- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
This death confirmation OSCE guide provides a step-by-step approach to confirming death in an OSCE setting, with an included video demonstration.
Background
According to the Academy of Medical Royal Colleges (AoMRC), death is the irreversible loss of essential characteristics which are necessary to the existence of a living human person.
Therefore, the definition of death should be regarded as the irreversible loss of the capacity for consciousness combined with the irreversible loss of the capacity to breathe. Death may be secondary to a wide range of underlying problems in the body.1
This means that whilst the end point of death is always within the brain, it can be diagnosed using circulatory, neurological or somatic criteria to identify situations that will lead to the irreversible loss of the capacity for consciousness and the irreversible loss of the capacity to breathe.
Confirming death (also called verifying death) is a core skill for medical practitioners in the UK, and this is most commonly undertaken using the circulatory criteria approach described below.2
Before death confirmation
Before confirming death, ensure that one of the following criteria has been fulfilled:
- The patient meets the criteria for not attempting cardiopulmonary resuscitation (e.g. the patient has a Do Not Attempt Cardiopulmonary Resuscitation (DNACPR) form)
- Attempts at CPR have failed
- Treatment aimed at sustaining life has been withdrawn as it has been decided that it would be to no further benefit to the patient
If family or friends of the patient are present, introduce yourself and offer your condolences. Explain the need to confirm death and offer the family the opportunity to leave or stay during the confirmation of death process.
Death confirmation
To perform death confirmation:
1. Wash your hands and don PPE if appropriate.
2. Check the identity of the patient with the ward/nursing staff, and ensure this matches the identity of the patient by checking their wristband.
3. Assess the patient’s response to verbal stimuli e.g. “Hello, Mr Smith, can you hear me?” (response to verbal stimuli is not part of the formal process but is good practice as a first approach to the patient)
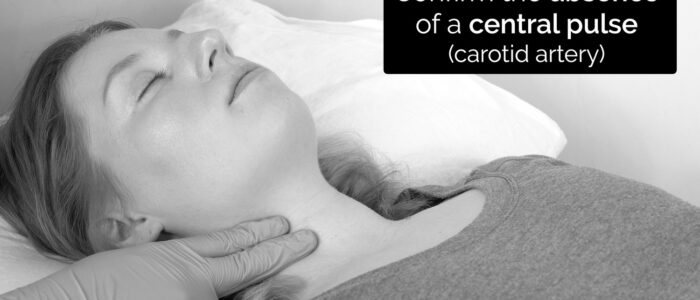
4. For a minimum of five minutes, confirm the absence of:
- Central pulse on palpation (carotid artery)
- Heart sounds on auscultation
- Respiratory sounds on auscultation
- Signs of life (e.g. movement and respiratory effort)
In a hospital setting, if appropriate equipment is available, this can be supplemented with one or more of the following:
- Asystole on continuous ECG monitoring
- Absence of pulsatile flow using direct intra-arterial pressure monitoring
- Absence of contractile activity using echocardiography
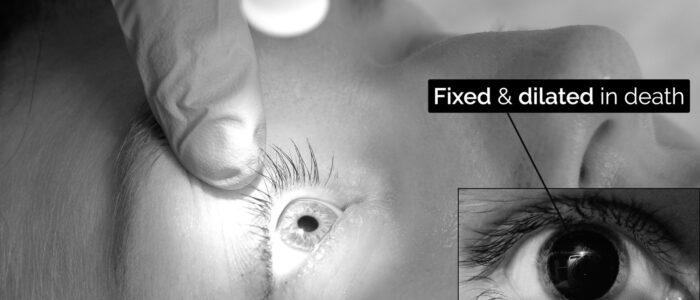
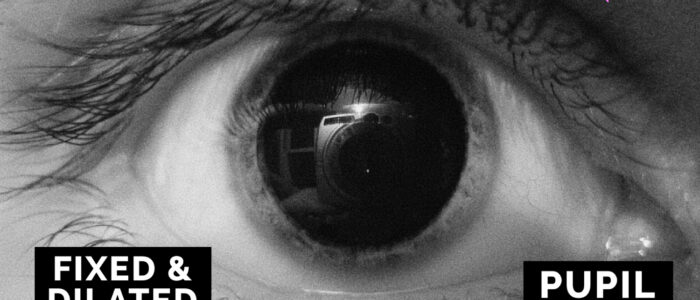
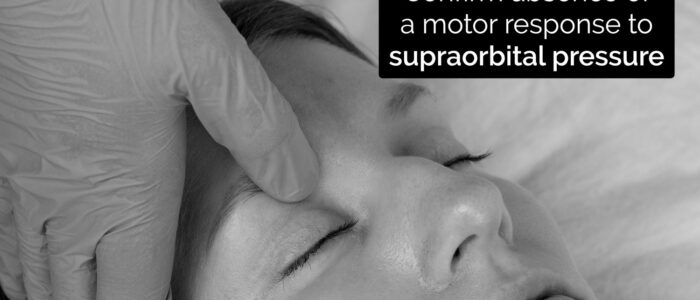
5. After five minutes of cardiorespiratory arrest, confirm:
- Bilateral absence of pupillary reflexes using a pen torch (after death, the pupils become fixed and dilated)
- Bilateral absence of corneal reflexes using a piece of cotton/paper
- The absence of any motor response to supraorbital pressure
6. The time of death should be recorded as the time at which all these criteria have been confirmed.
Corneal reflex
The corneal reflex involves the involuntary blinking of both eyelids in response to unilateral corneal stimulation (direct and consensual blinking). The afferent branch of the corneal reflex involves V1 of the trigeminal nerve whereas the efferent branch is mediated by the temporal and zygomatic branches of the facial nerve.
To assess the corneal reflex:
1. Gently touch the edge of the cornea using a wisp of cotton wool.
2. The absence of a blinking response would be expected in the context of death.
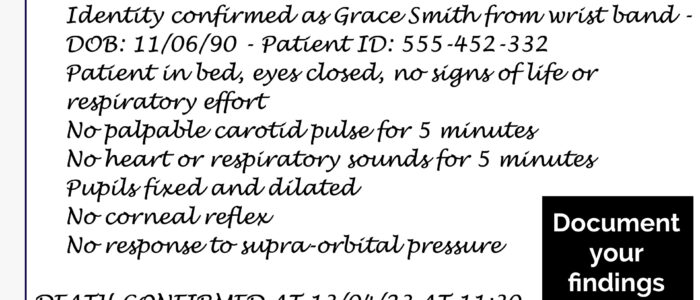
Documentation
Once you have completed the required steps to confirm the death, you must document your assessment.
Document each of the steps you performed and the result of each step. Then document that death has been confirmed, including the time at which this occurred.
Your hospital may require you to propose a medical cause of death in the notes for review by the medical examiner.
Sign and print your full name, grade, registration number and contact number.
Read our guide to documenting death confirmation for more details.
To complete death confirmation…
Inform the relevant nursing staff that you have confirmed the death. If not already present, you or the nursing staff should inform the next of kin.
Consider if the death may need referring to the coroner. If this is the case, a death certificate should not be issued, and you should discuss the situation with the consultant responsible for the patient and the medical examiner.
To learn more about completing a death certification, read our guide.
Reviewer
Dr Steven Gill
Consultant in Intensive Care Medicine and Anaesthesia
Clinical Lead for Organ Donation (Education)
Nottingham University Hospitals
References
- Academy of Medical Royal Colleges. Code of Practice for the Diagnosis and Confirmation of Death. Published in 2008. Available from: [LINK].
- Treatment and care towards the end of life: good practice in decision making. General Medical Council 2010. Available from: [LINK]
- OpenStax College. Mydriasis Image. Licence: CC BY 3.0