- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Hernias are one of the most common general surgical conditions but are often poorly understood. Getting to grips with the underlying anatomy of different hernias will hopefully enable you to identify them with confidence and understand the principles of their management.
This article will cover groin hernias (inguinal, femoral and obturator) and abdominal wall or “ventral” hernias (umbilical, epigastric, Spigelian and incisional).
We will also briefly discuss other hernia types and key differential diagnoses.
What is a hernia?
The often-recited surgical definition of a hernia is “the protrusion of a viscus into an abnormal space”.
In simple terms, a hernia is an organ or piece of tissue that passes through a hole and ends up somewhere it isn’t supposed to be. Herniation most commonly affects abdominopelvic organs but can also involve other parts of the body such as the intervertebral discs of the spine, the lung, or the brain.
Before we dive into the different types, it is important to unpick some of the surgical terminology used to describe hernias (e.g. “a 56-year-old male with a strangulated inguinal hernia”):
- “Reducible” – the contents of the hernia can be manipulated back into their original position through the defect from which they have emerged. These hernias are either left alone or repaired electively.
- “Incarcerated” or “Irreducible” – the contents of the hernia are stuck and cannot be pushed back into their original position. This can be due to sudden constriction of the hernia at the level of the fascial defect resulting in painful swelling of the tissues. Acutely incarcerated hernias should be repaired urgently. Other hernias can gradually become adherent to the surrounding tissues over time without causing any constriction of the contents. Chronically incarcerated hernias are usually repaired electively unless they are very painful or at high risk of obstruction or strangulation.
- “Obstructed” – the contents of a hernia containing bowel are compressed to the extent that the bowel lumen is no longer patent, leading to obstruction. The cardinal features of intestinal obstruction are colicky abdominal pain, distension, vomiting and absolute constipation. These hernias generally require emergency surgery unless they can be reduced very quickly.
- “Strangulated” – compression of the contents of the hernia by the fascial defect prevents blood flow into the tissues, causing ischaemia which may lead to infarction and necrosis. This typically presents with disproportionately severe constant pain, systemic illness and sepsis. These hernias are the most serious and require emergency surgery as soon as possible to salvage or resect their contents.
An abdominal hernia passes through an existing anatomical opening or an acquired fascial defect. Its contents are usually contained within a sac of parietal peritoneum. The opening it emerges from is called the hernia neck. This may be wide or narrow, and its edges may consist of fascial tissue, ligament or bone. The neck is important as it dictates the risk of complications – a loop of bowel trapped in a narrow defect with solid edges is much more likely to become obstructed or strangulated.
What causes a hernia?
Generally speaking, hernias are caused by increased intra-abdominal pressure, weak or damaged tissues, or a combination of both.
Increased intra-abdominal pressure may be due to:
- Chronic cough: COPD, long-term smoking, bronchiectasis, cystic fibrosis
- Abdominal distension: pregnancy, ascites, peritoneal dialysis, obesity (ventral hernias)
- Straining: chronic constipation, prostatism, heavy lifting during work or exercise
- Kyphoscoliosis
Weakened tissues may result from:
- Congenital defects: patent processus vaginalis, patent umbilical ring
- Collagen disorders: Ehlers-Danlos syndrome, vitamin C deficiency, family history of hernias
- Trauma: including surgery
- Ageing
- Chronic malnutrition
- Long-term corticosteroid use
Inguinal hernia
Inguinal hernias are by far the most common type of hernia. They account for over 70% of all hernias, and around 70,000 of them are repaired in England every year.
Definition
An inguinal hernia is an abnormal protrusion of abdominopelvic contents through the superficial inguinal ring into the groin.
Anatomy
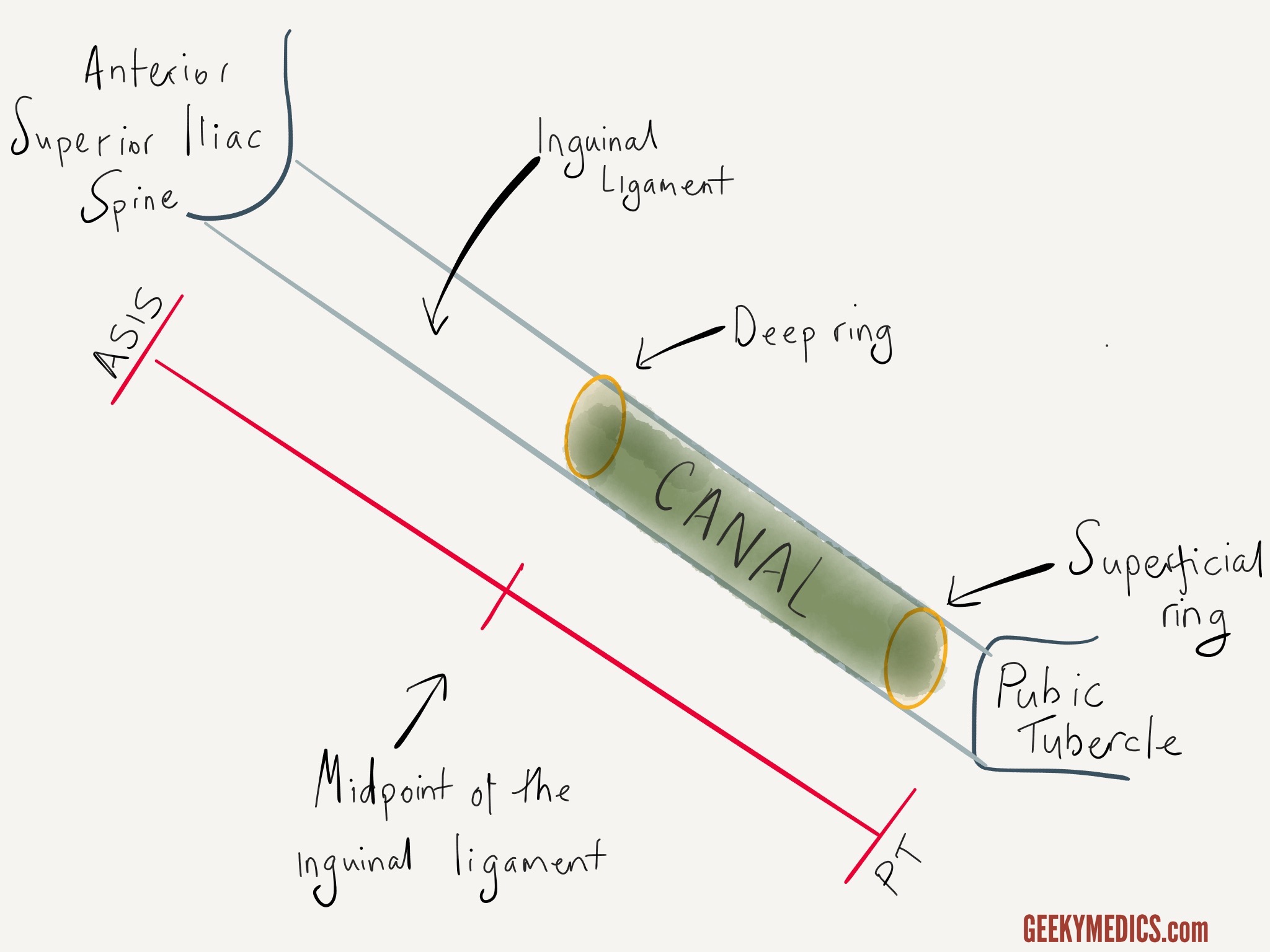
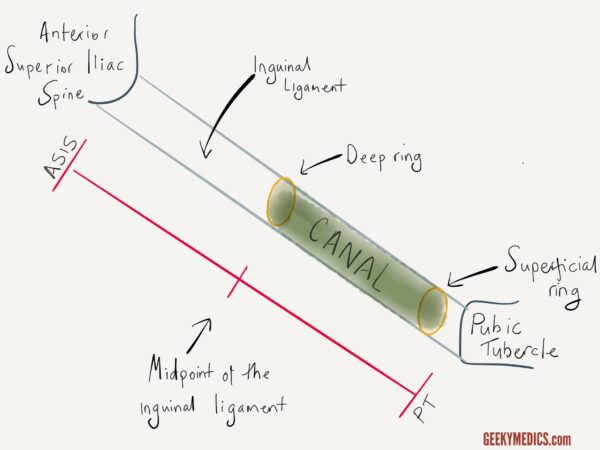
The inguinal ligament runs between the anterior superior iliac spine (ASIS) and the pubic tubercle (PT). Just above this ligament runs a structure known as the inguinal canal. The function of the inguinal canal is to provide a passageway between the peritoneal cavity and the external genitalia. In men, it transmits the spermatic cord to the testis, and in women, it contains the round ligament. In both sexes, it also carries the ilioinguinal nerve and the genital branch of the genitofemoral nerve.
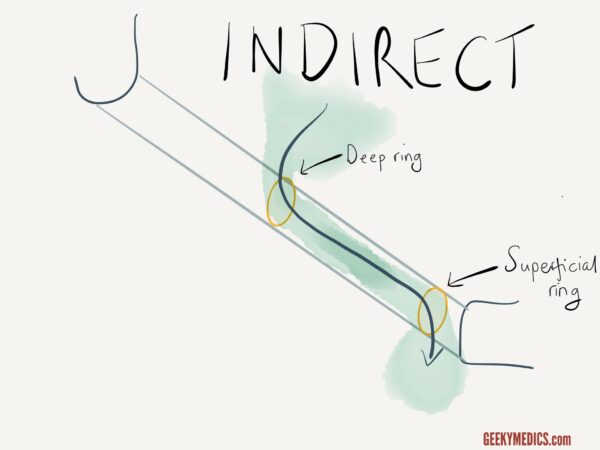
As shown in the diagram below, the inguinal canal is best visualised as a tube or tunnel with an entry point from the abdominal cavity (the deep inguinal ring) and an exit point into the groin (the superficial inguinal ring). The location of these two openings is clinically important and is a common exam question. The deep ring is located just above the mid-point of the inguinal ligament. The superficial ring lies just above and lateral to the pubic tubercle.
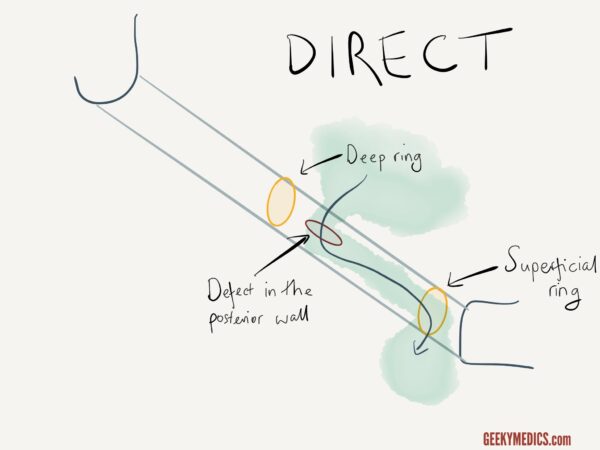
Direct inguinal hernia
A direct inguinal hernia is caused by a weakness in the posterior wall of the inguinal canal in an area known as Hesselbach’s triangle. Abdominal contents (usually just fatty tissue, sometimes bowel) are forced “directly” through this defect into the inguinal canal. The hernia enters the canal medial to the deep ring and exits via the superficial ring, as shown below.
Indirect inguinal hernia
An indirect inguinal hernia follows a different trajectory. Instead of piercing the posterior wall, the abdominal contents enter the deep ring, pass along the length of the inguinal canal and exit via the superficial ring, as shown below.
Differences between indirect and direct inguinal hernias
Both types of inguinal hernia exit via the superficial ring and can sometimes enter the scrotum. This is known as an inguinoscrotal hernia. It is much more common for indirect hernias to do this as the path through both anatomical inguinal rings offers less resistance to the passage of hernia contents.
An appreciation of the anatomical differences can help to distinguish between direct and indirect hernias on clinical examination of the hernia. The principle of this is that if you place your finger over the deep inguinal ring (just above the mid-point of the inguinal ligament), then you can control an indirect inguinal hernia which has been reduced. If when you press the deep ring, the hernia still protrudes, then the hernia is emerging via a defect in the posterior wall medial to this point and is, therefore, a direct hernia.
It is useful to understand this clinical test as it helps remember the difference between the two. However, the clinical application of this kind of assessment is limited as it is not very reliable and doesn’t change management.
Aetiology and risk factors
Inguinal hernias are much more common in men due to the anatomy of their inguinal canals. The incidence in adults peaks at age 70. Interestingly, studies have shown that a low BMI appears to be a risk factor for inguinal hernias, whilst obesity appears to be protective. This may be due to the presence of more intra-abdominal fatty tissue which covers and protects the deep inguinal ring.
Clinical features
Patients often present with a lump in the groin that comes and goes and has slowly increased in size over time. Alternatively, the lump may have popped out suddenly, for example after heavy lifting.
Many inguinal hernias are otherwise asymptomatic. Symptomatic hernias often present with groin pain or discomfort, particularly after coughing, bending over or standing for long periods. Some patients may also report pain or altered sensation over the scrotum or inner thigh due to compression of the ilioinguinal nerve. A small proportion may develop changes in bowel habit or urinary symptoms depending on the contents of the hernia.
Incarcerated, obstructed or strangulated inguinal hernias are a fairly common presentation to emergency departments or surgical assessment units.
The majority of inguinal hernias can be accurately diagnosed on clinical examination as a palpable swelling located above and medial to the pubic tubercle. Larger hernias may extend down into the scrotum. Where there is diagnostic uncertainty, an ultrasound scan of the groin can help differentiate between other possible causes such as enlarged lymph nodes, fatty lumps, or vascular pathology.
Management
The tissues around the inguinal canal are soft and stretchy, and inguinal hernias carry a relatively low risk of obstruction or strangulation of about 2% per year. If the hernia is small and asymptomatic, the patient may wish to leave it alone. However, hernias do tend to gradually increase in size over time and become more bothersome, so most of them will eventually need to be repaired. Patients with larger or symptomatic hernias should be offered surgery to relieve their symptoms and prevent complications.
Mesh repair is the gold standard for inguinal hernias. Direct and indirect inguinal hernias are managed in the same way. The main decision is whether to fix the hernia via open or laparoscopic surgery.
Open repair
Open repair involves directly exploring the inguinal canal via a groin incision, identifying and protecting important structures (including the spermatic cord and ilioinguinal nerve), reducing the contents of the hernia back into the abdominal cavity, and placing a mesh to strengthen the deep inguinal ring and the posterior wall. It is a simple operation with excellent results and can be done under either general or local anaesthetic. This approach is preferred for large inguinoscrotal hernias.
Laparoscopic repair
Laparoscopic repair is also very successful in experienced hands. It has the added benefits of decreased post-operative pain and a faster recovery. The operation involves visualising the anatomy from within the abdominal cavity, opening the peritoneum, pulling the contents of the hernia back inside, and placing a mesh in the preperitoneal space to cover the defect. This approach is preferred for recurrent or bilateral inguinal hernias.
Research has not shown either technique to be superior, so current guidelines recommend an individualised approach tailored to the characteristics of the hernia, the surgeon’s experience and the patient’s preference.
Femoral hernia
Femoral hernias are a less common type of groin hernia, accounting for 3-5% of all hernias. They frequently present with bowel obstruction, but the diagnosis is often missed in clinical practice.
Definition
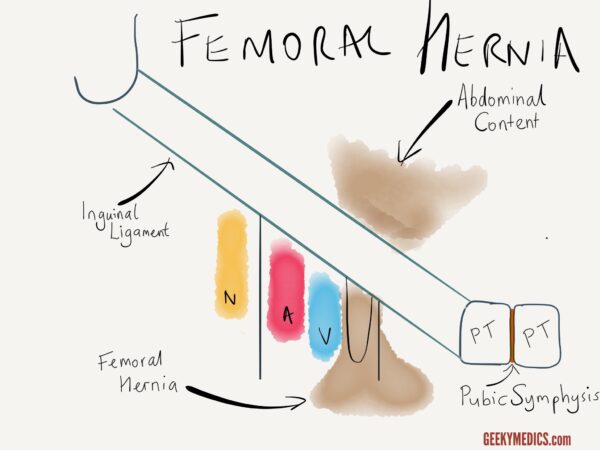
A femoral hernia is an abnormal protrusion of abdominopelvic contents through the femoral canal into the medial upper thigh.
Anatomy
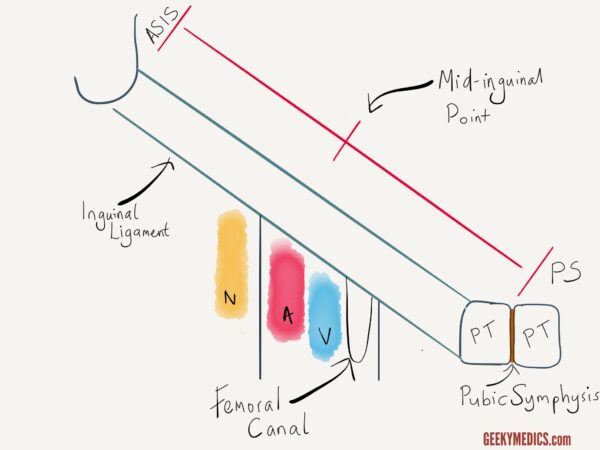
Passing beneath the inguinal ligament are some important structures travelling to the upper leg. Most notably these include the femoral artery, the femoral vein and the femoral nerve. The order in which these structures lie is easy to remember using the ‘NAVY VAN’ mnemonic. With the ‘Y’ signifying the creases of the groin, this illustrates how the structures lie from lateral to medial (nerve, artery, vein).
The femoral artery and vein are enclosed within the femoral sheath. Lying medial to the femoral vein is a space known as the femoral canal. The function of this space is to allow expansion of the femoral vein to increase venous return from the lower limb. The femoral canal normally contains just a small amount of fatty tissue and a lymph node known as the lymph node of Cloquet.
It is important to note that the femoral canal is a narrow space bordered medially by the sharp edge of the lacunar ligament. Femoral hernias are therefore at very high risk of obstruction or strangulation.
Aetiology and risk factors
Femoral hernias are much more common in women. Their incidence increases with age, and they are most likely to affect people over 50. As with inguinal hernias, a low BMI is a risk factor. This is because weight loss diminishes the amount of fatty tissue within the femoral canal, creating a space where hernias can enter.
Interestingly, having a previous laparoscopic inguinal hernia repair is protective against a femoral hernia, as the preperitoneal mesh should also cover the femoral canal.
Clinical features
Femoral hernias may present with a lump in the groin similar to an inguinal hernia. The two can often be differentiated clinically as inguinal hernias are situated above and medial to the pubic tubercle, whereas femoral hernias are located below and lateral to the pubic tubercle. Femoral hernias are usually quite small and are not always easily palpable, especially in overweight patients. Ultrasound can also be used to confirm the diagnosis.
A significant proportion of femoral hernias present as an emergency with symptoms of bowel obstruction or strangulation, but the diagnosis is often missed due to inadequate clinical examination or inadequate imaging. These patients often become very unwell, and the bowel may perforate due to the diagnostic delay. This is why you should always check the groins as part of an abdominal examination.
Management
Due to the high risk of complications, femoral hernias should always be repaired. There are many different ways to do this, but current guidelines advocate laparoscopic mesh repair as the best method.
Obturator hernia
Obturator hernias are very rare, constituting less than 1% of all hernias. Due to their anatomical location, they are difficult to diagnose clinically. This often results in a missed or delayed diagnosis which leads to considerably increased morbidity and mortality for patients.
Definition
An obturator hernia is an abnormal protrusion of abdominopelvic contents through the obturator foramen of the bony pelvis into the medial upper thigh.
Anatomy
The obturator foramen is an anterior opening formed by the rami of the pubis and ischium on either side of the pelvis. It is roughly 3.5cm x 5cm in size and is the largest foramen in the human skeleton. Men tend to have a smooth, oval-shaped obturator foramen, whilst women’s are smaller and more triangular.
“Obturator” means “blocked off” in Latin, reflecting that in life the obturator foramen is almost completely occluded by a layer of fibrous tissue known as the obturator membrane. The obturator internus and obturator externus muscles lie on either side of this membrane, creating a muscular sandwich which further strengthens the seal covering the hole. The obturator artery, vein and nerve form a neurovascular bundle which enters a small gap in the upper edge of the obturator membrane just beneath the superior pubic ramus. These structures then leave the pelvis and pass obliquely through the obturator canal, a short tunnel 2-3cm long and about 1cm wide, to enter the medial compartment of the thigh.
Aetiology and risk factors
Obturator hernias have been nicknamed the “little old lady hernia”. They overwhelmingly affect elderly multiparous women, and like femoral hernias, they are especially common in people who are very thin or have recently lost weight.
The female pelvis and pelvic floor muscles undergo marked changes during pregnancy and as part of normal ageing, creating wider gaps covered by laxer tissues which are easier for things to herniate through. The sharp pointy angles of the female obturator foramen also mean that structures that herniate through it are much more likely to get stuck there.
Clinical features
More than 90% of obturator hernias present as an emergency with an acute abdomen and clinical features of bowel obstruction and/or strangulation. This usually occurs suddenly, but some patients may report self-limiting episodes of subacute obstruction at home previously. These are characterised by attacks of colicky abdominal pain, bloating and nausea/vomiting which resolved within a few hours.
The deep position of the hernia means there is hardly ever a lump to feel on clinical examination. In addition to abdominal symptoms, up to 50% of patients present with pain and altered sensation along the inner thigh due to compression of the obturator nerve by the hernia, which is relieved by flexing the hip and worsened by internally rotating it. This is known as the Howship-Romberg sign and is pathognomonic for an obturator hernia. The Hannington-Kiff sign describes an absent adductor reflex on the affected side, but this can be hard to confidently elicit and is probably not worth relying upon as a diagnostic tool.
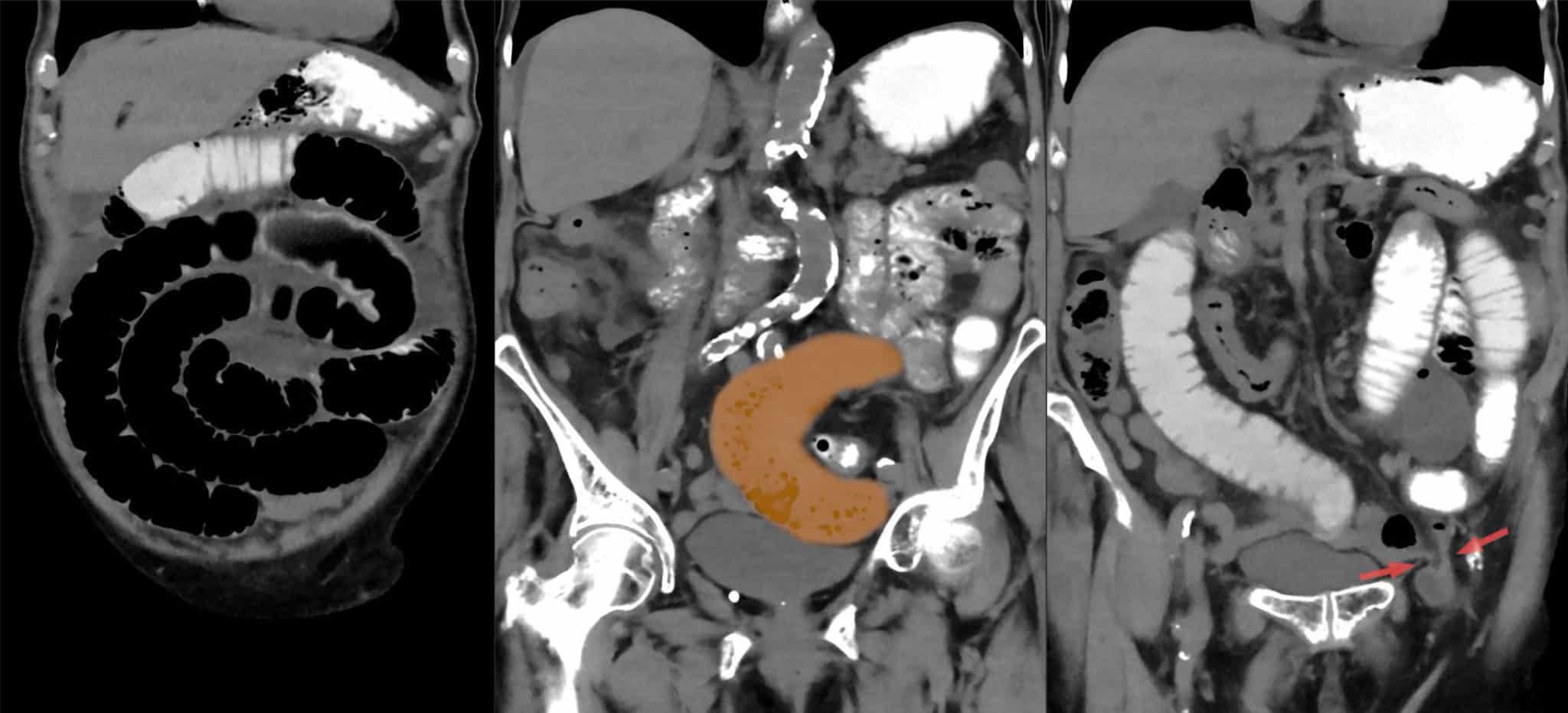
The gold-standard diagnostic test for an undifferentiated acute abdomen is a CT scan of the abdomen and pelvis with portal venous contrast, which should accurately identify an obturator hernia. They are also sometimes diagnosed using ultrasound or picked up unexpectedly on MRI scans.
Management
Obturator hernias generally require emergency surgery to relieve mechanical obstruction and deal with any compromised bowel segments.
As they are so rare, there are no standardised recommendations for their treatment. Open surgery via a lower midline laparotomy remains the standard, especially if bowel resection is required, but a laparoscopic approach offers better visualisation and access to deep structures within the pelvis with improved patient outcomes. Simple suture repair is the fastest and safest way to close the hernia defect in an acutely unwell patient but has a much higher risk of recurrence than a mesh repair.
In the elective setting, obturator hernias can either be repaired laparoscopically or via a groin incision.
Umbilical hernia
Umbilical hernias are the most common ventral hernia. They account for at least 15% of all hernias and are estimated to affect 25% of the general population.
Definition
An umbilical hernia is an abnormal protrusion of intra-abdominal contents through a fascial defect in or around the umbilical ring.
Anatomy
The umbilicus is a dimpled structure on the midline of the anterior abdominal wall at the level of the L3/L4 intervertebral disc.
It is an embryological remnant of the attachment of the umbilical cord which carried the fetal-maternal circulation from the placenta. During fetal development, the umbilical opening provides an entry point for the umbilical arteries and vein. After birth, the umbilical cord detaches and the blood vessels fibrose into a dense stalk of scar tissue known as the cicatrix, which is a crucial landmark for initial port insertion during laparoscopic surgery.
The residual umbilical opening is located in the centre of the cicatrix and is known as the umbilical ring. This gradually fuses with the surrounding midline fascia and normally closes completely within the first 5 years of life.
A true (or direct) umbilical hernia is a congenital problem which occurs when the umbilical ring fails to close, resulting in herniation of intra-abdominal contents into the middle of the cicatrix. This is extremely common, especially in children, and is why so many people have an “outie” belly button. A paraumbilical (or indirect umbilical) hernia is associated with an acquired fascial defect in the linea alba located within 3cm of the umbilical ring and results in a hernia which lies separate from the cicatrix. Umbilical hernias vary considerably, ranging from a few millimetres to a football.
Aetiology and risk factors
Umbilical hernias are more likely to affect women, especially during or after pregnancy, however, they are more likely to cause problems which ultimately require surgery in men. Down’s syndrome and Beckwith-Wiedemann syndrome have been associated with umbilical hernias in children.
Chronically raised intra-abdominal pressure due to obesity or ascites is a major risk factor. Up to 20% of patients with cirrhosis will develop an umbilical hernia secondary to ascites. Umbilical hernias can be lethal to these patients, as they often develop large hernias containing bowel and do not have the physiological reserve to survive an acute complication.
Clinical features
Umbilical hernias are usually asymptomatic. Symptomatic patients usually report a longstanding lump in their belly button which may be causing them varying amounts of bother. Due to their central position in the abdomen, symptomatic umbilical hernias may contain extraperitoneal fat, omentum, small bowel or transverse colon. Hernias containing bowel are at risk of obstruction or strangulation as most have fairly small fascial defects, and the umbilical ring is made from thick fibrous tissue. As many as 20% of umbilical hernias will present with acute complications.
On examination, there will be a palpable swelling in or around the umbilicus. The umbilicus itself may be everted or distorted by the hernia. It is important to note the condition of the overlying skin, which can become stretched and thin and may start to break down, posing a risk of infection.
An umbilical hernia is usually a clinical diagnosis. An ultrasound or CT scan can clarify the anatomy of larger hernias or rule out other pathology if there is any diagnostic uncertainty.
Management
Asymptomatic umbilical hernias have a low risk of complications and can safely be managed conservatively. These patients should be safety-netted about worrying symptoms to look out for and when to seek further medical advice.
International guidelines recommend that the majority of symptomatic umbilical hernias should undergo open repair with a mesh to reduce the risk of recurrence.
Very small hernias less than 1cm in size or women who plan to become pregnant in the future can be treated with simple suture repair instead. Large umbilical hernias more than 4cm in size or patients at high risk of wound infection are better managed with a laparoscopic approach.
Epigastric hernia
Epigastric hernias are a less common type of midline ventral hernia, which account for about 5% of all hernias. They have a relatively low risk of serious complications.
Definition
An epigastric hernia is an abnormal protrusion of intra-abdominal contents through a fascial defect in the linea alba between the umbilicus and the xiphoid process of the sternum.
Anatomy
The linea alba is a dense fibrous band which runs down the midline of the anterior abdominal wall from the xiphoid process to the pubic bone. It is formed by a complex interweaving and decussation of the fibres of the external oblique, internal oblique and transversus abdominis aponeuroses between the two rectus abdominis muscles. Epigastric hernias occur through a congenital or acquired defect in the upper part of the linea alba. These defects are often tiny, and the majority are less than 2cm in size.
Aetiology and risk factors
Epigastric hernias are more common in men and people aged 20-50. As with umbilical hernias, central obesity is a key risk factor as it increases intra-abdominal pressure and weakens the linea alba.
Clinical features
Epigastric hernias are usually asymptomatic. Symptomatic patients commonly present with an upper abdominal lump that comes and goes and may be uncomfortable. Epigastric hernias are unlikely to cause bowel obstruction or ischaemia as most of them only contain extraperitoneal fat. However, this fatty tissue can still strangulate, resulting in acute pain and inflammation around the hernia.
On examination, there will be a palpable swelling in the midline above the umbilicus. In most cases, it will be possible to gently reduce the hernia and feel the fascial defect with your fingers.
Like umbilical hernias, epigastric hernias are usually a clinical diagnosis.
Management
The treatment guidelines for epigastric hernias are the same as for umbilical hernias.
Spigelian hernia
Spigelian hernias are rare, representing 1-2% of all hernias. They are often hard to detect clinically due to their small size and unusual position. This hernia is named after Adriaan van den Spiegel, who described the anatomy of the semilunar line in 1627. However, it should be named after Josef Thaddeus Klinkosch, who first described the hernia in 1764.
Definition
A Spigelian hernia is a lateral ventral hernia characterised by the abnormal protrusion of abdominal contents through a defect in the fascial layers lateral to the rectus sheath.
Anatomy
The semilunar line is a curved tendinous intersection located at the point where the transversus abdominis muscle transitions into its aponeurosis. It forms a visible landmark which runs lateral to the rectus abdominis muscle from the ninth costal cartilage to the pubic tubercle on either side.
The Spigelian fascia is the portion of the transversus abdominis aponeurosis located between the semilunar line and the rectus sheath.
Spigelian hernias occur when a small defect develops in this layer and allows extraperitoneal fat or abdominal contents to escape. They are usually less than 2cm in size and are most likely to occur at or below the level of the arcuate line. This is located roughly halfway between the umbilicus and the pubis and is the point at which the posterior rectus sheath becomes deficient.
The Spigelian fascia also becomes wider here and is pierced by the inferior epigastric vessels. The overlying external oblique aponeurosis is strong and often remains intact, forcing the hernia to spread out within the abdominal wall muscle compartment rather than popping out under the skin. This is known as an interparietal hernia and is another reason Spigelian hernias can be so tricky to spot.
Aetiology and risk factors
Spigelian hernias are slightly more common in women and more likely to affect people aged 40-60.
Clinical features
Spigelian hernias are surrounded by tight fascial layers, making obstruction or strangulation of the contents much more likely. Around 25% of cases present as an emergency with acute complications.
Pain is the most common symptom, and patients often describe a feeling of localised stretching or tightness in the abdominal wall. The hernia may be palpable as a lump lateral to the rectus abdominis muscle, usually located below the umbilicus. However, Spigelian hernias are undetectable clinically in up to 50% of cases, and abdominal tenderness may be the only positive finding on examination.
An ultrasound scan of the symptomatic area can identify a small impalpable Spigelian hernia, but its accuracy may be limited in people with large body habitus. Some are diagnosed with a CT scan, or a diagnostic laparoscopy to investigate unexplained acute abdominal pain.
Management
Spigelian hernias should be repaired as they carry a high risk of complications. As they are rare, there is insufficient evidence to support standardised recommendations for their management. Recent guidelines suggest a laparoscopic approach to aid the identification of the fascial defect and advise using mesh.
Incisional hernia
Incisional hernias are a diverse group of conditions ranging from tiny port site hernias to total abdominal wall failure. They will complicate around 15% of all abdominal operations and have become increasingly common as more and more patients are undergoing surgery at some point in their lives.
Definition
An incisional hernia is a ventral hernia characterised by the protrusion of intra-abdominal contents through the site of a previous surgical incision.
Anatomy
A midline laparotomy through the linea alba is the most frequently used abdominal incision. There is only one fascial layer to open and close, so this technique is easy, fast and provides excellent access without damaging muscles. However, it involves one of the thinnest parts of the abdominal wall, and there is no backup available if the single fascial suture line fails. It is therefore unsurprising that incisional hernias most commonly occur in the midline, especially after an upper midline laparotomy.
Transverse or lateral incisions access specific structures such as the liver, gallbladder, appendix, uterus or retroperitoneal vessels. These involve several fascial layers and require the surgeon to split or cut muscles on the way down. They are more time-consuming to perform, but the fascial closure is stronger as it involves multiple suture lines and is reinforced by extra layers of tissue.
Laparoscopic and robotic surgery involves making multiple small incisions to insert instrument ports. These are known as port sites. The first port is most commonly located above or below the umbilicus, and other ports are then positioned according to the procedure performed. Laparoscopic ports have diameters of 5-12mm, so the incisions are small. However, a fascial defect 1cm in size can still cause a hernia if it is not closed properly, and port site hernias have a high risk of obstruction or strangulation if a loop of bowel manages to get stuck in the tiny hole.
A parastomal hernia is an incisional hernia related to a stoma site. Stoma formation involves the creation of a tunnel through the rectus sheath and rectus abdominis muscle to bring the bowel out onto the skin. This leaves a residual fascial defect which often allows other intra-abdominal contents to escape over time. Parastomal hernias are more likely to occur with a colostomy than with an ileostomy or urostomy.
Aetiology and risk factors
Incisional hernias occur because the fascial closure of the abdominal wall failed to heal properly. Wound healing depends upon the direct approximation of healthy tissue edges with minimal tension, no contamination or infection, a good blood supply, and adequate nutrition. There are numerous factors which may compromise adequate wound healing after abdominal surgery.
Technical factors
The surgeon’s fascial closure may have been suboptimal. For example, they may have used the wrong suture material, failed to approximate the correct fascial layers, left gaps between suture bites, tied loose knots, pulled the suture line overly tight or made a stoma opening too big.
Patient factors
Raised intra-abdominal pressure due to obesity, coughing, vomiting or a post-operative ileus will put additional tension on the fascial closure while it is trying to heal.
Smoking, peripheral arterial disease, diabetes and radiotherapy damage the capillary microcirculation and impair the blood supply to the tissues.
Chronic illnesses such as kidney disease, liver disease and intestinal disorders may result in malnutrition with inadequate protein levels available for building strong scar tissue.
Corticosteroids, immunosuppressant medications and chemotherapy increase the risk of infection and also dampen the inflammatory response to injury, directly impairing wound healing.
Disease-related factors
These include the need for emergency surgery, tissue damage or contamination, inflammatory processes (such as Crohn’s disease) or malignancy, and post-operative wound infections.
Clinical features
Many incisional hernias are asymptomatic. Patients with symptomatic hernias tend to present with a lump which has gradually increased in size since their surgery. Incisional hernias tend to be more painful than primary hernias, with up to 50% of patients experiencing pain or discomfort. Large incisional hernias can also be functionally debilitating as they impair the patient’s core muscle strength and stability. Up to 15% of incisional hernias will present acutely with obstruction or strangulation.
In most cases, there will be a palpable lump close to a previous surgical scar or stoma site. However, it may be difficult to feel the hernia due to scarring or the patient’s body habitus.
Ultrasound can help diagnose small defects, such as port site hernias. Larger hernias and those associated with open incisions should be investigated with a CT scan to facilitate surgical planning. This will allow full characterisation of the anatomy of the fascial defect and hernia contents as well as identification of any other hernias which may have been missed on examination.
Management
Asymptomatic incisional hernias can safely be managed conservatively.
The consensus is that symptomatic incisional hernias should be treated with a mesh repair. There are many open and laparoscopic techniques available, but you don’t need to worry about learning these (unless you’re studying for FRCS!). Symptomatic parastomal hernias can be treated by either reversing the stoma (if possible), performing a mesh repair around the stoma, or moving the stoma to another site on the abdominal wall.
Incisional hernia repairs can be technically challenging as many patients will have scarring and tissue damage from their previous surgery. The risk of recurrence is more than 10% and can be much higher for large hernias. It is important to remember that not all patients will meaningfully benefit from surgery, and there is a chance that a major abdominal wall reconstruction could leave some patients worse off than they were before.
The optimal strategy depends on numerous factors including the patient’s symptoms and quality of life, the nature of their previous operation(s), the anatomy of the fascial defect(s), the likelihood of obstruction or strangulation, the patient’s fitness to undergo further surgery and their risk of postoperative complications. The decision-making process is complex and should be specifically tailored to each case.
Other types of hernia
Richter’s hernia
A Richter’s hernia involves the partial herniation of just one edge of the bowel wall, usually the antimesenteric border of the small intestine, as opposed to its entire circumference.
It is named after August Gottlich Richter, who first described it in 1785. This is not a separate anatomical type of hernia, but a term used to describe a pathological phenomenon which can affect any hernia. It most commonly occurs in femoral hernias, inguinal hernias and ventral hernias with small fascial defects that won’t admit a whole loop of bowel (such as laparoscopic port site hernias). It can result in serious complications, as the herniated portion of the bowel wall can rapidly become strangulated and ischaemic, leading to necrosis, perforation and sepsis.
Patients often present with fairly vague symptoms and clinicians may be falsely reassured by the absence of features of intestinal obstruction. If the compromised bowel is manually reduced back into the abdominal cavity, the patient may develop generalised peritonitis when it perforates.
It is estimated that at least 10% of hernias requiring emergency surgery are Richter’s hernias. When assessing a patient with an acutely painful hernia, it is essential to take any abnormal findings seriously to avoid missing the diagnosis of bowel ischaemia. Red flags include skin changes over the hernia (erythema, cellulitis, bruising or dark discolouration), anxiety, fever, tachycardia, tachypnoea, raised inflammatory markers, acute kidney injury or elevated lactate. Patients with a piece of dead gut inside them also “don’t look right” from the end of the bed – once you’ve seen it, you won’t forget it.
Internal hernia
Unlike external hernias which end up outside the abdomen or pelvis, internal hernias occur when bowel loops remain within the peritoneal cavity but pass through an opening in the peritoneum or the mesentery.
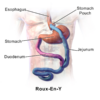
There are numerous congenital types, of which paraduodenal hernias are the most common. Internal hernias are also an important complication of abdominal surgery. Adhesions formed by scar tissue can create tight bands between adjacent structures which tangle up bits of bowel. Any procedure involving a Roux-en-Y reconstruction of the upper gastrointestinal tract – such as oesophagectomy, total gastrectomy, Whipple’s procedure, liver transplants and gastric bypass surgery – creates at least two new mesenteric spaces which small bowel loops can accidentally wander off into.
In addition, weight loss following bariatric surgery considerably increases the risk of herniation due to the rapid loss of intra-abdominal fatty tissue.
Internal hernias can be devastating as a large amount of bowel can end up in the wrong place and suddenly develop closed-loop obstruction or strangulation. Any patient with unexplained abdominal pain and a history of gastric bypass surgery should have an urgent CT scan to rule out an internal hernia.
Hiatus hernia
A hiatus hernia (also known as a hiatal hernia) is characterised by the herniation of abdominal contents into the chest through the oesophageal hiatus of the diaphragm.
The sliding type is extremely common and usually only involves a small part of the top of the stomach slipping upwards. This impairs the function of the lower oesophageal sphincter, leading to heartburn and reflux symptoms. Patients are often told they have these after having a tiny defect noted during a routine endoscopy and can become preoccupied with their diagnosis of a “hernia”.
In contrast, the para-oesophageal type can involve the stomach and multiple other abdominal organs herniating up around the oesophagus en masse. These may result in life-threatening complications and can be very challenging to repair.
Diaphragmatic hernia
Unlike hiatus hernias, which pass through an existing anatomical opening, true diaphragmatic hernias are caused by the herniation of abdominal contents through a pathological defect in the diaphragm muscle. They may be congenital – these include Bochdalek (posterolateral), Morgagni (anteromedial) and central hernias – or acquired, usually following surgical mishaps or blunt or penetrating thoracoabdominal trauma. It is important to maintain a high index of suspicion for a diaphragmatic injury in patients with stab wounds to the junctional zone around the lower chest and upper abdomen.
Subxiphoid hernia
This is a high ventral hernia in the upper abdomen less than 5cm from the xiphoid process or costal margin. It usually develops as an incisional hernia following a median sternotomy, upper midline laparotomy or rooftop incision. It is unusual for these to contain bowel unless they are very large, as the left lobe of the liver covers the fascial defect in most cases. They are usually asymptomatic.
Suprapubic hernia
This is a low ventral hernia occurring in the suprapubic region less than 4cm above the pubic symphysis. It usually develops as an incisional hernia following a lower midline laparotomy or Caesarean section. These can be challenging to repair, especially in obese patients, as the lower posterior rectus sheath is relatively weak and the hernia is close to the bladder and important neurovascular structures. A piece of mesh often has to be anchored directly onto the pubic bone to adequately cover the fascial defect.
Lumbar hernia
This is another rare lateral ventral hernia in which abdominal contents herniate posteriorly through the muscles of the superior or inferior lumbar triangle into the soft tissues of the back. It can occur spontaneously or as a result of surgery or torso trauma.
Sciatic hernia
This is an extremely rare pelvic hernia in which abdominopelvic contents herniate through the greater or lesser sciatic foramen into the gluteal region. It may be mistaken for a buttock abscess.
Perineal hernia
This involves the herniation of abdominopelvic contents through the muscles of the pelvic floor into the perineum. It occurs more frequently as an incisional hernia following radical pelvic surgery, such as abdominoperineal resection of the rectum or pelvic exenteration. It is therefore important for these patients to have their perineal wounds checked at follow-up appointments.
Burst abdomen
A burst abdomen (also known as full-thickness wound dehiscence) involves the failure of the fascial closure of the abdominal wall in the early postoperative period. It can be dramatic and requires a trip to the emergency theatre to put the bowel back where it should be and close everything up again.
Traumatic hernia
Traumatic hernias are thankfully rare. They occur as a result of high-energy blunt trauma to the abdominal wall with a sudden increase in intra-abdominal pressure which disrupts muscle and fascial layers, such as a seatbelt injury, handlebar injury or crush injury.
These mechanisms are associated with severe blunt polytrauma and patients may be critically unwell. There are often direct injuries to the underlying bowel with extensive soft tissue destruction leading to large and complex wounds.
Eponymous hernias
As well as Spigelian and Richter’s hernias, there are many other eponymously named hernias. The ones you are most likely to hear mentioned are named after a surgeon of yore who found an interesting internal organ inside a hernia. Some examples we have encountered in clinical practice include Amyand’s hernia (appendix in an inguinal hernia), de Garengeot’s hernia (appendix in a femoral hernia), and Littre’s hernia (Meckel’s diverticulum in any hernia).
Differential diagnoses – things that aren’t hernias
Sportsman’s hernia
The helpfully named “sportsman’s hernia” (also known as inguinal disruption, Gilmore’s groin, or athletic pubalgia) is not a hernia. It is a poorly understood group of conditions but is generally accepted to be a sprain or tear of the soft tissues in the groin which causes pain around the inguinal ligament and pubic tubercle.
Patients may experience abnormal tension in the inguinal canal due to damage to surrounding structures, and some develop chronic pain. An MRI scan will identify any soft tissue abnormalities. Surgery is only indicated if conservative treatment and physiotherapy are unsuccessful.
Divarication of the recti
Divarication of the recti (also known as rectus diastasis) occurs when the rectus abdominis muscles separate, leading to stretching and thinning of the linea alba to a width of more than 2cm. This causes a bulge in the midline, which can look striking on clinical examination but isn’t a hernia as there is no underlying fascial defect. It is often cosmetically unappealing to patients, especially women who develop it during pregnancy and also can lead to core weakness and instability.
Intensive physiotherapy and exercise programmes are first-line treatments as they can effectively bring the muscles back together again in addition to improving core strength. Surgery is reserved for large symptomatic divarications of more than 5cm and those associated with an umbilical or epigastric hernia.

Pseudohernia
A pseudohernia is a soft tissue bulge resulting from localised muscle paralysis secondary to trauma, nerve root compression by an intervertebral disc prolapse, peripheral neuropathy or infections such as shingles (herpes zoster). This may also be mistaken for a hernia on clinical examination.
References
Reference texts
- Birindelli, A., Sartelli, M., Di Saverio, S. et al.2017 update of the WSES guidelines for emergency repair of complicated abdominal wall hernias. World J Emerg Surg 12, 37 (2017).
- Dabbas N, Adams K, Pearson K, Royle G. Frequency of abdominal wall hernias: is classical teaching out of date? JRSM Short Rep. 2011 Jan 19;2(1):5.
- Seker G, Kulacoglu H, Öztuna D, Topgül K, Akyol C, Çakmak A, Karateke F, Özdoğan M, Ersoy E, Gürer A, Zerbaliyev E, Seker D, Yorgancı K, Pergel A, Aydın I, Ensari C, Bilecik T, Kahraman İ, Reis E, Kalaycı M, Canda AE, Demirağ A, Kesicioğlu T, Malazgirt Z, Gündoğdu H, Terzi C. Changes in the frequencies of abdominal wall hernias and the preferences for their repair: a multicenter national study from Turkey. Int Surg. 2014 Sep-Oct;99(5):534-42.
- Hemberg, A., Montgomery, A., Holmberg, H. et al.Waist Circumference is not Superior to Body Mass Index in Predicting Groin Hernia Repair in Either Men or Women. World J Surg 46, 401–408 (2022).
- HerniaSurge Group. International guidelines for groin hernia management. Hernia. 2018 Feb;22(1):1-165.
- NICE Technology appraisal guidance [TA83]: Laparoscopic surgery for inguinal hernia repair. National Institute for Health and Care Excellence 2004. Available from: [LINK]
- Bedewi MA, El-Sharkawy MS, Al Boukai AA, Al-Nakshabandi N. Prevalence of adult paraumbilical hernia. Assessment by high-resolution sonography: a hospital-based study. Hernia. 2012 Feb;16(1):59-62.
- Henriksen NA, Montgomery A, Kaufmann R, Berrevoet F, East B, Fischer J, Hope W, Klassen D, Lorenz R, Renard Y, Garcia Urena MA, Simons MP; European and Americas Hernia Societies (EHS and AHS). Guidelines for treatment of umbilical and epigastric hernias from the European Hernia Society and Americas Hernia Society. Br J Surg. 2020 Feb;107(3):171-190.
- Henriksen NA, Kaufmann R, Simons MP, Berrevoet F, East B, Fischer J, Hope W, Klassen D, Lorenz R, Renard Y, Garcia Urena MA, Montgomery A; on behalf of the European Hernia Society and the Americas Hernia Society. EHS and AHS guidelines for treatment of primary ventral hernias in rare locations or special circumstances. BJS Open. 2020 Apr;4(2):342-353.
- Rennie, S.R., Eliopoulos, C. & Gonzalez, S. Evaluation of the obturator foramen as a sex assessment trait. Forensic Sci Med Pathol(2022).
- Li, Z., Gu, C., Wei, M. et al.Diagnosis and treatment of obturator hernia: retrospective analysis of 86 clinical cases at a single institution. BMC Surg 21, 124 (2021).
- Park, Jinyoung MD, PhD. Obturator hernia: Clinical analysis of 11 patients and review of the literature. Medicine: August 21, 2020 – Volume 99 – Issue 34 – p e21701
- Schizas, D., Apostolou, K., Hasemaki, N. et al.Obturator hernias: a systematic review of the literature. Hernia 25, 193–204 (2021).
- Ponten, J.E.H., Somers, K.Y.A. & Nienhuijs, S.W. Pathogenesis of the epigastric hernia. Hernia16, 627–633 (2012).
- Hertzer NR, Montie JE. Spigelian hernia: a review of the literature and report of three cases. Cleveland Clinic Journal of Medicine Jan 1971, 38 (1) 13-18. Available from: [LINK]
- Mittal T, Kumar V, Khullar R, Sharma A, Soni V, Baijal M, Chowbey PK. Diagnosis and management of Spigelian hernia: A review of literature and our experience. J Minim Access Surg. 2008 Oct;4(4):95-8.
- Hanzalova, I., Schäfer, M., Demartines, N. et al.Spigelian hernia: current approaches to surgical treatment—a review. Hernia (2021).
- Muysoms FE, Miserez M, Berrevoet F, Campanelli G, Champault GG, Chelala E, Dietz UA, Eker HH, El Nakadi I, Hauters P, Hidalgo Pascual M, Hoeferlin A, Klinge U, Montgomery A, Simmermacher RK, Simons MP, Smietański M, Sommeling C, Tollens T, Vierendeels T, Kingsnorth A. Classification of primary and incisional abdominal wall hernias. Hernia. 2009 Aug;13(4):407-14.
- P W G Carne, G M Robertson, F A Frizelle, Parastomal hernia, British Journal of Surgery, Volume 90, Issue 7, July 2003, Pages 784–793
- Kingsnorth A. The management of incisional hernia. Ann R Coll Surg Engl. 2006 May;88(3):252-60.
- SandersD L, Kingsnorth A N. The modern management of incisional hernias BMJ 2012; 344 :e2843
- Regelsberger-Alvarez CM, Pfeifer C. Richter Hernia. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing 2022. Available from: [LINK]
- Sheen AJ, Stephenson BM, Lloyd DM, et al. ‘Treatment of the Sportsman’s groin’: British Hernia Society’s 2014 position statement based on the Manchester Consensus Conference. British Journal of Sports Medicine 2014;48:1079-1087.
- P Hernández-Granados, N A Henriksen, F Berrevoet, D Cuccurullo, M López-Cano, S Nienhuijs, D Ross, A Montgomery, European Hernia Society guidelines on management of rectus diastasis, British Journal of Surgery, Volume 108, Issue 10, October 2021, Pages 1189–1191.
Image references
- Figure 1. Geeky Medics. Anatomy of the inguinal canal.
- Figure 2. Geeky Medics. Direct inguinal hernia.
- Figure 3. Geeky Medics. Indirect inguinal hernia.
- Figure 4. James Heilman, MD. A large right sided hernia. License: [CC BY-SA]
- Figure 5. Rocco Cusari. Ernia inguino-scrotale permagna. License: [CC BY-SA]
- Figure 6. Geeky Medics. Anatomy of the femoral canal.
- Figure 7. Geeky Medics. Femoral hernia.
- Figure 8. Hellerhoff. Duenndarmileus bei inkarzerierter Femoralhernie 82W – CT coronar – 001 – Annotation. License: [CC BY-SA]
- Figure 9. BodyParts3D. Obturator foramen 03 anterior view. License: [CC BY-SA]
- Figure 10. Henry Vandyke Carter. Obturator membrane and obturator canal. License: [public domain]
- Figure 11. Purpleblue. Belly Button 002. License: [CC BY-SA]
- Figure 12. Nosoyfranco45. Quién da más. License: [CC BY-SA]
- Figure 13. Milliways, Hernia umilicalis. License: [CC BY-SA]
- Figure 14. Adêle Mongrédien. Linea alba. License: [public domain]
- Figure 15. Geeky Medics. Linea alba.
- Figure 16. Henry Vandyke Carter. Semilunar line. License: [public domain]
- Figure 17. AfroBrazilian.Hernia spiegheli 01. License: [CC BY-SA]
- Figure 18. Geeky Medics. Abdominal incisions.
- Figure 19. Kim. Cholecytectomy incisions 4 days post operation. License: [CC BY-SA]
- Figure 20. PacoPeramo. Hernia epigástrica. License: [CC BY-SA]
- Figure 21. Mikael Häggström. Colostomy and parastomal hernia. License: [public domain]
- Figure 22. Hellerhoff. Richter-Hernie 82W – CT paraaxial KM pv – 001 – Annotation. License: [CC BY-SA]
- Figure 23. Hellerhoff. Richter-Hernie 82W – CT sagittal KM pv – 001. License: [CC BY-SA]
- Figure 24. Niels Olson. InternalHernia. License: [CC BY-SA]
- Figure 25. BruceBlaus, Roux-En-Y Part 2. License: [CC BY-SA]
- Figure 26. Fedenko. Диагностика диастаза прмых мышц живота 01. License: [CC BY-SA]