- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Contraception (or birth control) prevents pregnancy by stopping either ovulation, fertilisation or implantation.
There are many methods of contraception (each with advantages and disadvantages):
- Natural family planning
- Barrier methods
- Combined hormonal contraceptives
- Progestogen-only contraceptives
- Long-acting reversible contraceptives (LARCs): intrauterine, injection, implant
- Sterilisation
- Emergency contraception
It is important to understand the different methods of contraception available and be able to counsel individuals regarding their contraceptive options so that they can make an informed decision.
Contraceptive choice
When deciding on a method of contraception, a patient-informed decision (guided by clinical advice) should be made. The patient may wish to involve a partner in the decision-making process.
It is important to explore the patient’s ideas, concerns and expectations about contraceptive options. When counselling patients regarding contraception, it is important to cover:
- Mode of action
- Hormonal content
- Side effect profile
- Risks and potential complications
- Effect on menstruation
- Effectiveness
- Method of use and practicality
- Reversibility and effect on future fertility
- Follow-up requirements
Not all contraceptives will be suitable for all patients.
UK Medical Eligibility Criteria (UK MEC)
The Faculty of Sexual and Reproductive Health (FSRH) produce the UK Medical Eligibility Criteria for Contraceptive Use (UK MEC) which guides clinicians on the safety of different methods of contraception based on patient characteristics and medical co-morbidities:
- UKMEC 1: no restriction
- UKMEC 2: benefit generally outweighs the risk
- UKMEC 3: theoretical or proven risk generally outweighs the benefit
- UKMEC 4: contra-indicated
Natural family planning
Natural family planning, or fertility awareness, is where intercourse is timed to coincide with the times during the menstrual cycle when ovulation is least likely.
Fertility signs such as body temperature and cervical mucous are monitored by the individual. This aims to prevent pregnancy by reducing the risk of sperm being present during ovulation.
This method is unsuitable for individuals with irregular menstrual cycles.
Benefits
- There are no side effects from this type of contraception
- It is acceptable to most faiths and cultures
Limitations
- Much less effective form of contraception
- Must avoid sex or use other contraception around the time of ovulation
- Requires significant patient commitment to record daily fertility signs
- Fertility signs are unreliable when breastfeeding
- Fertility signs can be affected by illness and stress
- Does not protect from sexually transmitted infections
Unintended pregnancy rate
- Percentage of individuals experiencing an unintended pregnancy within 1 year with typical use of natural family planning = 24%
Barrier methods
Barrier methods of contraception reduce the risk of pregnancy by acting as a barrier to stop sperm from entering the cervix and subsequently stopping sperm from fertilising the ovum.
Barrier methods are the only method of contraception which will prevent sexually transmitted infections (STIs). Therefore, barrier methods should be recommended to all patients, in addition to a more effective method of contraception.
External condoms
External condoms (sometimes referred to as ‘male condoms’) are barriers made of latex, polyisoprene or polyurethane that cover the penis to prevent semen containing sperm from entering the vagina as well as preventing transmission of STIs.

Benefits
- Significantly reduces STI transmission
- Side effects are rare
- Non-hormonal method
Limitations
- Can break, split or tear during use
- Can interrupt intercourse to put a external condom on
- Should not be used with oil-based lubricants (risk of breaking)
- Need to know the correct technique for using condoms
- Some patients are allergic to latex condoms (alternative materials are available)
Unintended pregnancy rate
- Percentage of individuals experiencing an unintended pregnancy within 1 year with typical use of external condoms = 18%
Internal condoms
Internal condoms (also sometimes referred to as female condoms) are a barrier made of polyurethane inserted into the vagina to prevent sperm from passing through the cervix and fertilising an ovum.

Benefits
- Significantly reduces STI transmission
- Side effects are rare
- Non-hormonal method
Limitations
- Can break, split or tear during use
- May interrupt intercourse to put the internal condom in place
- Should not be used with oil-based lubricants (risk of breaking)
- Need to know the correct technique for using condoms
- Internal condoms are not as widely available as external condoms
Unintended pregnancy rate
- Percentage of individuals experiencing an unintended pregnancy within 1 year with typical use of internal condoms = 21%
Diaphragm/cervical cap
The diaphragm is a silicone cup placed over the cervix as a barrier to sperm. This is similar to a cervical cap, which is smaller and also placed over the cervix. Spermicide must be used with the diaphragm and cervical cap.

Benefits
- Only used during intercourse
- Can be put in place in advance of intercourse
- Side effects are rare
- Non-hormonal method
Limitations
- Can break, split or tear during use
- May interrupt intercourse to put the diaphragm/cap in
- Patients must be comfortable self-examining and taught the correct technique for using a diaphragm/cap
- Must be left in place for six hours following last intercourse (if subsequent intercourse occurs, more spermicide should be inserted)
- Does not protect against STIs
Unintended pregnancy rate
- Percentage of individuals experiencing an unintended pregnancy within 1 year with typical use of the diaphragm/cervical cap = 12%
Combined hormonal contraceptives
Combined hormonal contraceptives contain synthetic versions of both oestrogen and progesterone. They work by mimicking the luteal phase of the menstrual cycle, leading to the inhibition of the hypothalamic-pituitary-gonadal axis. This prevents the release of LH and FSH needed for ovulation.
Combined contraceptives further reduce the risk of pregnancy by thickening the cervical mucus to prevent sperm passage and by thinning the endometrium to reduce the chance of implantation.
Medical contraindications
Certain patient groups are contraindicated from using combined contraceptives:
- Migraine with aura
- Current breast cancer
- Significant VTE risk factors (e.g. previous VTE, thrombogenic mutations, previous stroke, SLE, atrial fibrillation, age >35 and smoking >15 cigarettes daily)
- Cardiovascular risk factors: hypertension (>160mmHg systolic or >100mmHg diastolic), history of ischaemic heart disease
- Severe liver disease
These contraindications are listed in full in the UKMEC guidelines.
Exogenous oestrogen increases the risk of VTE. Any risk factors for VTE should be considered before prescribing combined contraceptives.
Combined oral contraceptive pills (COCP)
Combined oral contraceptive pills contain oestrogen and a progestogen (synthetic progesterone).
Traditionally, patients take the pill on a 21/7 cycle (i.e. 21 days of taking the pill at the same time each day, then a 7-day break where they will have a period-like withdrawal bleed)
Depending on patient preference and suitability, other regimens can be used, such as 21/4, 63/7, or continuous use with no hormone-free interval. Commonly prescribed examples of the COCP are Microgynon 30® and Rigevidon®.
This type of contraception is most suited to individuals who are good at remembering to take pills daily and who tolerate hormonal contraceptives.
Benefits
- No interruption to intercourse
- Can be stopped at short notice if not tolerated
- Less strict “missed pill rules” than the progestogen-only pill
- May make periods more regular, lighter and less painful
- May reduce the risk of ovarian, endometrial and bowel cancer
- May have therapeutic benefits in gynaecological disorders, including endometriosis and menorrhagia
Limitations
- Effectiveness is reduced if a pill is forgotten
- Side effects may include headaches, nausea, breast tenderness and mood swings
- Vomiting and diarrhoea may affect the effectiveness
- Certain drugs (e.g. anti-epileptics) may affect the effectiveness
- Increases the risk of VTE and stroke
- Potentially increases the risk of breast and cervical cancer while using the COCP
- Does not protect from STIs
Unintended pregnancy rate
- Percentage of individuals experiencing an unintended pregnancy within 1 year with typical use of COCP = 9%
Contraceptive patches
Contraceptive patches deliver oestrogen and a progestogen through the skin (transdermally).
They are approximately 4x4cm in size and can be applied to any skin except the breast, where the tissue is oestrogen sensitive. Common sites to apply them are on the back, abdomen and buttocks.
One patch is applied for 7 days and then immediately changed for a new patch. Traditionally, 3 patches are worn for 21 days in total, and then a 7-day patch-free interval is taken, where a patient may have a period-like withdrawal bleed. As with the COCP, tailored regimens can be used.
This type of contraceptive is suited to patients who do not mind wearing patches but tend to forget pills.
Benefits
- Do not need to remember daily like the pill
- No interruption to intercourse
- Can be stopped at short notice if not tolerated
- May make periods more regular, lighter and less painful
- May reduce the risk of ovarian, endometrial and bowel cancer
- Vomiting and diarrhoea do not affect effectiveness unlike the pill
Limitations
- Protection from pregnancy may be affected if they forget to change the patch or if it falls off
- Side effects may include headaches, nausea, breast tenderness and mood swings
- Certain drugs may affect effectiveness including some anti-epileptic drugs
- Increases the risk of VTE and stroke
- Potentially increases the risk of breast and cervical cancer while using the patch
- Does not protect from STIs
Unintended pregnancy rate
- Percentage of individuals experiencing an unintended pregnancy within 1 year with typical use of contraceptive patches = 9%
Vaginal rings
The contraceptive vaginal ring (also known as the NuvaRing®) is a small plastic ring self-inserted high in the vagina and secretes oestrogen and a progestogen.
The ring is inserted into the vagina for 21 days, then removed for a 7-day break before the next ring is put in. Again as with the COCP, tailored regimens can be used (e.g. wearing 3 rings in a row for 63 days, then taking a 7-day break).

Benefits
- Do not need to remember daily like the pill
- No interruption to intercourse
- Can be stopped at short notice if not tolerated
- May make periods more regular, lighter and less painful
- May reduce the risk of ovarian, endometrial and bowel cancer
- Vomiting and diarrhoea do not affect effectiveness unlike the pill
Limitations
- Side effects may include headaches, nausea, breast tenderness and mood swings
- Certain drugs may affect protection including some anti-epileptic drugs
- Increases the risk of VTE and stroke
- Potentially increases the risk of breast and cervical cancer while using the ring
- Does not protect from STIs
- Can become dislodged
Unintended pregnancy rate
- Percentage of individuals experiencing an unintended pregnancy within 1 year with typical use of combined hormonal contraception = 9%
Progestogen-only pill (POP)
The traditional progestogen-only pill (POP) is taken daily without any breaks. These pills do not contain any oestrogen. There are several types of POP:
- Desogestrel POP (e.g. Cerazette®): works mainly by inhibiting ovulation, thickening cervical mucus and thinning the endometrium. This POP should be taken at the same time each day to be effective (12-hour window if missed pill).
- Norethisterone and levonorgestrel POPs: work mainly by thickening cervical mucus and thinning the endometrium. These POPs are less commonly used as the missed pill window is 3 hours.
- Drospirenone POP (newly released): inhibits ovulation and is taken daily (similar to other POPs), however 4 pills out of a 28-day pack are hormone-free placebos to allow for a break (24-hour window if missed pill).
Benefits
- Suitable for patients where oestrogen is contraindicated or those who are intolerant to oestrogen
- Daily pill so don’t have to remember to start and stop pills
- No interruption to intercourse
- Can be stopped at short notice if not tolerated
- Evidence suggests POPs are safe post-partum and when breastfeeding
Limitations
- Protection from pregnancy is affected if a pill is forgotten
- More strict “missed pill rules” than COCP
- May cause irregular bleeding or amenorrhoea
- Vomiting and diarrhoea may affect protection
- Certain drugs including some enzyme inducers may affect the effectiveness
- Does not protect from STIs
Unintended pregnancy rate
- Percentage of individuals experiencing an unintended pregnancy within 1 year with typical use of POPs = 9%
Long-acting reversible contraceptives (LARCs)
LARCs are long-acting methods of contraception, avoiding the need for a daily pill or weekly patch. They are the most effective method of contraception and are convenient for patients.
Contraceptive injection
The contraceptive injection contains progestogen only and is given every 12 weeks. It is typically administered intramuscularly into the buttocks.
The systemic progestogen inhibits ovulation, thickens the cervical mucus and thins the endometrium. Depo-Provera® is one of the most commonly administered contraceptive injections.
Benefits
- Suitable for patients where oestrogen is contraindicated or those who are intolerant to oestrogen
- Do not need to remember to take a pill daily
- No interruption to intercourse
Limitations
- May cause irregular bleeding, amenorrhoea or more frequent bleeding
- The patient needs to attend clinic every 3 months and tolerate intramuscular injections
- Can affect bone mineral density if used long-term
- Does not protect from STIs
- Irreversible for the duration of the drug’s effect
- Fertility can take up to one year to return after stopping the injection
Unintended pregnancy rate
- Percentage of individuals experiencing an unintended pregnancy within 1 year with typical use of the contraceptive injection = 6%
Contraceptive implant
The contraceptive implant is a small plastic rod approximately 4cm in length inserted subdermally in the upper arm.
It slowly releases a progestogen (levonorgestrel) to prevent pregnancy. The most common brand in the UK is Nexplanon®.
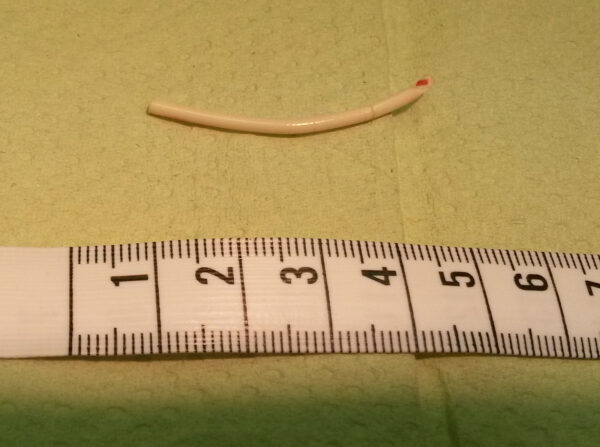
Benefits
- Once inserted, it lasts for 3 years
- Suitable for those who cannot use oestrogen
- The most effective form of contraception available (even including sterilisation)
- No interruption to intercourse
Limitations
- May cause irregular bleeding, amenorrhoea or more frequent bleeding
- Qualified practitioner required to insert the implant
- Can cause or worsen acne
- Procedure to fit and remove it, which has a risk of bruising and infection
- Does not protect from STIs
- Can be affected by enzyme inducers (e.g. carbamazepine)
Unintended pregnancy rate
- Percentage of unintended pregnancies within 1 year with typical use of the contraceptive implant = 0.05% (i.e. 1 in 2000)
Intrauterine system (IUS)
The intrauterine system (IUS) is a hormonal coil containing levonorgestrel. It is a T-shaped plastic rod with threads inserted into the uterus and releases progestogen locally. The threads remain in the vagina to allow for the removal of the coil.
An IUS prevents pregnancy by thinning the endometrium to prevent implantation and by thickening cervical mucus to prevent sperm passage.
There are several brands of IUS:
- Mirena®: used for 6 years for contraception and 5 years for the endometrial protection component of hormone replacement therapy
- Kyleena®: slightly smaller hormonal coil containing less progestogen and is also licensed for 5 years
- Jaydess®: similar size to the Kyleena® and is licensed for 3 years
The above coils are all suitable for nulliparous individuals.
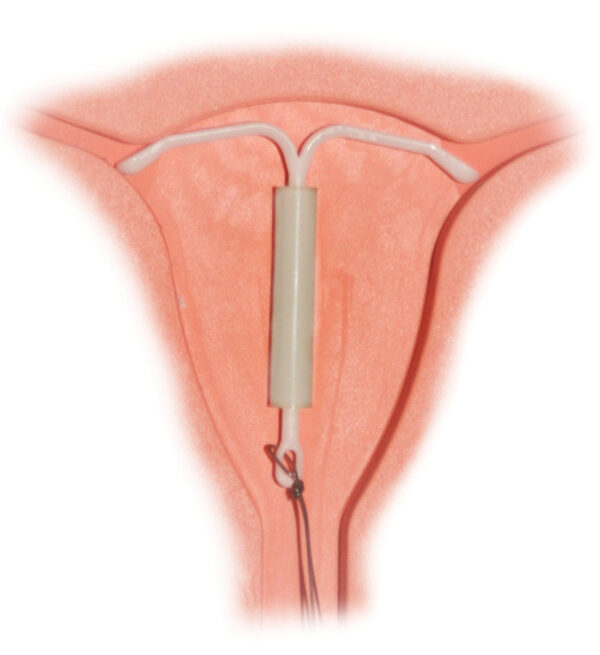
Benefits
- Lasts for 3 or 5 years
- Suitable for those who cannot take oestrogen
- Very effective in preventing pregnancy
- No interruption to intercourse
- More likely than the implant to reduce heavy menstruation (particularly the Mirena®)
- Some individuals report fewer systemic side effects as compared to the implant
Limitations
- Can make menstruation irregular, especially in the first 6 months and can cause amenorrhea (may be a benefit)
- Can cause acne, headaches and breast tenderness
- Qualified practitioner required to insert coil
- Involves a procedure with speculum exam to fit and remove the coil
- Small risk of uterine perforation and infection with insertion
- If pregnancy occurs, more likely to be an ectopic pregnancy
- Does not protect from STIs
Unintended pregnancy rate
- Percentage of individuals experiencing an unintended pregnancy within 1 year with typical use the IUS = 0.2% (i.e. 1 in 500)
Intrauterine device (‘copper coil’)
The intrauterine device (IUD), also called the copper coil, is similar to the IUS but does not contain any hormones. The rod is coated in copper, which creates an inhospitable environment for sperm and ovum to survive in the uterus.
Various different coils are available in different shapes and sizes. Copper coils generally last for either 5 or 10 years.
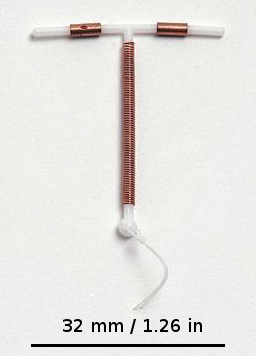
Benefits
- Lasts 5-10 years
- Non-hormonal method
- Very effective in preventing pregnancy
- No interruption to intercourse
- Effectiveness unaffected by other medications
- Can be used as emergency contraception
Limitations
- Can cause heavier, longer and more painful menstruation
- Qualified practitioner required to insert coil
- Involves a procedure with speculum exam to fit and remove the coil
- Small risk of uterine perforation and infection with insertion
- If pregnancy occurs, more likely to be an ectopic pregnancy
- Does not protect from STIs
Unintended pregnancy rate
- Percentage of individuals experiencing an unintended pregnancy within 1 year with typical use of the IUD = 0.8% (i.e. 1 in 125)
Sterilisation
Female sterilisation
Female sterilisation is performed under general anaesthetic or during a caesarean section.
It is considered irreversible when counselling patients, though it is sometimes possible to reverse the procedure surgically. Hence, it is only suitable for individuals who are certain they do not want to become pregnant in the future.
Methods of female sterilisation include:
- Tubal occlusion with surgical clips
- Salpingectomy
Benefits
- Permanent contraception
- No interruption to intercourse
- Does not affect their hormonal levels
- Effectiveness unaffected by other medications
Limitations
- Carries risks of surgery, including bleeding, infection and pain
- Very difficult to reverse (considered irreversible)
- Individuals need to be informed that, in rare cases, they can still become pregnant
- If pregnancy occurs, more likely to be an ectopic pregnancy
- Does not protect from STIs
Unintended pregnancy rate
- Percentage of individuals experiencing an unintended pregnancy within 1 year following female sterilisation = 0.5% (i.e. 1 in 200)
Male sterilisation (vasectomy)
Male sterilisation, or vasectomy, involves a procedure under local anaesthetic to remove a section of each vas deferens.
This prevents pregnancy by preventing sperm from entering the semen. Because vasectomy is considered irreversible, this procedure is only suitable for men who do not intend to have children in the future.
Benefits
- Permanent contraception
- Does not interrupt intercourse
- Less invasive and lower-risk procedure than female sterilisation
Limitations
- Carries risks of surgery, including bleeding and infection
- Some men experience pain after their surgery (post-vasectomy pain)
- Very difficult to reverse
- Contraception should be used afterwards until semen is confirmed to be sperm-free
- Does not protect from STIs
Unintended pregnancy rate
- Percentage of individuals experiencing an unintended pregnancy within 1 year following male vasectomy = 0.15% (i.e. 1 in 667)
Emergency contraception
Emergency contraception is used by individuals who have had unprotected sexual intercourse (UPSI) or contraceptive failure and wish to minimise their risk of pregnancy.
There are two main methods of emergency contraception:
- Oral emergency contraception (‘morning after pill’): Levonelle® and ellaOne®
- Insertion of an intrauterine device (copper coil)
Oral emergency contraception
Levonelle®
Levonelle contains a high dose of the synthetic progestogen levonorgestrel. It is thought to prevent pregnancy by delaying ovulation, by which time any sperm in the reproductive tract would be non-viable.
Levonelle® must be taken within 72 hours of UPSI to be effective. If taken later, after the start of the LH surge, there is no evidence of any benefit to this method of emergency contraception.
Benefits
- Can be taken if the patient has recently taken a progestogen-containing contraceptive
- Can start ongoing hormonal contraception on the same day
- Can be taken more than once in a menstrual cycle
- Unlike the copper coil, no insertion procedure is required
- Easily accessible for patients (can be bought over the counter)
- Fewer contra-indications than ellaOne®
Limitations
- The least effective form of emergency contraception
- No evidence of any benefit if taken after ovulation has occurred
- More effective at the start of the 72-hour window than at the end
- Efficacy affected by enzyme-inducing medications and by patient weight
- Does not provide any ongoing contraception
- Delays menstruation
Unintended pregnancy rate
- Effectiveness is difficult to quantify but around 1.7-2.2% of individuals who took this pill within 72 hours of UPSI became pregnant in the same cycle
ellaOne®
EllaOne®, which contains ulipristal acetate, prevents pregnancy by delaying or stopping ovulation.
It must be taken within 120 hours to be effective, and unlike Levonelle®, evidence suggests that some effectiveness remains even after the start of the LH surge (although not after ovulation itself).
Benefits
- More effective than Levonelle®, particularly if close to the ovulation date
- Unlike the copper coil, no insertion procedure is required
- Easily accessible for patients (can be bought over the counter)
- Effective up to 120 hours after UPSI, as compared to 72 hours for Levonelle®
- Effectiveness remains the same throughout the 120-hour window
- Can be used more than once in the same cycle
Limitations
- No evidence of any benefit if taken after ovulation has occurred
- Efficacy affected by enzyme-inducing medications and by patient weight
- Must wait 5 days after taking ellaOne® before starting other hormonal contraceptives; efficacy in theory reduced if hormonal contraceptives are taken within the preceding 7 days
- Not recommended in patients with severe asthma
- Does not provide any ongoing contraception
- Delays menstruation
Unintended pregnancy rate
- Effectiveness is difficult to quantify but around 1.3-1.6% of individuals who took this pill within 120 hours of UPSI became pregnant in the same cycle
Intrauterine device (copper coil)
The IUD (copper coil) is the most effective form of emergency contraception and should be offered to all patients for consideration.
The coil must be inserted within 5 days of UPSI or 5 days of ovulation, depending on the number of episodes of UPSI, when they occurred and the regularity of the individual’s cycle. More information can be found in the FSRH guidance on emergency contraception.
The IUD can be left to give long-term contraception or removed after the next period, depending on the individual’s preference.
Benefits
- The most effective form of emergency contraception
- Provides ongoing contraception for up to 10 years
- The only form of emergency contraception which is effective if fitted after ovulation
- Is not affected by patient weight or other medications
Limitations
- A qualified practitioner is required to insert the coil, which some individuals may find uncomfortable. The procedure itself carries small risks of perforation and infection.
- Less convenient than oral emergency contraception
Unintended pregnancy rate
- Effectiveness is difficult to quantify but <0.1% of individuals who had the coil inserted during the appropriate window became pregnant in the same cycle.
Summary of effectiveness
Table 1. Summary of the effectiveness of different methods of contraception. Adapted from the FSRH guidance on combined hormonal contraception.
| Method | Unintended pregnancy rate (typical use)* |
| No contraception | 85% |
| Natural family planning | 24% |
| External condoms | 18% |
| Internal condoms | 21% |
| Diaphragm | 12% |
| Combined hormonal contraception (oral, patch and ring) | 9% |
| Progestogen-only pills | 9% |
| Injection | 6% |
| Implant | 0.05% |
| Intrauterine system (IUS) | 0.2% |
| Intrauterine device (IUD) | 0.8% |
| Female sterilisation | 0.5% |
| Male sterilisation | 0.15% |
*Percentage of individuals experiencing an unintended pregnancy within 1 year with typical use using this method
Reviewers
Dr Grace Farrington
GP Trainee
Dr Ashley Jefferies
Community Sexual and Reproductive Health Registrar
Editor
Dr Chris Jefferies
References
- Percy, L., & Mansour, D. (2016). Contraception Made Easy Revised Edition. Banbury: Scion Publishing Ltd.
- NHS. Your contraception guide. 2021. Available from: [LINK]
- Collins S, Arulkumaran S, Hayes K, Jackson S, Impey L. Oxford Handbook of Obstetrics and Gynaecology. 3rd ed. Oxford: Oxford University Press; 2013.
- Faculty of Sexual and Reproductive Health [FSRH] (2019) FSRH Guideline Combined Hormonal Contraception. Available at: [LINK]
- FSRH (2019) Faculty of Sexual and Reproductive Healthcare Clinical Guidance, Progestogen-Only Pills. Available at: [LINK]
- FSRH (2019) UK Medical Eligibility Criteria for Contraceptive Use UKMEC 2016. Available at: [LINK]
- FSRH (2019) Faculty of Sexual and Reproductive Healthcare Clinical Guidance, Intrauterine Contraception. Available at: [LINK]
- FSRH (2020) FSRH Guideline: Emergency Contraception. Available at: [LINK]
Image references
- Figure 1. Flegmus. External Condom. License: [CC BY-SA]
- Figure 2. BruceBlaus. Internal Condom. License: [CC BY-SA]
- Figure 3. HiGyn.Contraceptive Diaphragm side view. License: [CC BY-SA]
- Figure 4. Sakky.Real nuvaring. License: [Public domain]
- Figure 5. Vera de Kok. Implanon. License: [CC BY-SA]
- Figure 6. Hic et nunc. Mirena IUS. License: [Public domain]
- Figure 7. LeiaWonder. IUD with scale. License: [CC BY-SA]