- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Local anaesthesia is used to prevent the sensation of pain and allow procedures and surgeries without general anaesthetic. It can be administered in various ways:
- Infiltration of local anaesthetic
- Peripheral nerve block (usually for limb surgeries, e.g. using ultrasound imaging to inject around the brachial plexus)
- Central anaesthesia such as spinal or epidural
This infiltration of local anaesthetic OSCE guide provides a step-by-step approach to infiltrating local anaesthetic in an OSCE setting.
Background
Mechanism of action
Nerve conduction is blocked by inhibiting sodium ion influx through sodium channels in the neuronal membrane. Agents have to be in an unionised form to penetrate the neural membrane.
pKa determines the ratio of ionised to unionised local anaesthetic. The closer the pKa is to the body’s pH, the faster the onset of the anaesthetic. The stability of the agents is increased by making the pH slightly acidic. This is one of the reasons injections are associated with a burning sensation.
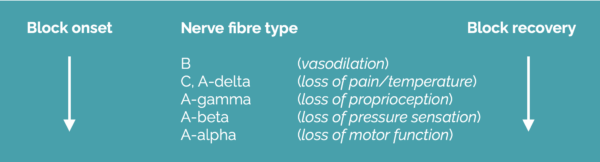
Anaesthetic blockage affects the smallest diameter nerves first, with larger myelinated nerves taking longer for onset. Smaller nerves are also quicker to recover from anaesthetic blockage.
Local anaesthetics are ineffective in infected tissue due to the localised hypoxia creating an acidic environment.
Types of local anaesthetic
These are broadly separated into two groups, ester-linked and amide-linked.
Esther-linked anaesthetics
Esther-linked anaesthetics are metabolised by pseudocholinesterase and produce para-aminobenzoic acid (PABA) as a by-product. This is important because PABA is associated with allergic reactions. Therefore, these agents are not frequently used in clinical practice.
Examples of esther-linked agents include:
- Cocaine (the only vasoconstrictor, still used in rhinoplasty)
- Procaine
- Tetracaine
Amide-linked anaesthetics
Amide-linked anaesthetics are metabolised in the liver, and allergic reactions are rare. Allergic reactions can occur if PABA is used as a preservative. Amide-linked agents are frequently used in clinical practice. All amides have an ‘i’ in the prefix.
Examples of amide-linked agents include:
- Lidocaine: most commonly used, short-acting, dosage is 3mg/kg plain or 7mg/kg with adrenaline (e.g. xylocaine 1% with 1:200,000 adrenaline)
- Bupivacaine: slower onset but longer duration upward of 8 hours effective anaesthesia, reports up to 24 hours, dosage is 2mg/kg (not changed by the addition of adrenaline), can be cardiotoxic (ventricular arrhythmias), particularly in patients with acidosis, hypercarbia or hyperaemia
- Levobupivacaine: similar to bupivacaine but reduced cardiotoxicity, dosage is 3mg/kg
- Prilocaine: rapid onset and metabolism, metabolite causes methaemoglobinaemia
- Ropivacaine: long-acting with reduced cardiac and central nervous system toxicity
Topical anaesthetics
Topic anaesthetics are frequently used in paediatrics before venepuncture or cannulation. Examples include:
- Ametop: 4% tetracaine, requires an occlusive dressing, onset is 45 minutes
- EMLA (eutectic mixture of local anaesthetic): 2.5% lidocaine and 2.5% prilocaine, onset is >1 hour
Local anaesthetic additives
Adrenaline
Adrenaline can be added to local anaesthetic in differing concentrations. Adrenaline causes vasoconstriction which reduces intraoperative bleeding.
Care must be taken with adrenaline as larger doses increase myocardial activity (e.g. tachycardia, hypertension, potential arrhythmias).
Examples of local anaesthetic with adrenaline preparations include:
- Xylocaine: lidocaine with 1:200,000 (1mg/200ml) adrenaline
- Lignospan: lidocaine with 1:80,000 (1mg/80ml) adrenaline
Care should be taken when using local anaesthetics in the hand and digits (use a concentration of 1:200,000). These preparations should not be used in the penis.
Sodium bicarbonate
Sodium bicarbonate (alkaline solution) has also been shown to increase the speed of onset of anaesthetic, enhance its effect and reduce the pain of injection.
Dosage calculations
Dose calculations can be confusing as the concentrations are expressed as a percentage, whereas the maximum dosages are expressed as milligrams per kilogram.
Multiply the percentage by 10 to work out the dosage of anaesthetic per millilitre:
- Lidocaine 1% contains 10mg/ml
- Levobupivicaine 0.25% contains 2.5mg/ml
Local anaesthetic toxicity
Local anaesthetic toxicity is rare but must be recognised and managed promptly. Causes of toxicity include dosage error or inadvertent intravascular injection. Toxicity predominantly affects the central nervous system and cardiovascular system.
Clinical features related to the central nervous system include:
- Dizziness
- Peri-oral paraesthesia
- Disorientation
- Tinnitus
- Muscle twitching
- Seizures (tonic-clonic)
- Coma
Clinical features related to the cardiovascular system (requires higher doses) include:
- Sinus bradycardia due to blockade of the spontaneous pacemaker
- Depression of cardiac contractility
- Sinus arrest
- Bupivacaine can cause refractory ventricular fibrillation
Management of local anaesthetic toxicity:
- Stop any further local anaesthetic infiltration
- Call for help
- Administer high-flow oxygen and follow the ABCDE algorithm
- If circulatory arrest, commence basic life support
- Administer 1.5ml/kg of 20% lipid emulsion (e.g. intralipid emulsion) as a bolus over 1 minute, followed by an infusion of 15ml/kg/hour. Further boluses and changes to the infusion rate may be required.
Recovery may take over an hour, so it is important to continue resuscitation.
Gather equipment
Gather the appropriate equipment:
- Alcohol wipe
- Gloves and necessary personal protective equipment
- Syringe: 5ml, 10ml, 20ml depending on volume required
- Filter needle: blunt needle for drawing up local anaesthetic
- Needle: ideally narrow bore such as a 27 gauge (white) to encourage slow injection, but can use a 22 gauge (blue)
- Gauze to dab any bleeding spots
Select an appropriate local anaesthetic
Select an appropriate local anaesthetic for the procedure. Fast-acting anaesthetics allow speedy onset but wear off quickly, so using a combination is ideal. It is important to be meticulous with calculations to ensure you do not overdose the patient.
Fast acting
Fast-acting local anaesthetics include:
- Lidocaine 1%: 3mg/kg
- Xylocaine 1% (has 1:200,000 adrenaline): 7mg/kg (ideal, as you can give higher volumes and adrenaline causes vasoconstriction reducing bleeding)
These should be used with caution in end-arteries.
Slow acting
Slow-acting local anaesthetics include:
- Levobupivacaine 2mg/kg (better in patients with cardiac disease)
- Bupivacaine 2.5mg/kg
Example dose: 5ml 1% xylocaine mixed with 5mL 0.25% levobupivacaine to make up total 10mL
Introduction
Wash your hands and don PPE.
Introduce yourself to the patient including your name and role.
Confirm the patient’s name and date of birth.
Briefly explain what the procedure will involve using patient-friendly language: “Before we start the procedure, I’m going to use a local anaesthetic to numb the skin. This will involve me using a small needle to inject a local anaesthetic drug just underneath the skin. I’m afraid the injection can give you a burning sensation. This will take around 5 – 10 minutes to work, after this, you should not feel any pain, although you may feel some pulling and pushing”
Check if the patient has an allergy to local anaesthetic (e.g. lidocaine).
Gain consent to proceed with local anaesthesia.
Infiltrate the local anaesthetic
1. Assess the site requiring local anaesthetic and clean the skin with an alcohol wipe away from the wound before injection. Open wounds should be cleaned with saline or aqueous fluid, do not apply alcohol cleansing solution to open wounds.
2. Allow the alcohol to dry on the skin
3. Draw up the required local anaesthetic into a syringe using a red filter needle
4. Mount your narrow gauge needle on the syringe
5. Put a little tension on the skin to make it taut, and introduce the needle below the dermis
6. Withdraw the plunger on the syringe gently to ensure there is no flashback of blood indicating the needle tip is in a vein – if it is, withdraw the needle and compress the area for 30 seconds to prevent haematoma
7. Inject the local anaesthetic very slowly to start, looking at the patient’s reaction. Once you have injected approximately 1mL, begin to advance the needle slowly, injecting as you move, watching the dermis plump up with fluid
8. Repeat this process until you have administered local anaesthetic to the desired area
9. Wait for 5-10 minutes, as this will allow the local anaesthetic and adrenaline to work
10. Test the area with your needle (and the patient’s eyes closed) to see if they feel sharpness. They may feel pulling and pushing but should not feel the pin prick.
11. Once the area is numb, you can start the procedure
12. Remember to place sharps in the sharps bin and any other material in the clinical waste bin
Tips for the infiltration of local anaesthetic
- Use a fine needle to reduce the pain of multiple injections (27 gauge is ideal)
- Move the needle as you inject to prevent large dose intravascular injection
- Inject slowly to reduce the pain of infiltration. Expanding the skin quickly with a fast injection is one of the main causes of pain and may affect your rapport with the patient
- You can combine anaesthetics in one injection (e.g. 5ml of 1% lidocaine and 5ml of 0.25% levobupivacaine). This combines fast onset with a longer duration of anaesthesia. You can also add 1ml of 8.4% sodium bicarbonate to reduce pain and decrease the onset of anaesthesia. Alternatively, some clinicians use a fast-acting local anaesthetic before the procedure and give slow-acting anaesthetic at the end whilst the area is still numb.
- Test for pain sensation before starting any procedure
To complete the procedure…
Explain to the patient that the procedure is now complete.
Thank the patient for their time.
Dispose of your PPE and equipment into an appropriate clinical waste bin.
Wash your hands.
Document details of the local anaesthetic infiltration in the patient’s notes




