- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
This guide provides a structured approach to joint fluid interpretation, including typical joint fluid aspiration results for specific disease processes. Reference ranges vary between labs, so always consult your local medical school or hospital guidelines.
Normal joint fluid results (adults)
- Colour: colourless
- Clarity: transparent
- Viscosity: normal
- WBC: < 200 cells/mm3
- Neutrophils (% of total WCC): <25 %
- Gram stain: negative
- Crystals: negative
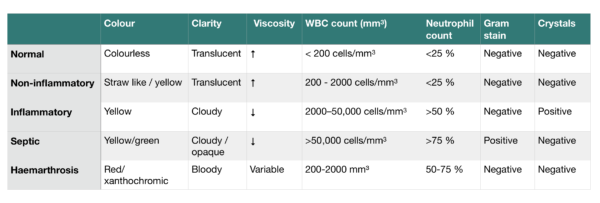
Overview of joint fluid findings
This table summarises the typical findings in joint fluid analysis for various pathologies.
Non-inflammatory joint effusion
Aetiology
Causes of non-inflammatory joint effusion include:
- Osteoarthritis
- Trauma
Clinical features
Typical clinical features of non-inflammatory joint effusion include:
- Localised joint pain
- Gradual onset of symptoms
- Pain on movement, worse at the end of the day
- Crepitus
Joint fluid findings
Typical joint fluid analysis findings include:
- Colour: straw-like
- Clarity: translucent
- Viscosity: increased
- WBC: 200 – 2000 cells/mm3
- Neutrophils: <25 %
- Gram stain: negative
- Crystals: negative
Further investigations
Further investigations for suspected non-inflammatory joint effusion include:
- Blood tests (FBC, CRP): typically normal in non-inflammatory joint effusion.
- X-ray of the affected joint(s): may reveal fractures or other changes consistent with osteoarthritis.
- MRI of the affected joint(s): useful for assessing the ligaments and menisci of the knee for pathology.
Inflammatory joint effusion
Aetiology
Causes of inflammatory joint effusion include:
- Rheumatoid arthritis
- Reactive arthritis
- Psoriatic arthritis
- Acute gout or pseudogout
Clinical features
Rheumatoid arthritis
Typical clinical features of inflammatory joint effusion associated with rheumatoid arthritis include:
- Symmetrical swollen, warm, erythematous and painful joints
- Usually, the small joints of the hands and feet are affected
- Morning stiffness greater than one hour
- May be associated with systemic features (e.g. fever, weight loss)
Psoriatic arthritis
Typical clinical features of inflammatory joint effusion associated with psoriatic arthritis include:
- Affected joints are generally red or warm to the touch
- Small joints of the hand and wrist are commonly affected (most commonly the distal interphalangeal joints)
- Typically asymmetrical in presentation
- Associated changes to the nails, such as onycholysis and hyperkeratosis
Acute gout
Typical clinical features of inflammatory joint effusion associated with acute gout include:
- A single hot, swollen and tender joint (most commonly the metatarsophalangeal joint at the base of the big toe).
Pseudogout
Typical clinical features of inflammatory joint effusion associated with pseudogout include:
- A single hot, swollen and tender joint (most commonly the knee joint)
Joint fluid findings
Typical joint fluid analysis findings include:
- Colour: yellow
- Clarity: cloudy
- Viscosity: decreased
- WBC: 2000–50,000 cells/mm3
- Neutrophils: >50 %
- Gram stain: negative
- Crystals: positive
- Gout – needle negative birefringent crystals
- Pseudogout – rhomboid positively birefringent crystals
Further investigations
Further investigations for suspected inflammatory joint effusion include:
- Full blood count
- CRP
- ESR
- Urate (raised in gout)
- Antibodies (e.g. anti-CCP, rheumatoid factor – both typically positive in rheumatoid arthritis)
- X-ray of the joint: may reveal joint erosions/destruction
Septic joint effusion
Aetiology
Causes of septic joint effusion include:
- Staphylococcus aureus
- Streptococci
- Neisseria gonorrhoeae (young sexually active adults)
- Escherichia coli (elderly, intravenous drug users)
Clinical features
Typical clinical features of septic joint effusion include:
- A single painful, swollen and warm joint
- Associated fever and other systemic features (e.g. tachycardia, hypotension)
Joint fluid findings
Typical joint fluid analysis findings include:
- Colour: yellow/green
- Clarity: cloudy/opaque
- Viscosity: decreased
- WBC: >50 000 cells/mm3
- Neutrophils: >75 %
- Gram stain: often positive
- Crystals: negative
Further investigations
Further investigations for suspected septic joint effusion include:
- Full blood count: WCC is typically raised
- CRP: typically raised
- Blood cultures: may identify the causative organism
- Joint fluid culture: may identify the causative organism
- X-ray of the joint: may reveal joint destruction
Haemorrhagic joint effusion
Aetiology
Causes of haemorrhagic joint effusion include:
- Trauma
- Tumours
- Bleeding disorders
Clinical features
Typical clinical features of a haemorrhagic joint effusion include:
- A painful, swollen and warm single joint
- Restricted range of movement in the affected joint
- Excessive bruising surrounding the affected joint
Joint fluid findings
Typical joint fluid analysis findings include:
- Colour: red/xanthochromic
- Clarity: bloody
- Viscosity: variable
- WBC: 200-2000 mm³
- Neutrophils: 50-75%
- Gram stain: negative
- Crystals: negative
Further investigations
Further investigations for suspected haemorrhagic joint effusion include:
- Full blood count: haemoglobin may be reduced if the bleeding was significant
- Coagulation studies: may reveal impaired coagulation
- X-ray of the affected joint: may identify associated fractures in the context of trauma
Worked examples
Case 1
A 23-year-old female presents with a swollen and warm knee joint that is very painful on flexion. On systemic enquiry, she also mentions she has been suffering from purulent vaginal discharge for several weeks. She is sexually active with multiple partners and uses condoms inconsistently. Her knee joint is aspirated, with the results shown below.
Results
Joint fluid analysis reveals the following:
- Colour: yellow
- Clarity: opaque
- Viscosity: decreased
- WBC: 60,000 mm³
- Neutrophils: 90 %
- Gram stain: negative
Answer
Septic arthritis (the most likely causative organism is Neisseria gonorrhoeae)
Case 2
A 25-year-old male presents with pain in the metacarpophalangeal (MCP) joints of both hands. He has morning joint stiffness that lasts for more than an hour. On examination, you note multiple warm, swollen MTP joints, with associated erythema. The largest joint effusion is aspirated, with the results shown below.
Results
Joint fluid analysis reveals the following:
- Colour: yellow
- Clarity: cloudy
- Viscosity: decreased
- WBC: 40,000 mm³
- Neutrophils: 60 %
- Gram stain: negative
Answer
Inflammatory joint effusion (secondary to rheumatoid arthritis)
Case 3
A 67-year-old female presents with left knee stiffness and pain that worsens with movement. Her symptoms have progressively worsened over the last 8 years and she is now struggling to mobilise outside. On examination, there is left knee swelling, with significant crepitus noted on passive flexion and extension. There is no associated erythema or warmth. There is a positive sweep test on assessment and the effusion is aspirated, with the results shown below.
Results
Joint fluid analysis reveals the following:
- Colour: colourless
- Clarity: translucent
- Viscosity: increased
- WBC: 1500 mm³
- Neutrophils: 15 %
- Gram stain: negative
Answer
Non-inflammatory joint effusion (secondary to osteoarthritis)
References
- Abdullah S, Young‐Min SA, Hudson SJ, Kelly CA, Heycock CR, Hamilton JD. Gross synovial fluid analysis in the differential diagnosis of joint effusion. Journal of Clinical Pathology. 2007;60(10):1144-1147. doi:10.1136/jcp.2006.043950.
- Goldenberg DL. Bacterial arthritis. In: Ruddy S, Harris ED, Sledge CB, Kelley WN, eds. Kelley’s Textbook of Rheumatology. 6th ed. Philadelphia, Pa.: Saunders; 2001:1469–1483.
- Schumacher HR Jr. Synovial fluid analysis and synovial biopsy. In: Ruddy S, Harris ED, Sledge CB, Kelley WN, eds. Kelley’s Textbook of Rheumatology. 6th ed. Philadelphia, Pa.: Saunders; 2001:605–619.




