- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
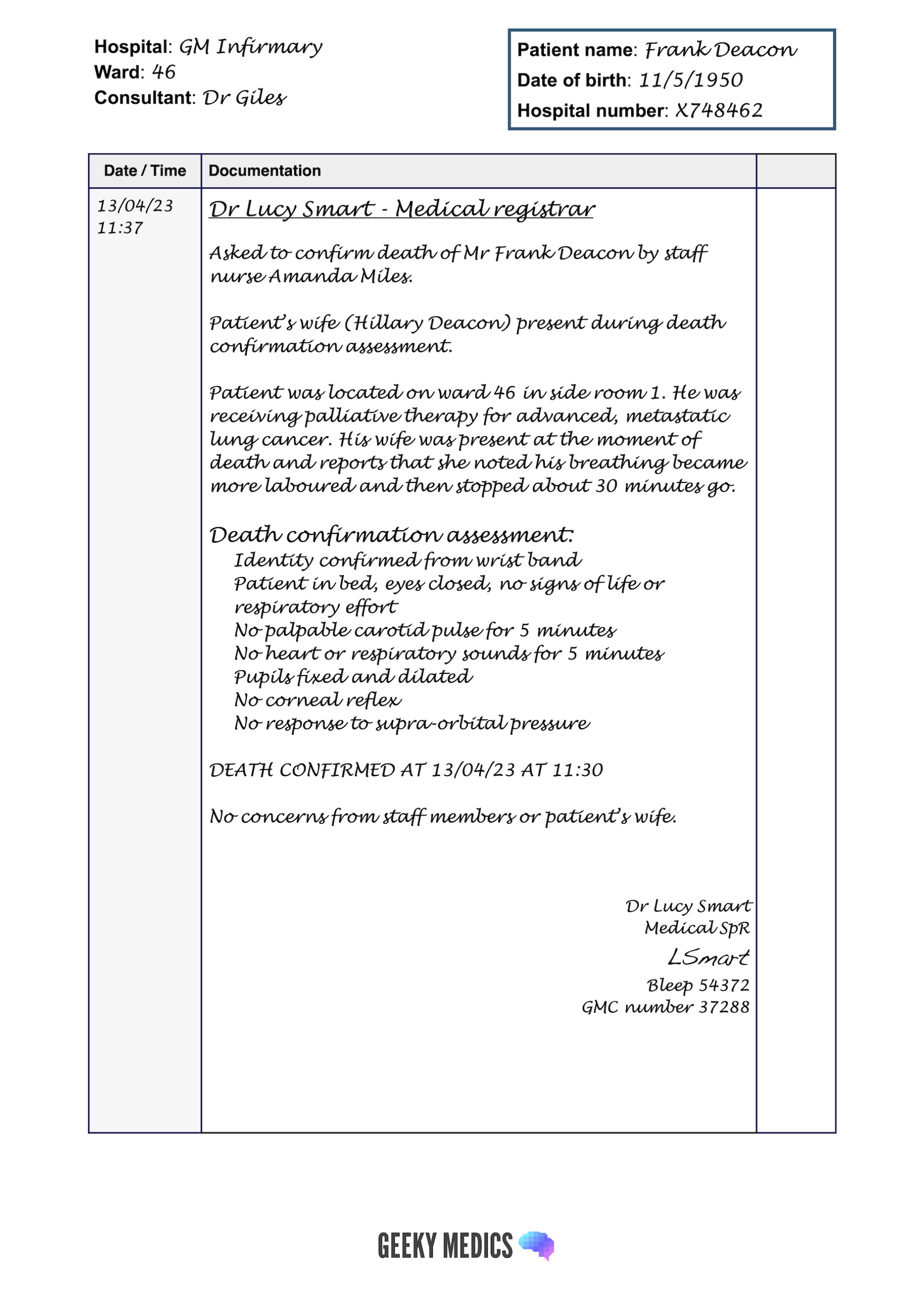
In addition to knowing how to perform death confirmation, it’s important to document the process accurately in the medical notes.
This guide provides a structured approach to documenting death confirmation in a patient’s notes. For more information on completing a death certificate, see our guide to certification of death.
Documentation basics
Before we discuss how to document the death confirmation, we need to cover the basics that apply to all documentation in a patient’s notes. You can check out our detailed guide to writing in the notes for more information.
What should I use to write with?
You need to use a pen with black ink, as this is the most legible if notes are photocopied.
Patient details
For every new sheet of paper, your first task should be to document at least three key identifiers for the relevant patient:
- Full name
- Date of birth
- Unique patient identifier
- Home address
If a patient label containing at least three identifiers is available, this can be used instead of manually writing out the information.
Location details
You should indicate the patient’s current location on the continuation sheet:
- Hospital
- Ward
Starting your entry in the notes
At this point, you should already be holding a pen with black ink, and you should have ensured the continuation sheet has at least three key patient identifiers at the top.
The next documentation steps include:
1. Adding the date and time (in 24-hour format) of your entry.
2. Writing your name and role as an underlined heading.
3. Adding your entry in the notes below this heading (see the next section for details).
Documenting death confirmation in the notes
1. Document your reason for attending and, if relevant, who asked you to attend (e.g. asked to confirm the death of Mr Smith by staff nurse Amanda Miles).
2. Document who was present while you confirmed the death (e.g. staff members and/or the deceased patient’s family and friends).
3. Document the circumstances of the death:
- Location of the patient
- The individual who first noted the patient to be dead
- Any individual present at the moment of death
4. Document the confirmation of death assessment:
- Identity confirmed by wristband
- General inspection: no signs of life or respiratory effort
- No palpable central (carotid) pulse*
- No heart sounds on auscultation*
- No respiratory sounds on auscultation*
- Any other monitoring used to confirm cardiorespiratory arrest: continuous ECG monitoring, arterial line, echocardiography
- Absence of pupillary reflexes and corneal reflex
- Absence of motor response to supra-orbital pressure
* The patient must be observed for at least five minutes to confirm cardiorespiratory arrest. It is important to document this.
5. Document the outcome of the assessment, including the time of death (which should be documented as the time at which you completed your assessment).
6. Document any discussions you had with staff members or relatives of the deceased concerning the death.
7. Document any concerns of staff members or the patient’s relatives.
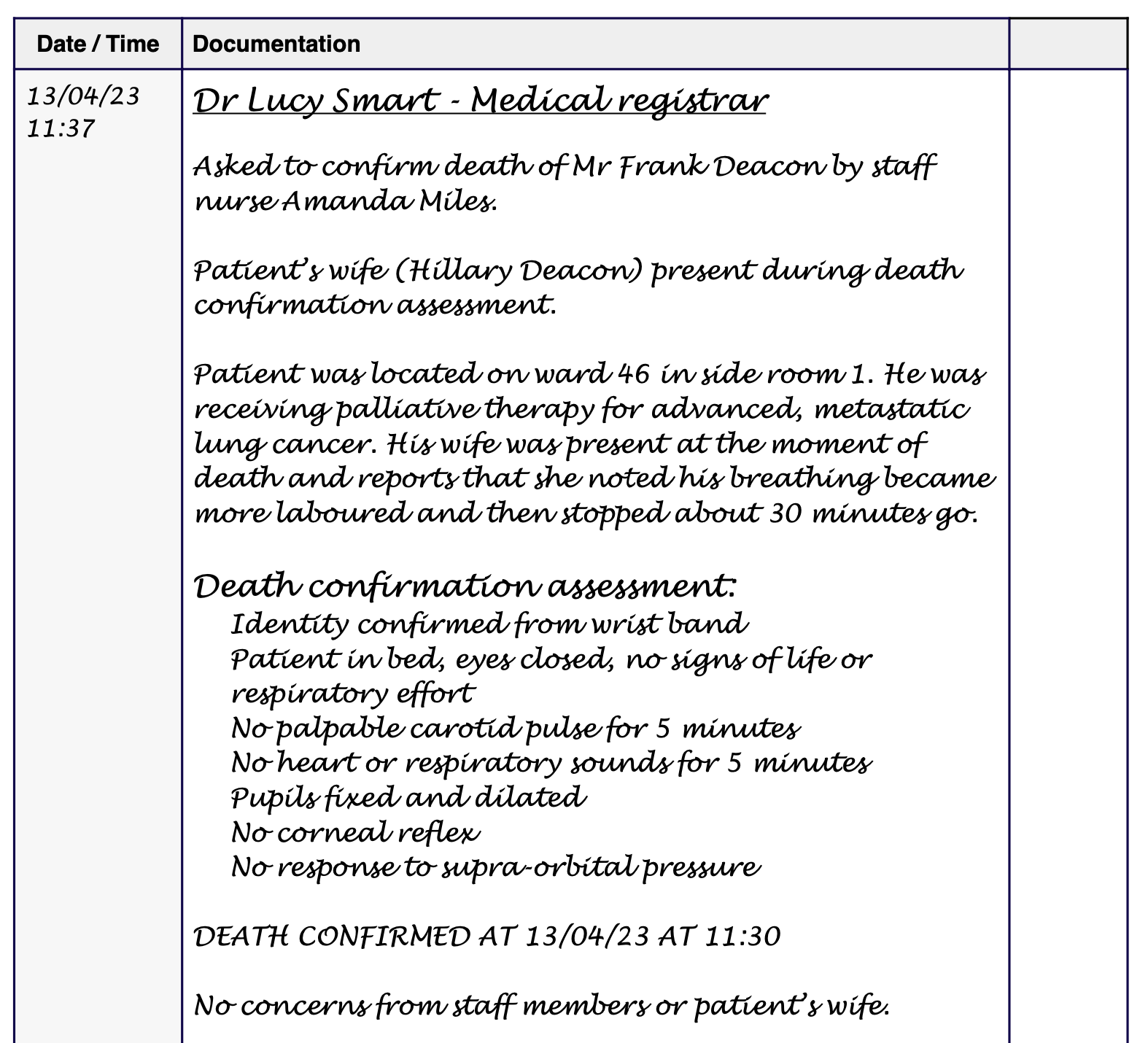
Completing the entry in the notes
At the end of your entry to need to include the following:
- Your full name
- Your grade/role (e.g. medical registrar, nurse practitioner)
- Your signature
- Your professional registration number (e.g. GMC number, NMC pin)
- Your contact number (e.g. phone/bleep)