- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Fractures of the distal radius are common upper limb injuries.1
Distal radius fractures are a common presentation to emergency departments and urgent care centres.
Many patients can be initially treated, and then discharged for orthopaedic follow up. However, it is important to identify patients with displaced fractures or neurovascular compromise who may require urgent orthopaedic intervention.2
Aetiology
Fractures of the distal radius are most common in two main groups of patients:3
- Young patients who participate in sport or are involved in trauma
- Elderly patients with osteoporosis and low energy trauma
The most common mechanism of injury is a fall onto an outstretched hand (FOOSH). If atraumatic, a pathological fracture should be suspected, and further workup should investigate for malignancy (e.g. blood tests including FBC, serum calcium, alkaline phosphatase and an isotope bone scan).
Types of distal radius fracture
There are three key fractures of the distal radius to be aware of:
- Colles’ fracture (most common): an extra-articular fracture with dorsal displacement (“dinner fork deformity”)
- Smith’s fracture: an extra-articular fracture with volar displacement
- Barton’s fracture: an intra-articular fracture with associated dislocation of the radiocarpal joint
Risk factors
Risk factors can be thought of in terms of those which increase the risk of osteoporosis and those which increase the risk of falling (Table 1).
Table 1. An overview of risk factors for fractures of the distal radius.
| Risk factors for osteoporosis | Risk factors for falling |
|
|
Clinical features
A thorough history and examination of the injury should be performed for patients who present with a suspected distal radius fracture.
The mechanism of injury and clinical findings, including skin integrity, assessment of circulation and sensation, should be documented at presentation.2
History
Typical symptoms of distal radius fractures include:
- Pain
- Swelling
- Loss of function
Other important areas to cover in the history include:
- Events surrounding the fall: features suggestive of syncope, other injuries (e.g. head injury), previous episodes
- Clinical features of neurovascular compromise (see below)
- Past medical history: risk factors for osteoporosis, previous fragility fractures, co-morbidities
- Family history: a family history of fragility fractures, especially parental hip fractures, is a risk factor for osteoporosis
- Social history: smoking and alcohol (risk factors for osteoporosis), occupation (may influence the choice of management)
For more information on falls, see the Geeky Medics guide to the assessment, investigation and management of falls.
Neurovascular injury
Although less common, it is important to ask about symptoms which may suggest neurovascular injury including the 3P’s:
- Paraesthesia: tingling, pins and needles or loss of sensation in the hand (suggesting nerve injury)
- Pain: disproportionate to the injury (suggesting compartment syndrome)
- Pallor: pallor or duskiness of the hand (suggesting vascular injury)
Clinical examination
A thorough orthopaedic examination of the hand and wrist, along with a neurological examination of the upper limb should be performed to assess functional capacity and neurovascular deficits.
Typical clinical findings may include:
- Obvious deformity of the wrist
- Swelling and/or bruising at the wrist
- Tenderness on palpation of the distal radius
Less common clinical findings may include:
- Open wound and/or the bone protruding through the skin (open fractures require different management due to the risk of infection)
- Loss of sensation or movement distal to the fracture (suggesting nerve injury)
- Pulselessness and/or pallor of the hand (suggesting vascular compromise)
Neurological examination
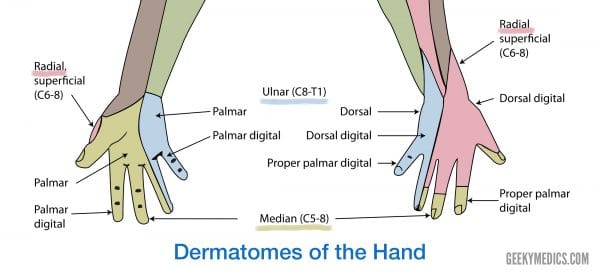
For suspected distal radius fractures, the neurological examination should also include assessment of the median, ulnar and radial nerves (Figure 1).
To assess the median nerve:
- Motor: grip strength and OK sign
- Sensory: the tip of the second digit (digital cutaneous branch) and thenar eminence (palmar cutaneous branch)
To assess the ulnar nerve:
- Motor: finger abduction/adduction
- Sensory: the tip of the little finger
To assess the radial nerve:
- Motor: finger and wrist extension
- Sensory: dorsal first webspace
Differential diagnoses
The clinical presentation of fractures of the distal radius is similar to several other fractures of the wrist:5
- Scaphoid fracture: commonly caused by a FOOSH as well. However, the main complaint is typically localised pain and tenderness over the anatomical snuffbox (triangular depression over lateral, dorsal hand).
- Ulnar styloid fracture: fracture of the ulnar styloid may be associated with distal radius fractures. It typically presents with local tenderness over the ulnar styloid.
- Fracture of the radial shaft: less common than distal radius fractures. The range of motion of the wrist is typically pain-free.
Investigations
Bedside investigations
Relevant bedside investigations include:
- Electrocardiogram (ECG): if there is suspicion of cardiac involvement in the fall
- Urine dipstick: if there is suspicion of a UTI causing confusion as a reason for the fall
- Blood sugar monitoring (BM): if there is suspicion of a hypoglycaemic episode as a reason for the fall
Laboratory investigations
Relevant laboratory investigations include:
- Baseline blood tests (FBC, U&E, LFTs)
- Bone profile if suspecting osteoporosis (vitamin D, serum calcium, ALP)
Imaging
Relevant imaging investigations include:6
- X-rays: AP and lateral views of the wrist (Figure 2)
- CT: may be required if suspected intra-articular involvement or for pre-operative planning
- MRI: may be required if suspected soft tissue injuries

Osteoporosis assessment
A wrist fracture is the most common fragility fracture in perimenopausal and young postmenopausal women.1
If the fracture is thought to be a fragility fracture due to osteoporosis, the FRAX® risk assessment tool should be used to assess whether osteoporosis treatment should be started (bisphosphonates) or if a DEXA scan (dual-energy x-ray absorptiometry) is indicated.8
Management
According to the British Orthopaedic Associations’ standards for practice, the aim of treatment is to optimise functional recovery rather than achieving specific radiological parameters.9
Management of distal radius fractures can be structured according to their immediate management (usually done in the emergency department) followed by the definitive management (usually decided upon by the orthopaedic team in the fracture clinic).
Immediate management
Regardless of the specific type of fracture, the immediate management remains the same:9
- ABCDE assessment
- Analgesia
- Assessment of skin integrity and neurovascular status: capillary refill time, movements and sensations in the hand
- Removal of any rings or jewellery on the affected hand
- Reduction of displaced fractures: under intravenous regional anaesthesia (IVRA) or haematoma block, followed by repeat X-ray
- Immediate immobilisation (e.g. back slab cast)
- Elevation
All patients should be referred to the fracture clinic service and assessed within 72 hours.9
Definitive management6,9
Table 2. Overview of definitive management strategies for types of wrist fractures
| Type of fracture | Definitive management |
| Stable, undisplaced fracture |
If patients are unable to tolerate cast, or in those with an incomplete fracture, a forearm splint holding the wrist in neutral can be used. |
| Colle’s fracture (dorsal displacement) |
For patients with simple fracture patterns and/or poor co-morbid status:
For patients with complex fracture patterns and good co-morbid status:
|
| Smith’s fracture (volar displacement) |
Any volar displacement is always unstable and will, therefore, need surgical fixation (unless surgery is unsuitable due to co-morbidities):
|
| Barton’s fracture |
The chance of successful reduction is low, therefore ORIF is usually required. If it is a volar Barton’s fracture, these (like Smith’s) are always unstable and require surgical fixation |
Follow-up
All patients should receive information regarding expected functional recovery and rehabilitation, including advice about the return to normal activities such as work, education and driving.
Patients should be able to self-refer to the fracture service if progress is not as anticipated and hospitals should provide this mechanism.9
Rehabilitation6
Whether the patient is being treated in a cast or splint or is awaiting surgical fixation, it is critical to have them begin rehabilitation of the hand at the earliest opportunity. Rehabilitation includes:
- Elevation of the limb
- Early finger motion
- Occupational therapy programme (graduated range of motion programme) as the fracture unites
Cast care advice
Patients should be educated on cast care, as well as safety-netted about when to return to the ED. Most casts are removed after 4-6 weeks.
Cast care advice should include:
- Keep plaster dry
- Do not scratch underneath the plaster
- Keep elevated for the first week to help reduce the swelling
- Keep fingers moving to improve circulation and reduce stiffness
Patients should be advised to return to the emergency department if they develop any of the following red flags:
- Increasing pain in the area
- Numbness in the fingers
- Increasing swelling in the fingers
- Change of colour in the fingers
- The plaster becomes wet or damaged
Complications
Generic complications
Generic complications, which may occur with any fracture, include:
- Infection
- Bleeding
- Neurovascular injury
- Pain
Specific complications
Specific complications of distal radius fractures include:
- Malunion (most common complication)
- Stiffness/decreased range of movement
- Acute median and/or ulnar nerve damage (~10% of low energy fractures and 30% of high energy fractures)3
- Osteoarthritis
- Extensor pollicis longus rupture: patient will be unable to lift their thumb off the table (3-5%)10
- Non-union
- Sensitive scar
- Chronic regional pain syndrome
Key points
- Fractures of the distal radius are common upper limb injuries following a fall onto an outstretched hand (FOOSH).
- There are three important types of wrist fractures: Colle’s fractures, Smith’s fractures and Barton’s fractures.
- Colles’ fractures are the most common type of wrist fracture (~15% of the population).
- The most common clinical findings are pain, swelling and deformity of the wrist.
- Neurovascular status should be checked distally to any fracture.
- Immediate management involves administering analgesia, reducing displaced fractures and immobilisation of the wrist.
- Definitive management depends on the direction of any displacement of the fracture. Volar displaced fractures always require surgical fixation.
- Specific complications of distal radius fractures include malunion, decreased range of movement, nerve damage (median/ulnar) and osteoarthritis.
Reviewer
Miss Nicola MacKay
Trauma and Orthopaedics Registrar
Editor
Hannah Thomas
References
- Patient.info. Wrist Fractures. Last edited in 2016. Available from: [LINK]
- British Society for Surgery of the Hand (BSSH). Management of distal radius fractures. Last edited in 2020. Available from: [LINK]
- Leah Ahn, Mark Vitale, Orrin Franko. Distal Radius Fractures. Last updated in 2020. Available from: [LINK]
- Geeky Medics. Created in March 2020.
- Derek Dombroski, Christian Veillette. Radial shaft fractures. Last updated in 2008. Available from: [LINK]
- BMJ Best Practice. Wrist fractures. Available from: [LINK]
- Lucien Monfils. X-ray of Colle’s fracture. License: [CC BY-SA]. Available from: [Link]
- Centre for Metabolic Bone Diseases, University of Sheffield. FRAX Risk Assessment Tool. Available from: [LINK]
- British Orthopaedic Association Standards for Trauma and Orthopaedics (BOASTs). Published in 2017. The management of distal radial fractures. Available from: [LINK]
- Kevin C. Chung, Alexandra L. Mathews. Management of complications of distal radius fractures. Published in 2015. Available from: [LINK]
- WG Blakeney. Stabilisation and treatment of Colle’s fracture in elderly patients. Published in 2010. Available from: [LINK]




