- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Mastitis is a painful inflammatory condition of the breast. A breast abscess is a localised collection of pus occurring in the breast.
30% of lactating women develop mastitis, most within 2-3 weeks postpartum.1 Non-lactational mastitis occurs in 5-9% of women, most commonly in women of reproductive age.
Aetiology
Anatomy
The breast contains breast lobules, each draining to a milk duct which empties to the surface of the nipple.
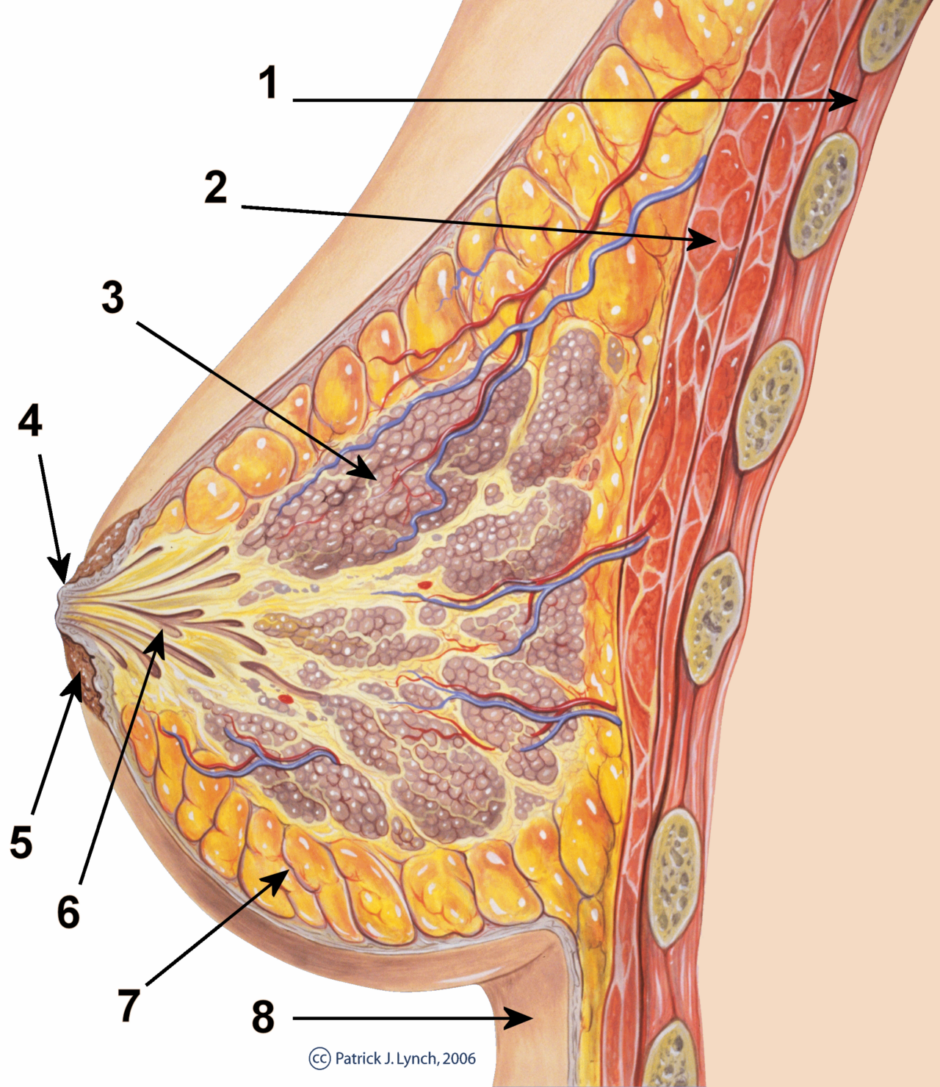
Injury to the nipple skin during breastfeeding provides an entry point for the bacteria to enter, resulting in mastitis which can progress to breast abscess. Inverted nipples predispose to breast infection due to obstruction of the ducts.
Pathophysiology
Breast infections (mastitis) can be divided into three categories:2
- Lactational: occurs during breastfeeding, the most common organism is Staphylococcus aureus
- Non-lactational: occurs in non-lactating women of any age. The infection is usually mixed, the commonest organisms are staph aureus, enterococci, and anaerobic bacteria.
- Granulomatous: a rare breast infection which occurs in women with diabetes mellites, autoimmune diseases and sarcoidosis.
Up to 30% of lactating women can develop mastitis. Periductal mastitis occurs in 5-9% of non-lactating women of reproductive age.
A breast abscess is a complication of mastitis, although it can occur without previous mastitis. Up to 10% of women with mastitis will progress to developing a breast abscess.
Risk factors
Lactational mastitis happens due to milk stasis due to reduced breastfeeding. This can happen due to:3
- Changes in feeding regime
- Introduction of bottle feeding
- Poor attachment of the infant to the breast
- Maternal stress and fatigue
Non-lactational mastitis is commonly seen in smokers due to damage to ducts secondary to hypoxia.
Other risk factors for mastitis include:
- Inverted nipples
- Nipple piercings
- Skin conditions such as eczema
- Diabetes
- Immunosuppression
Clinical features
History
Typical symptoms of mastitis/breast abscess include:
- Erythema of the breast
- Swelling of the breast
- Painful breast
- Fever and general malaise
Other important areas to cover in the history include:
- If the patient is lactating
- Risk factors (listed above)
It is important to be aware of inflammatory breast cancers masquerading as mastitis.
Clinical examination
Typical clinical findings of mastitis/breast abscesses on breast examination include:
- Warm/hot skin
- Tender, firm breast
- The presence of fluctuation suggests abscess formation
An untreated breast abscess can present with spontaneous rupture and discharge from the abscess cavity.

Differential diagnoses
Differential diagnoses to consider in the context of mastitis or a breast abscess include:
- Engorged breasts: usually happens in the first few days postpartum. Usually bilateral with tender, painful swollen breast. Mastitis is commonly unilateral.
- Galactocele: smooth round painless swelling, systemic features of fever and malaise are absent
- Breast cancer (inflammatory cancer): presents as diffuse painful redness with skin oedema (peau d’orange). It is important to complete management with antibiotics and assess for complete resolution of mastitis symptoms as this excludes inflammatory breast cancer.
- Fat necrosis of breast: presents as a firm lump with bruised skin. There is usually a history of trauma with no systemic features of infection. Fat necrosis will resolve spontaneously.
Investigations
Mastitis is a clinical diagnosis and does not require investigations. If a breast abscess is suspected, a breast ultrasound should be performed to confirm the diagnosis.
Management
Mastitis
Management of mastitis includes:4
- Analgesia
- Advice to continue breastfeeding
- Addressing any predisposing risk factors
- Oral antibiotics
In lactating women, prescribe flucloxacillin 500mg QDS 10-14 days. If penicillin-allergic, prescribe erythromycin or clarithromycin. In non-lactating women, prescribe co-amoxiclav. If penicillin-allergic, prescribe erythromycin or clarithromycin with metronidazole.
Consider hospital admission if there are signs of sepsis, haemodynamic instability, or the patient is immunocompromised.
Breast abscess
If breast access is suspected, refer the patient urgently to the local breast clinic. The diagnosis is confirmed using ultrasound.
Initial management is usually ultrasound-guided aspiration of the breast abscess. The aspirate is sent for culture and sensitivity, with the results guiding antibiotic therapy. Repeated ultrasound-guided aspirations may be required.
Surgical open drainage is required if the patient is septic, the overlying skin is compromised, or ultrasound-guided aspiration fails. During open surgical drainage, the abscess wall should be sent for histology.
If the abscess does not resolve after antibiotics and ultrasound aspirations, an ultrasound-guided core biopsy should be performed to exclude malignancy or granulomatous mastitis.
Granulomatous mastitis is difficult to treat. The mainstay of treatment includes antibiotics and corticosteroids and rarely surgery.

Complications
If left untreated, mastitis can progress to a breast abscess. Recurrent mastitis can lead to periductal fistulas.
Prognosis
Mastitis and associated abscesses usually respond well to treatment leading to complete resolution. Non-lactational breast abscesses have a higher reoccurrence rate, and repeated infections can lead to periductal fistulas. Granulomatous mastitis is often recurrent.
Key points
- Mastitis is a painful inflammatory condition of the breast which, if left untreated, can lead to the formation of a breast abscess
- Up to 30% of lactating women can develop mastitis. Smoking is the most important risk factor in non-lactational mastitis.
- Mastitis is a clinical diagnosis, the presence of fluctuation on breast examination suggests abscess formation
- Early treatment with appropriate antibiotics (depending on lactational vs non-lactational status) is important in preventing abscess formation.
- If a breast abscess is suspected, patients should be referred urgently to the local breast clinic. Treatment involves antibiotics and ultrasound-guided aspiration.
- Recurrent infections can lead to complications, including periductal fistulas.
Reviewer
Mr Pawel Pietrzak
Consultant Breast Surgeon
Editor
Dr Chris Jefferies
References
- NICE CKS. Mastitis and Breast Abscess. Available from: [LINK]
- Hughes L, Mansel R, Webster D. Benign disorders and diseases of the breast. Saunders; 2009.
- Bundred N. The aetiology of periductal mastitis. The Breast. 1993;2(1):1-2.
- Dixon J. Breast Infection. BMJ. 2013;347(dec16 1):bmj.f3291-bmj.f3291.
Image references
- Figure 1. Patrick J. Lynch and Morgoth666. Breast anatomy. License: [CC BY]
- Figure 2. Arturoborrero. Mama con drenaje. License: [CC BY-SA]