- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Kawasaki disease is an acute self-limiting systemic vasculitis of unknown cause that mainly affects children under the age of five (but can affect children of any age, including infants and teenagers).1
It is found worldwide but has a preponderance for children of East Asian origin. In the UK, it affects 8 per 100,000 children under the age of five.2 In Japan, the incidence is over 200 per 100,000 children under the age of five.3
Kawasaki disease is a medium-sized artery vasculitis, particularly affecting the coronary arteries. Early diagnosis and treatment are important to reduce the risk of major cardiac complications, including coronary artery aneurysms and sudden cardiac death.1
Aetiology
The aetiology of Kawasaki disease remains unknown. The leading theory is that an infectious trigger causes an immune-mediated response in a genetically susceptible child. However, no definite genetic variants or infectious agents have been identified.3
Risk factors
Risk factors for Kawasaki disease include:4
- Asian ethnicity, especially Japanese
- Aged <5 years (80% of cases occur in those under the age of five)
- Male sex (male to female ratio 1.5:1)
Clinical features
Kawasaki disease should be considered in any child with a fever lasting five or more days.5 It is a clinical diagnosis, and there is no diagnostic test.
The diagnosis of Kawasaki disease is based on the American Heart Association diagnostic criteria.6
American Heart Association diagnostic criteria
Presence of fever (usually ≥39°C) for at least five days, plus at least four out of five key features:
- Mucositis: erythema and cracking of the lips, strawberry tongue and/or oral erythema
- Conjunctivitis: bilateral conjunctivitis without exudate
- Rash: maculopapular, erythroderma or erythema multiforme
- Peripheral changes: erythema, oedema and/or desquamation of the hands and feet
- Cervical lymphadenopathy
It is important to ask parents or carers whether any of these features have been present since the onset of the fever, as some may have resolved by the time of assessment.5
Some children do not fulfil the full diagnostic criteria yet later develop coronary artery aneurysms. This is known as incomplete Kawasaki disease.
Clinical examination
All children presenting with fever should be thoroughly examined, covering all major body systems. Examination findings suggesting Kawasaki disease are the features in the diagnostic criteria above. Some examples are shown in Figure 1.

Natural history
Kawasaki disease usually follows three phases:3
- Acute phase (1-2 weeks from fever onset): high fever, irritability, rash, mucositis, peripheral erythema and oedema.
- Subacute phase (2-4 weeks from fever onset): afebrile, most clinical features begin to resolve, desquamation of the hands and feet. The highest risk period for developing cardiac complications.
- Convalescent phase (4-8 weeks from fever onset): asymptomatic period, clinical features have resolved. Coronary artery aneurysms often improve but may get worse.
Differential diagnoses
Fever is a common paediatric presentation. The differential diagnosis is broad, including viral, bacterial and rheumatological conditions. Possible differential diagnoses include:1,4
- Scarlet fever or acute rheumatic fever (Group A streptococcus)
- Toxic shock syndrome or staphylococcal scalded skin syndrome (Staph aureus)
- Paediatric multisystem inflammatory syndrome temporally associated with COVID-19 (PIMS-TS)
- Viral exanthems: erythema infectiosum (parvovirus B19) or infectious mononucleosis (EBV)
- Measles
- Systemic-onset juvenile idiopathic arthritis
- Steven-Johnson syndrome / toxic epidermal necrolysis
Investigations
There is no diagnostic test for Kawasaki disease, and it is a clinical diagnosis. All patients should undergo an echocardiogram. Other investigations may be useful in suspected incomplete Kawasaki disease or to exclude alternative diagnoses.
Beside investigations
Relevant bedside investigations include:6
- ECG: may show arrhythmias or ST-T changes if myocarditis or myocardial infarction occurs
- Urinalysis: may show sterile pyuria
Laboratory investigations
Relevant laboratory investigations include:6
- Baseline blood tests (FBC, U&E, LFTs): there may be anaemia, raised white cells and raised platelets. LFTs may be deranged if hepatitis occurs.
- ESR and/or CRP: often significantly raised
- Anti-streptolysin O titre (ASOT): to exclude group A streptococcal infection
Consider PIMS-TS blood tests if suspected as a differential diagnosis (troponin, D-dimer, coagulation with fibrinogen, and ferritin).
Imaging
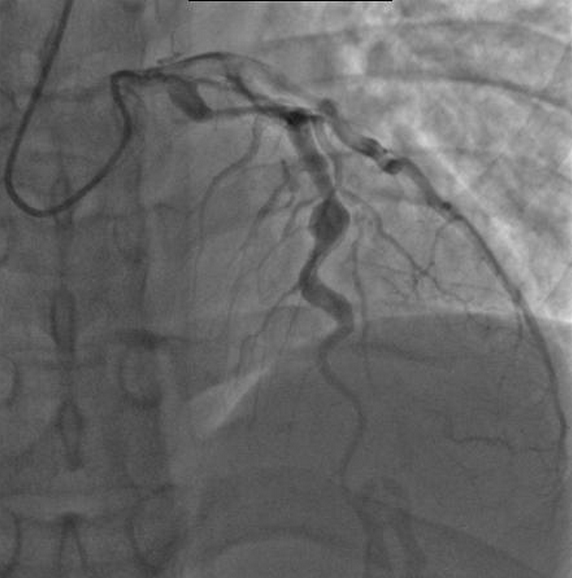
An echocardiogram is essential. It should be performed as soon as Kawasaki disease is suspected but should not delay treatment (e.g. if the child presents out-of-hours or to a hospital without a suitably qualified sonographer).
Typical findings on echocardiogram include:6
- Coronary artery aneurysms (as shown in Figure 2)
- Valvular disease (e.g. mitral regurgitation)
- Coronary artery thrombosis
- Poor ventricular function/evidence of myocarditis
- Pericardial effusion/evidence of pericarditis
The echocardiogram can be normal in the first week of the disease, so this does not rule out the diagnosis. Serial echocardiograms are needed to monitor disease progression. Their timings depend on the initial findings and will be guided by cardiology.
Management
Children with Kawasaki disease should be admitted to hospital. Early treatment aims to prevent coronary artery aneurysms. Oral aspirin and intravenous immunoglobulin (IVIG) are the main treatments used.2
Aspirin
Aspirin is thought to reduce the risk of coronary artery aneurysms and thrombosis through its antiplatelet and anti-inflammatory effects.
Typically, high-dose aspirin is given until the fever has resolved for 48 hours, then low-dose aspirin for approximately 6 weeks (duration will be guided by cardiology).4
Reye’s syndrome
Aspirin is usually contraindicated in children under 16 due to the risk of Reye’s syndrome, a rare acute encephalopathy associated with liver failure. However, in Kawasaki disease, the benefits are felt to outweigh this risk.1
Intravenous immunoglobulin (IVIG)
An infusion of IVIG within the first 10 days of illness can reduce the incidence of coronary artery aneurysms. Clinical improvement should be seen within 36 hours.
A second dose of IVIG may be given if an improvement is not seen. Other treatments, including corticosteroids or infliximab (an anti-TNF agent), may be used in refractory cases or in those with risk factors for IVIG resistance.4
Complications
Most children with Kawasaki disease recover well, and the overall mortality rate is <0.5%.4 However, complications can include:4
- Coronary artery aneurysms: 15-25% of untreated children develop aneurysms, but the risk is much lower with early treatment. Giant aneurysms may rupture, causing cardiac tamponade.
- Myocarditis/pericarditis
- Arrhythmias
- Valvular disease (e.g. mitral regurgitation)
- Coronary artery thrombosis/myocardial infarction
- Sudden cardiac death
Key points
- Kawasaki disease is an acute self-limiting systemic vasculitis of unknown cause.
- It mainly (but not exclusively) affects children under five.
- Key clinical features include fever ≥5 days, rash, conjunctivitis, mucositis with strawberry tongue, peripheral changes in the hands and feet, and cervical lymphadenopathy.
- Kawasaki disease is a clinical diagnosis, and all patients should undergo echocardiography.
- Treatment includes oral aspirin and IVIG.
- Serious complications can occur, particularly coronary artery aneurysms.
- Multidisciplinary discussion is advised, including cardiology, infectious diseases, and rheumatology input.
Reviewer
Dr Catriona Anderson
Consultant Paediatric Rheumatologist
University of Edinburgh / NHS Lothian
Editor
Dr Chris Jefferies
References
- Patient UK. Kawasaki Disease. Published 2020. Available from: [LINK]
- Eleftheriou D, Levin M, Shingadia D et al. Management of Kawasaki disease. Arch Dis Child. 2014;99(1):74-83. Available from: [LINK]
- Rife E and Gedalia A. Kawasaki Disease: an Update. Curr Rheumatol Rep. 2020; 22(10):75. Available from: [LINK]
- BMJ Best Practice. Kawasaki disease. Published 2019, updated 2022. Available from: [LINK]
- National Institute for Health and Care Excellence. NG143: Fever in under 5s: assessment and initial management. Published 2019, updated 2021. Available from: [LINK]
- McCrindle BW, Rowley AH, Newburger JW et al. Diagnosis, Treatment, and Long-Term Management of Kawasaki Disease: A Scientific Statement for Health Professionals From the American Heart Association. Circulation. 2017;135(17):e927-e999. Available from: [LINK]
- Dong Soo Kim. Kawasaki. Licence: [CC BY-SA 4.0]
- mprice18. KawasAngio. Licence: [CC BY 3.0].




