- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
What is a lumbar puncture?
A lumbar puncture (LP), or “spinal tap”, is an important and commonly used procedure carried out across a wide range of specialities. It is, therefore, important to understand its indications, the steps involved and the potential complications.
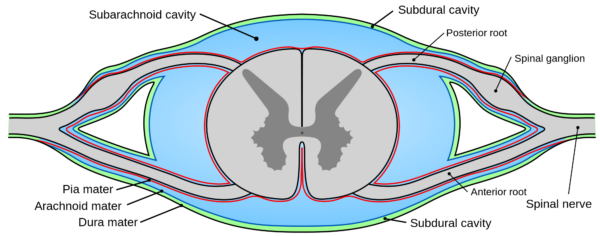
It is also worth learning the layers the needle passes through during the procedure, as this is a common question in medical exams (Figure 2). It should be noted that this guide is not intended to be used for performing this procedure on a patient. Instead, it is aimed at informing medical students in preparation for exams including relevant lumbar puncture anatomy.
Anatomy
A lumbar puncture is an invasive test designed to access the subarachnoid space in the lower spinal canal. The brain and spinal cord are covered by three layers of meninges- the dura, arachnoid, and pia mater (Figure 1). The subarachnoid space lies between the arachnoid and pia mater and contains a solution called cerebrospinal fluid (CSF). CSF is a clear, colourless fluid that provides lubrication around the spinal cord, maintains intracranial pressure, acts as a mechanical shock absorber and transports various metabolic products. The human body contains approximately 100-150ml of CSF. As you can see below, the subarachnoid space lies close to the ventral and dorsal columns of the spinal cord, therefore anatomical spatial awareness is crucial to performing a safe and accurate lumbar puncture.
Indications
A lumbar puncture may need to be performed for a variety of reasons, both diagnostic and therapeutic: ²
- Cerebrospinal fluid analysis (i.e. meningitis, multiple sclerosis, subarachnoid haemorrhage)
- Spinal epidural (i.e. during labour)
- Spinal medications (i.e. analgesia, chemotherapy, antibiotics)
- Fluid removal (i.e. to reduce intracranial pressure)
Contraindications
Performing a lumbar puncture in a patient with any of the following problems may be contraindicated and in rare circumstances can lead to life-threatening complications. Therefore, a thorough review of the patient’s medical history and presenting complaint should always be sought beforehand, and senior review or neurosurgical advice taken if there is any doubt. 2,3
- Suspicion of raised intracranial pressure
- Anticoagulant therapy (i.e. Warfarin)
- Thrombocytopenia or other clotting disorders
- Suspicion of a spinal abscess
- Risk of herniation (i.e. Arnold-Chiari malformation)
- Acute spinal cord trauma
- Congenital spinal abnormalities
In any of the above circumstances, imaging with CT or MRI should be undertaken before consideration of lumbar puncture. 3
Gather equipment
Gather the appropriate equipment to perform a lumbar puncture (these often come as a sterile lumbar puncture set in many hospitals):
- Lumbar puncture needle: recent evidence supports the use of an atraumatic needle to reduce the risk of post-procedure headaches. Needle size is based on experience and clinical judgement.5
- Sterile field: to cover the patient and the bed
- Chlorhexidine cleaning solution (0.5 % in alcohol 70%) or alternatively iodine
- Manometer: to measure the opening pressure
- Sample collection containers
- Local anaesthetic (typically lidocaine 1%)
- Syringe (5-10ml) and needles for local anaesthetic administration (usually need one for drawing up anaesthetic and one for administration)
- Dressing to apply after the lumbar puncture is complete
- Pen for marking the planned insertion site
Introduction
Wash your hands and don PPE if appropriate.
Introduce yourself to the patient including your name and role.
Confirm the patient’s name and date of birth.
Explain what the procedure will involve using patient-friendly language: “Today I’ve been asked to perform a lumbar puncture, which involves inserting a fine needle into the back to collect a small sample of fluid. I’ll also be using some local anaesthetic, to make the procedure as comfortable as possible. It’s really important that we carry out this test because [insert reason the LP is being performed]. There are some complications that can be associated with performing a lumbar puncture, some of the more common things include a headache and some bruising of the skin after the procedure. There are some rare but much more serious complications, which include damage to nerves resulting in pain and weakness in the legs and also infection.”
Gain consent to perform a lumbar puncture.
Ask the patient if they have any pain before continuing with the clinical procedure.
Identify the insertion site
Map out the insertion site on the patient:
- With the patient standing, mark out L4 by joining a line between the highest points of the iliac crests.
- Palpate above for L3 and below for L5.
- The insertion site can be marked out either between L3/4 or L4/5 depending on the patient’s anatomical features.
Position the patient
Position the patient lying on their side in a fetal position: ask the patient to flex forwards whilst bringing their knees up towards their chest.
Prepare the insertion site
Clean the insertion site and the surrounding area thoroughly using chlorhexidine solution and allow to dry.
Wash your hands and don sterile gloves.
Apply a sterile drape with an opening over the site of insertion.
Local anaesthetic
Draw up the local anaesthetic and then replace the drawing needle with a new one for the injection.
Inject local anaesthesia around the site and allow time for it to take effect (at least a few minutes).
It is important to warn the patient that this will sting initially but then should quickly go numb.
Perform the lumbar puncture
Press the lumbar puncture needle to the patient’s skin over the insertion site and ask if it feels sharp (if it does, it suggests more local anaesthetic or time is needed).
If the patient is unable to feel the sharp sensation you should proceed with performing the lumbar puncture.
Advance the lumbar puncture needle through the insertion site slowly, tilted slightly cranially. The bevel of the needle should face laterally as you insert it. If using an atraumatic needle, you first insert the short introducer needle and then insert the longer atraumatic needle through this.
The needle passes through the following layers before it reaches the subarachnoid space:
- Skin
- Subcutaneous fat
- Supraspinous ligament
- Interspinous ligament
- Ligamentum flavum
- Dura mater
- Subdural space
- Arachnoid mater
As the needle passes through the three defined ligaments, three ‘pops’ (sudden reductions in resistance) will normally be felt. After the third ‘pop’ (ligamentum flavum) the dura should be breached and CSF should begin to flow through the lumen of the lumbar puncture needle. If there is no CSF flowing through the needle, try withdrawing the needle very slightly and rotating the bevel of the needle to face cranially.

Measure the opening pressure
Once CSF is flowing through the lumbar puncture needle, you can measure the opening pressure by attaching a manometer and recording at what level the meniscus of the CSF settles at. Measurement of opening pressure does not need to be performed routinely.
Collect a sample of CSF
CSF should be collected using an aseptic non-touch technique as it drips from the back of the lumbar puncture needle.
Removal of CSF can be diagnostic (e.g. suspected meningitis) or therapeutic (e.g. benign intracranial hypertension). You should extract an appropriate volume based on your intentions (typically 8-15mL for diagnostic purposes), and place in the appropriate laboratory containers.
For some conditions, such as subarachnoid haemorrhage, it is important to number the containers sequentially so you know in which order the CSF samples were taken (this can allow you to differentiate between a traumatic tap and subarachnoid haemorrhage).
Removal of the needle
Slowly remove the lumbar puncture needle and compress the site with some sterile gauze until you apply a dressing.
Immediately dispose of the lumbar puncture needle into a sharps bin.
To complete the procedure…
Dispose of the remaining clinical equipment into a clinical waste bin.
Wash your hands.
Explain to the patient that the procedure is now complete and advise them to lay flat for at least the next 30 minutes.
Dispose of PPE appropriately and wash your hands.
Ask the patient and nursing staff to inform you if they notice the site becoming red, inflamed or painful.
Send the CSF samples to the laboratory for analysis.
Interpretation of results
When a lumbar puncture is performed for diagnostic reasons, the results can be interpreted with a thorough analysis of the CSF (Table 1). Some components of this analysis can be done at the bedside, while others require specialist review in the lab. 7
| Component | Where is this done? | Interpretation |
| Opening pressure | Bedside (attach a manometer to the LP needle after insertion) | Normal is 8-20cm CSF |
| Appearance | Bedside | Normal is clear Cloudy/purulent suggests meningitis Blood-stained suggests a subarachnoid haemorrhage or a traumatic LP. A SAH will typically result in multiple consistently bloody samples, whereas in the case of a traumatic LP the amount of blood should reduce significantly in each subsequent sample. |
| Total protein | Laboratory test | Normal is 0.15-0.45 g/L |
| Glucose | Laboratory test-(alongside blood glucose concentration) | Normal is 40-60% of blood glucose |
| Gram stain and culture | Laboratory test | Performed if bacteria are suspected |
| Microscopy for cell counts | Laboratory test | High RBC is suggestive of a traumatic tap High total WCC is suggestive of an infection High neutrophils suggest a bacterial meningitis High lymphocytes suggest viral/TB/fungal meningitis |
In patients presenting with clinical signs of meningitis (fever, neck stiffness, headache), there are three primary sources to distinguish between- viral, bacterial, and tuberculous (Table 2). Viral meningitis is usually self-limiting, whereas bacterial meningitis and tuberculous require prompt treatment with the appropriate antimicrobials. Therefore, if any form of meningitis is suspected, microbiology results should not delay management, and patients should be started on immediate empirical antibiotic therapy.
| Viral | Bacterial | TB | |
| Opening pressure | Normal | Raised | Raised or Normal |
| Protein | Raised or Normal | Raised | Raised |
| Glucose | Normal | Low | Low |
| WCC | Raised | Raised | Raised or Normal |
| Cells present | Mainly lymphocytes | Mainly neutrophils | Lymphocytes |
Complications of lumbar puncture 2
- Headache
- Infection
- Bleeding
- Cerebral herniation (i.e. Arnold-Chiari malformation)
- Radiculopathy
- Back pain
References
- Henry Gray. Gray’s Anatomy. Thecal Sac. Available from: [LINK].
- Kimberly Johnson DS. Lumbar Puncture: Technique, indications and complications in adults. UptoDate. 2018 [cited 2018 Jun 11]. Available from: [LINK].
- Engelborghs S, Niemantsverdriet E, Struyfs H, Blennow K, Brouns R, Comabella M, et al. Consensus guidelines for lumbar puncture in patients with neurological diseases. Alzheimer’s Dementia Diagnosis, Assess Dis Monit. 2017;8:111–26.
- Rochwerg Bram, Almenawer Saleh A, Siemieniuk Reed A C, Vandvik Per Olav, Agoritsas Thomas LL et al. Atraumatic (pencil-point) versus conventional needles for lumbar puncture: a clinical practice guideline. BMJ. 2018;361.
- Abe KK, Yamamoto LG, Itoman EM, Nakasone TAF, Kanayama SK. Lumbar puncture needle length determination. Am J Emerg Med. 2005;23(6):742–6.
- Henry Gray. Gray’s Anatomy. Supraspinatus ligament. Available from: [LINK].
- Paul Hamilton IB. Neurological Investigations. In: Kerr E, editor. Data Interpretation for Medical Students. 2nd ed. Lancaster: Carnegie Book Production; 2012. p. 223–7.
Editor
Samantha Strickland
Reviewer
Mr George Spink (FRCS SN)
Consultant Neurosurgeon