolar damage and pulmonary oedema (in keeping with acute respiratory distress syndrome).12
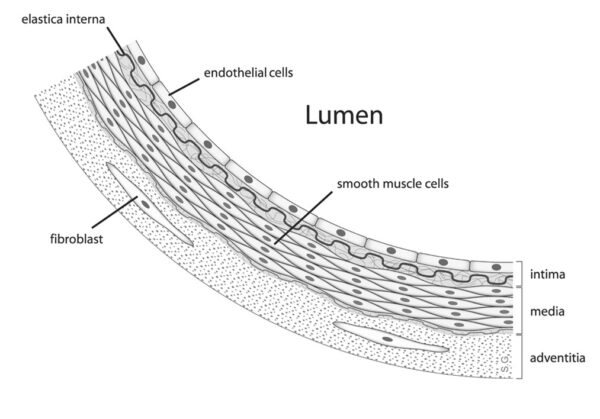
SARS-CoV-2 also causes damage to endothelial cells, which are found in the inner layer of blood vessels (Figure 1). Endothelial dysfunction results in a procoagulant state, leading to thrombotic complications (such as pulmonary embolism and microvascular thrombi in the lungs).13
There is emerging evidence that SARS-CoV-2 can affect other organs (such as the brain and gastrointestinal tract), potentially through its ability to disrupt endothelial surfaces and incite exaggerated immune responses.14-15 This can cause symptoms which persist months after the acute infection (often referred to as “Long COVID”).
Risk factors
The following risk factors are associated with an increased risk of contracting COVID-19:
- Close contact with an infected person (within one metre for at least 15 minutes)
- Old age
- Residence or employment in an area with increased transmission (such as healthcare settings or care homes)
The following risk factors are associated with an increased risk of developing severe COVID-19 infection:
- Male sex
- Asian and Afro-Caribbean ethnicity17
- Medical comorbidities (including chronic respiratory disease, type 2 diabetes and heart failure)
- Current or former smokers
Clinical features
History
Typical symptoms of COVID-19 include:
- Fever
- New and continuous cough (typically described as dry, but may be productive)
- Altered sense of smell and taste
- Dyspnoea (initially on exertion, but may progress to resting dyspnoea)
- Non-specific symptoms (fatigue, myalgia and pharyngitis)
- Delirium and reduced mobility in the elderly
Other important areas to cover in the history include:
- Recent contact with suspected or confirmed COVID-19 cases
- Smoking history: quantify in pack-years (1 pack-year = smoking 20 cigarettes a day for a year)
- Travel history: the patient may have travelled from an endemic area
Clinical examination
A full respiratory examination should be performed in suspected cases of COVID-19.
Typical clinical findings in COVID-19 include:
- Tachypnoea and tachycardia
- Crepitations and bronchial breathing on auscultation
- Cutaneous manifestations: such as maculopapular rash, urticaria and petechial rash (Figure 2)

Differential diagnoses
Differential diagnoses to consider in the context of suspected COVID-19 include:
- Community-acquired bacterial pneumonia
- Influenza infection
- Common cold
- Middle East Respiratory Syndrome (MERS)
- Aspiration pneumonia
Investigations
Bedside investigations
Relevant bedside investigations include:
- COVID-19 nasopharyngeal and/or oropharyngeal swab: the swab is used to sample the respiratory mucosa. The sample is analysed using real-time reverse-transcription polymerase chain reaction (RT-PCR). A positive result indicates the presence of SARS-CoV-2 viral RNA.
- Pulse oximetry: aim for 94-98% initially, but the target saturations may be reduced to 88-92% if the patient has COPD (this is a risk-benefit judgement made by a senior clinician).
- Sputum culture: to exclude other causes of lower respiratory tract infection, including bacterial causes.
- Arterial blood gas: recommended in patients with low oxygen saturations or signs of respiratory distress. May show type 1 or type 2 respiratory failure. May also show elevated lactate, which indicates tissue hypoxia and organ dysfunction.
Laboratory investigations
Relevant laboratory investigations include:
- Full blood count: may show leucocytosis and lymphopenia
- CRP: may be elevated
- U&Es: may be elevated and indicate acute kidney injury
- LFTs: may be elevated (associated with severe disease)
- Coagulation screen: may show elevated D-dimer and prolonged prothrombin time (both associated with severe disease).19
Imaging
Chest X-ray
A chest X-ray may reveal bilateral ground-glass opacifications and consolidation.
Ground-glass opacifications refer to areas of hazy opacification which do not completely obscure the underlying pulmonary vasculature or bronchial structures.20
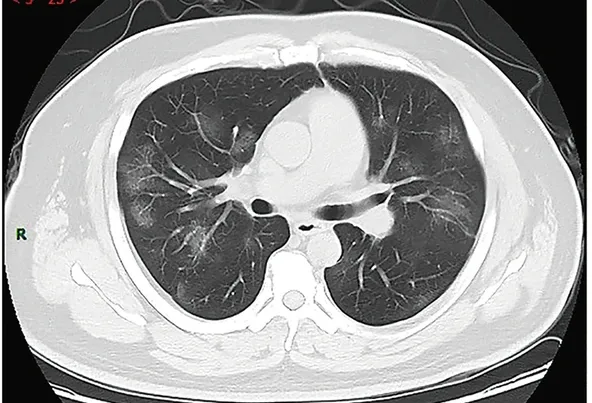
CT chest
National guidelines recommend CT chest for patients with severe disease when chest X-ray is unclear or normal (though local guidelines may vary).21
Common CT chest findings include bilateral ground-glass changes, fine reticulations (linear opacifications) and peribronchovascular thickening (thickening of the connective tissue that encloses the bronchi and pulmonary arteries).22
Management
Conservative management
Conservative management of COVID-19 includes:
- Self-isolation: at the time of writing, all COVID-19 cases and their close contacts must self-isolate for 10 days. Self-isolation should continue after 10 days if the patient still has a fever, rhinorrhoea, malaise or diarrhoea.25
- Symptom management: such as honey to reduce cough frequency, and discouraging patients from lying on their back as this reduces cough efficiency.
- Adequate hydration and nutrition.
Medical management
Medical management of COVID-19 includes:
- Oxygen therapy: to maintain target saturations 94-98% (or 88-92% if the patient has COPD)
- Antipyretics: such as paracetamol
- Dexamethasone: used in severe disease (such as oxygen saturations <90% on room air, sepsis or ARDS). The dose is 6mg once daily for 7-10 days.26-27
- Remdesivir: this antiviral may be used in severe disease (this is a senior-led decision). Remdesivir is usually given as a loading dose of 200mg IV on day 1, followed by 100mg IV for 5-10 days.28,29
- Empirical antibiotics: only recommended if bacterial co-infection is suspected. Signs of bacterial co-infection include a change in symptoms (such as new pyrexia), new neutrophilia and radiological findings suggestive of bacterial pneumonia.30
- Venous thromboembolism prophylaxis: used in hospitalised patients as COVID-19 increases the risk of venous thromboembolism. Low-molecular-weight heparins are commonly used (such as enoxaparin).
Ventilation
Options for ventilatory support in COVID-19 include:
- Continuous positive airway pressure (CPAP): may be used in type 1 respiratory failure (PaO2 < 8kPa/ 60mmHg).31
- Non-invasive ventilation (NIV): may be used in type 2 respiratory failure (PaO2 < 8kPa / 60mmHg and PaCO2 > 6.0kPa / 45mmHg).
- Mechanical ventilation: may be needed if the patient continues to deteriorate despite optimal use of CPAP or NIV.
- Extracorporeal membrane oxygenation (ECMO): may be needed if the patient continues to deteriorate despite mechanical ventilation and if the patient has potentially reversible respiratory failure. ECMO involves diverting the patient’s blood to an artificial oxygenator, where oxygen is added and carbon dioxide is removed from the blood. The blood is then pumped back into the patient’s circulatory system (Figure 5). The decision to start ECMO is senior-led, and ECMO is only performed in specialist centres.

Complications
Disease-related complications
Disease-related complications include:
- Venous thromboembolism (e.g. pulmonary embolism)
- Acute kidney injury
- Septic shock
- Cardiovascular complications (e.g. acute coronary syndrome and myocarditis)
- “Long COVID”: approximately 10% of COVID-19 patients display symptoms for 12 weeks or more after the initial infection.33 These symptoms include persistent cough, lethargy and myalgia.34
Treatment-related complications
Treatment-related complications include:
- Dexamethasone: hyperglycaemia and confusion
- Mechanical ventilation: ventilator-associated lung injury (VALI), ventilator-associated pneumonia (VAP) and laryngeal injury
Key points
- Coronavirus disease 2019 (COVID-19) is a contagious respiratory disease, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
- COVID-19 is primarily transmitted through respiratory air droplets. Close contact with an infected person increases the risk of developing COVID-19.
- The most common symptoms are continuous cough, fever and an altered sense of smell or taste.
- A diagnosis of COVID-19 is based on clinical findings, detection of SARS-CoV-2 viral RNA using RT-PCR and radiological findings.
- Characteristic chest X-ray findings include bilateral ground-glass opacifications and consolidation.
- Management includes self-isolation and supportive measures in mild cases. Dexamethasone and ventilatory support may be needed in severe cases.
- Complications include venous thromboembolism, septic shock and “Long COVID”.
Feedback
Please click here to fill out the feedback form, which should take less than 1 minute of your time. Feedback is vital as it allows authors to improve their articles, leading to even better content on Geeky Medics!
Reviewer
Dr Bhamini Puvaneswaran
Infectious Disease and Medical Microbiology Specialist Registrar
Editor
Dr Chris Jefferies
References
- Gorbalenya AE et al. The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nature Microbiology. Published in 2020. Available from: [LINK]
- Center for Systems Science and Engineering, Johns Hopkins University. COVID-19 Dashboard. Published in 2020. Available from: [LINK]
- Wiersinga J et al. Pathophysiology, Transmission, Diagnosis and Treatment of Coronavirus Disease 2019 (COVID-19). JAMA. Published in 2020. Available from: [LINK]
- van Doremalen N et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. New England Journal of Medicine. Published in 2020. Available from: [LINK]
- BMJ Best Practice. Coronavirus disease 2019 (COVID-19). Published in 2020. Available from: [LINK]
- McAloon C et al. Incubation period of COVID-19: a rapid systematic review and meta-analysis of observational research. Published in 2020. Available from: [LINK]
- World Health Organization. Transmission of SARS-CoV-2: implications for infection prevention precautions. Published in 2020. Available from: [LINK]
- Public Health England. Investigation of novel SARS-CoV-2 variant. Published in 2021. Available from: [LINK]
- Parasher A. COVID-19: Current understanding of its pathophysiology, clinical presentation and treatment. Postgraduate Medical Journal. Published in 2020. Available from: [LINK]
- Kumar R et al. Pathophysiology and potential future therapeutic targets using preclinical models of COVID-19. ERJ Open Research. Published in 2020. Available from: [LINK]
- Blanco-Melo D et al. Imbalanced Host Response to SARS-CoV-2 Drives Development of COVID-19. Cell. Published in 2020. Available from: [LINK]
- Polak SB et al. A systematic review of pathological findings in COVID-19: a pathophysiological timeline and possible mechanisms of disease progression. Modern Pathology. Published in 2020. Available from: [LINK]
- Jin Y et al. Endothelial activation and dysfunction in COVID-19: from basic mechanisms to potential therapeutic approaches. Signal Transduction and Targeted Therapy. Published in 2020. Available from: [LINK]
- Dennis A et al. Multi-organ impairment in low risk individuals with long COVID. MedRxiv. Published in 2020. Available from: [LINK]
- Ma C et al. COVID-19 and the Digestive System. The American Journal of Gastroenterology. Published in 2020. Available from: [LINK]
- Rosenbach D. Endothelium. License: [CC BY-SA]. Available from: [LINK]
- Sze S et al. Ethnicity and clinical outcomes in COVID-19: a systematic review and meta-analysis. Published in 2020. Available from: [LINK]
- Tn FO. Petechial rash. License: [CC BY-SA]. Available from: [LINK]
- Danwang C et al. A meta-analysis of potential biomarkers associated with severity of coronavirus disease (COVID-19). Biomarker Research. Published in 2020. Available from: [LINK]
- Kobayashi Y et al. Management of ground-glass opacities: should all pulmonary lesions with ground-glass opacity be surgically resected? Translational Lung Cancer Research. Published in 2013. Available from: [LINK]
- British Society of Thoracic Imaging. Radiology decision tool for suspected COVID-19. Published in 2020. Available from: [LINK]
- Jalaber C et al. Chest CT in COVID-19 pneumonia: a review of the current knowledge. Diagnostic and Interventional Imaging. Published in 2020. Available from: [LINK]
- Hellerhoff. COVID-19 Chest X-Ray. License: [CC BY-SA]. Available from: [LINK]
- Jin Y et al. COVID-19 CT Chest. License: [CC BY-SA]. Available from: [LINK]
- Public Health England. Stay at home: guidance for households with possible or confirmed coronavirus (COVID-19) infection. Published in 2020. Available from: [LINK]
- Horby et al. Dexamethasone in Hospitalised Patients with COVID-19 – Preliminary Report. New England Journal of Medicine. Published in 2020. Available from: [LINK]
- National Institute for Health and Care Excellence. COVID-19 prescribing briefing: corticosteroids. Published in 2020. Available from: [LINK]
- Beigel JH et al. Remdesivir for the Treatment of COVID-19 – Final Report. New England Journal of Medicine. Published in 2020. Available from: [LINK]
- British National Formulary. Remdesivir. Published in 2020. Available from: [LINK]
- Wu CP et al. Recognition and management of respiratory co-infection and secondary bacterial pneumonia in patients with COVID-19. Cleveland Clinic Journal of Medicine. Published in 2020. Available from: [LINK]
- Nicholson TW et al. Respiratory failure and non-invasive respiratory support during the COVID-19 pandemic: an update for re-deployed hospital doctors and primary care physicians. BMJ. Published in 2020. Available from: [LINK]
- Meurs V et al. ECMO. License: [CC-BY]. Available from: [LINK]
- Office for National Statistics. The prevalence of long COVID symptoms and COVID-19 complications. Published in 2020. Available from: [LINK]
- Nabavi N. Long COVID: How to define it and how to manage it. BMJ. Published in 2020. Available from: [LINK]