- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Acute coronary syndrome (ACS) is a term used to describe a sudden reduction in blood flow to the heart which may result in irreversible damage to the myocardium.
ACS can be divided into three unique clinical entities: ST-segment elevation myocardial infarction (STEMI), non-ST segment elevation myocardial infarction (NSTEMI) and unstable angina.
NSTEMIs are defined by the presence of myocardial infarction as detected by a rise in cardiac biomarkers, without ECG changes indicative of a STEMI.1
In 2018/2019 there were 87,091 cases of myocardial infarction reported in the UK with 64% of these being NSTEMIs.2
Differentiating between a STEMI, NSTEMI and unstable angina has important implications for management.
Aetiology
Broadly speaking, ACS is caused by a mismatch between myocardial oxygen demand and myocardial oxygen delivery.
In a STEMI, the mismatch between myocardial oxygen demand and delivery is almost always caused by total occlusion of a coronary artery from atherosclerotic plaque rupture and subsequent thrombus formation. The severity is dependent on the size, location, and duration of the occlusion.
In NSTEMIs however, there are more varied causes of mismatch including partial coronary artery obstruction from a ruptured plaque (most common), partial occlusion from a stable plaque, coronary artery vasospasm (Prinzmetal’s angina) or coronary arteritis.
In some cases, myocardial supply and demand mismatch may be caused by conditions that only indirectly affect the coronary arteries (e.g. severe anaemia, hypotension, tachycardia, aortic stenosis, and pulmonary embolism).
In these situations, revascularisation strategies are unnecessary and the underlying cause should be addressed. These are known as ‘type 2’ myocardial infarctions and often do not present with chest pain, their classification as NSTEMIs is controversial.
Risk factors
Risk factors for ACS include any factors which increase the risk of coronary artery atherosclerosis.
Non-modifiable risk factors include:
- Male sex
- Older age
- Previous history of ACS/ischaemic heart disease
- Family history of ACS/ischaemia heart disease
- Renal insufficiency
- Diabetes
Modifiable risk factors include:
- Tobacco smoking
- Longstanding hypertension
- Hyperlipidaemia
Clinical features
History
Initial assessment of anyone with acute chest pain involves a thorough history. See the Geeky Medics OSCE guide to a comprehensive chest pain history.
The history should assess the acute presentation and features of ACS and include an assessment of cardiovascular risk factors.
Typical symptoms of ACS/NSTEMI include:
- Sudden onset central crushing chest pain radiating to the left arm and/or jaw lasting longer than 20 minutes (if pain-free, identify when their last episode of pain occurred)
- Diaphoresis
- Nausea
- Shortness of breath
Other important areas to cover in the history include:
- Assessment of cardiovascular risk factors: hypertension, hyperlipidaemia, diabetes, smoking and family history
- Assessment of differential diagnoses: risk factors and symptoms of venous thromboembolism, musculoskeletal, respiratory and gastrointestinal symptoms.
Clinical examination
All patients with suspected ACS require a comprehensive cardiovascular examination. However, examination findings can be non-specific in an NSTEMI.
A combination of thorough chest pain history, 12-lead ECG and high sensitivity troponin is the gold standard for diagnosis.
Although a physical examination is necessary to look for complications of ACS and to assess clinical stability, it should not delay initial investigations and management.
Typical clinical findings of ACS/NSTEMI include:
- Signs of respiratory distress, pallor, diaphoresis, or fluid overload
- Tachycardia
- High or low blood pressure
- S4 heart sound: due to reduced ATP production impairing left ventricular relaxation
- Signs of papillary muscle dysfunction (e.g. mitral regurgitation)
- Pulmonary oedema: due to acute left-sided heart failure
Differential diagnoses
Chest pain has a wide range of differential diagnoses. See the Geeky Medics guide to chest pain history for more information on the typical clinical features of each differential diagnosis.
Despite the high sensitivity of ST-segment deviation and raised troponins for acute thrombotic cardiac events, these markers are not always specific.
Troponin is a good indicator for myocardial damage but is not always due to myocardial ischaemia.
Several other pathologies may cause myocardial damage in the absence of coronary artery pathology and thus present with raised serum troponin and ECG changes. These include:
- Myocarditis
- Pericarditis
- Pulmonary embolism
- Aortic dissection
- Acute heart failure
- Arrhythmias
- Sepsis
- Cardiotoxic agents
It is important that these conditions are identified and treated to prevent further myocardial damage.
Investigations
12-lead ECG
Serial 12-lead ECGs are important for assessing and monitoring patients with suspected ACS. A record of the patient’s baseline ECG may be helpful in determining the presence of acute changes.
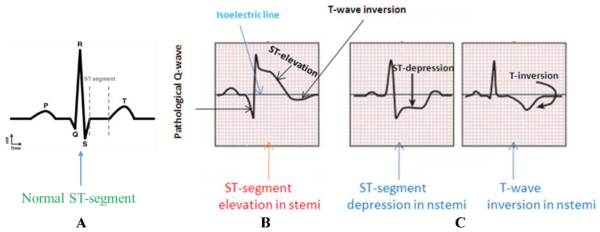
The presence of raised serum troponins in the absence of the following features indicates a diagnosis of an NSTEMI:
- Persistent ST-segment elevation
- Evidence of a posterior MI
- New left bundle branch block
Typical ECG findings of an NSTEMI include:3
- Regional ST-segment depression
- T wave inversion or flattening
- Any dynamic or new Q or T wave changes
See the Geeky Medics guides to ECG interpretation for more information.
Troponin
High sensitivity troponin I or T are the recommended tests for suspected ACS.
Troponin is a structural protein which is found solely in cardiac myocytes. The presence of troponin within the blood indicates myocardial necrosis.
When necrosis occurs, cardiomyocyte’s membranes rupture, releasing intracellular enzymes including troponin into the bloodstream.5
To be indicative of myocardial damage, troponin levels need to be about three standard deviations from the normal range.
Typically, serial troponin tests are required in order to see the trend of troponin over time.
In an NSTEMI, the troponin is expected to rise two to three hours after the onset of chest pain, peaking 12-48 hours post the incident and declining for the next 4-10 days.5
It is, therefore, possible for someone to present to hospital with symptoms of ACS and have a normal troponin and ECG initially, but still be having an NSTEMI.
A second troponin 30 minutes to three hours after initial presentation is typically required to exclude an NSTEMI in patients at high risk of ACS.
Laboratory investigations
Other relevant laboratory investigations include:
- U&Es: renal function may affect treatment options. Chronic kidney disease (CKD) can lead to raised troponin and non-coronary artery related myocardial damage. In addition, CKD is a risk factor for coronary artery disease.
- Glucose: hyperglycaemia should be tested for and managed during ACS as hyperglycaemia has been associated with poorer outcomes.6
- FBC: underlying anaemia may exacerbate ACS or be indicative of an occult bleed.
Other investigations
Coronary angiography is important in high to moderate risk groups to identify the presence and location of coronary artery vasculature blockage.
An echocardiogram is useful to assess left ventricular function in patients with both suspected and confirmed ACS.
Chest X-ray may be useful to rule out other potential causes of chest pain (e.g. pneumothorax, pneumonia).
Diagnosis
The diagnosis of NSTEMI is made from the combination of clinical history, abnormal troponins, and the absence of ST-elevation on ECG.
Management
The following sections are in accordance with the 2020 NICE guidelines for the management of acute coronary syndromes.7
Immediate management
ACS is an emergency situation and an initial ABCDE approach should be taken. See the Geeky Medics guide to the acute management of ACS for more information.
Immediate management of ACS includes:
- Antiplatelet therapy: aspirin 300mg
- Analgesia: either GTN or intravenous opioids
- Initial anti-thrombin therapy: fondaparinux if low bleeding risk and the patient is not undergoing immediate angiography. Unfractionated heparin can be used for patients with renal impairment.
- Supplemental oxygen should be offered only to patients with SpO2 of less than 94%.
Coronary angiography
Coronary angiography is an invasive procedure which utilises intravenous contrast and X-ray imaging to assess coronary artery patency.
Percutaneous coronary intervention (PCI) involves a thin guide wire being placed in the affected coronary artery and the inflation of a balloon to achieve patency at the location of the blockage.
A stent is placed around the balloon prior to insertion and will remain in the affected artery post-procedure to keep the artery patent.
Coronary angiography is required for all clinically unstable adult patients diagnosed with NSTEMI as soon as possible and at least within 24 hours of becoming clinically unstable.
Clinically unstable patients are defined by the following clinical features:
- Ongoing or recurring pain despite treatment
- Haemodynamic instability (low blood pressure, shock)
- Dynamic ECG changes
- Left ventricular failure
Risk stratification
After the diagnosis of NSTEMI has been confirmed and initial pharmacological treatment offered, formal risk stratification using an established scoring system is recommended.
Categorisation based on 6-month mortality of patients diagnosed with unstable angina or NSTEMI aids in providing appropriate short-term interventions and treatment.
The Global Registry of Acute Cardiac Events (GRACE) scale predicts 6-month mortality for patients admitted with ACS.
Low risk (predicted 6-month mortality <3%)
For patients who are assessed as low risk, consider conservative management without coronary angiography. However, younger patients may benefit from coronary angiography and PCI.
Offer dual antiplatelet therapy:
- Ticagrelor if bleeding risk not high
- Clopidogrel or aspirin only if high bleeding risk
In low-risk patients, consider ischaemia testing before discharge. If ischaemia is present on testing, consider coronary angiography and possible PCI.
Left ventricular function should be assessed prior to discharge.
High or moderate risk (predicted 6-month mortality >3%)
If no contraindications, high or moderate risk patients should be offered coronary angiography within 72 hours, with subsequent PCI if required.
Patients undergoing coronary angiography should be offered dual antiplatelet therapy with either prasugrel or ticagrelor. Clopidogrel can be used if a patient is receiving ongoing anticoagulation for another indication.
If undergoing PCI, patients should be offered fractionated heparin.
Left ventricular function should be assessed prior to discharge.
Long term management
Long term management of ACS is essentially the same for STEMI and NSTEMIs.
All patients with a diagnosis of NSTEMI, regardless of their risk stratification, require long term management and prevention strategies.
Drug therapy
The following drug regime is recommended for all patients post NSTEMI and STEMI to reduce the risk of future ACS (secondary prevention) and improve myocardial function:
- ACE inhibitor or ARB: continued indefinitely
- Dual antiplatelet therapy (aspirin plus a second agent): for up to 12 months
- Beta-blocker for at least 12 months: continued indefinitely in the presence of reduced left ventricular ejection fraction
- Statin: continued indefinitely
Lifestyle
Lifestyle changes and education are important in reducing the risk of a subsequent cardiovascular event. Advice should include:
- Eating a Mediterranean diet and increasing fruit and vegetable intake
- Regular physical activity: 20-30 minutes a day
- Low-risk drinking: no more than 14 units a week
- Smoking cessation
- Maintaining a healthy body weight
Cardiac rehabilitation
Cardiac rehabilitation should be offered to all patients with an NSTEMI, ideally before hospital discharge.
These programs involve:
- Advice on lifestyle, driving, flying and sex
- Tailored physical activity
- Stress management
- Health and lifestyle education
Complications
Mechanical complications such as papillary muscle rupture, ventricular aneurysm and free wall rupture are rare post-NSTEMI.8
Non-mechanical complications include arrhythmias, thromboembolic complications, heart failure, pericarditis, and depression.
Though all-cause mortality is higher for STEMI patients vs NSTEMI patients during the initial hospital presentation, there is evidence that of those surviving hospital discharge, NSTEMIs patients have a worse long-term prognosis.
In 2013, the 180-day all-cause mortality was 7.6%. for cases hospitalised with NSTEMI in the UK.9
Key points
- NSTEMIs are a type of acute coronary syndrome and are defined by the presence of myocardial infarction as detected by a rise in cardiac biomarkers, without ECG changes indicative of a STEMI.
- Acute coronary syndrome is caused by a mismatch between myocardial oxygen demand and myocardial oxygen delivery.
- NSTEMIs typically present like other acute coronary syndromes with chest pain or tightness, shortness of breath, nausea, and diaphoresis.
- 12-lead ECG and serum troponins are important initial investigation for the diagnosis of NSTEMI. NSTEMIs are characterised by the absence of STEMI defining ECG changes.
- Management is based on clinical stability and risk stratification but typically involves anti-platelet therapy, with or without invasive strategies such as coronary angiography and percutaneous coronary intervention.
- Secondary prevention measures (pharmacological and lifestyle modification) are important to reduce the future risk of further cardiovascular events.
- Complications of NSTEMIs include heart failure, arrhythmias, pericarditis, thromboembolic events, depression, and rarely mechanical complications such as ventricular aneurysms.
Reviewers
Dr Nicholas Taylor
Emergency Medicine physician with an interest in acute cardiology
Associate Dean Phase 2 at the ANU Medical School
Dr Simon O’Connor
Cardiologist
Clinical Senior Lecturer at the ANU Medical School
Editor
Dr Chris Jefferies
References
- Basit H, Malik A, Huecker MR. Non ST Segment Elevation Myocardial Infarction. Published January 2020, Available from: [LINK]
- NICOR, Myocardial Ischemia National Audit Project, published 10th December 2020, available from: [LINK]
- Life in the fast lane, Myocardial Ischemia, published 16th December 2020, available from: [LINK]
- Chowdhury MEH, Alzoubi K, Khandakar A, Khallifa R, Abouhasera R, Koubaa S, Ahmed R, Hasan A. Comparison of ECG changes in STEMI and NSTEMIs. License: [CC-BY]. Available from: [LINK]
- Stark M, Kerndt CC, Sharma S. Published July 10th 2020, Available from: [LINK]
- Ishihara M. Acute hyperglycemia in patients with acute myocardial infarction. Circ J. 2012;76(3):563-571. doi:10.1253/circj.cj-11-1376
- NICE, Acute coronary syndromes, published: 18th November 2020, available from: [LINK]
- Elbadawi A, Elgendy IY, Mahmoud K, et al. Temporal Trends and Outcomes of Mechanical Complications in Patients With Acute Myocardial Infarction. Published September 23rd 2019, available from: [LINK]
- Gale C. Acute coronary syndrome in adults: scope of the problem in the UK, Br J Cardiol 2017;24(suppl 1):S3–S9, published: September 2017, available from: [LINK]