- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Oral cavity examination occasionally appears in OSCEs and you’ll be expected to identify relevant signs using your clinical examination skills. This guide provides a step-by-step approach to performing an examination of the oral cavity in an OSCE setting.
Gather equipment
- Headtorch or pen torch
- Tongue depressors (x2)
Introduction
Wash your hands and don PPE if appropriate.
Introduce yourself to the patient including your name and role.
Confirm the patient’s name and date of birth.
Briefly explain what the examination will involve using patient-friendly language.
Gain consent to proceed with the examination.
Ask the patient to sit on a chair.
If the patient has any dentures or implants, ask them to remove them for the assessment.
Check if the patient currently has any pain before proceeding with the clinical examination.
General inspection
Inspect the patient’s face for swelling:
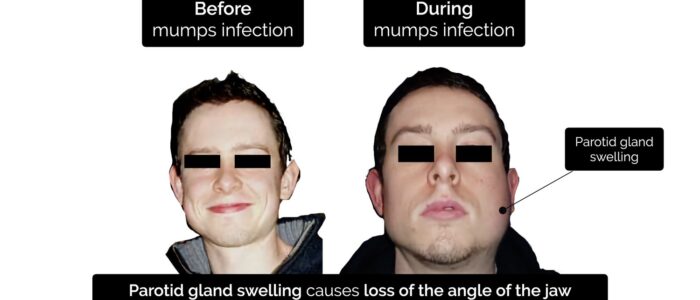
- Parotid gland swelling: causes loss of the angle of the jaw and a hamster-like appearance of the cheek on the affected side.
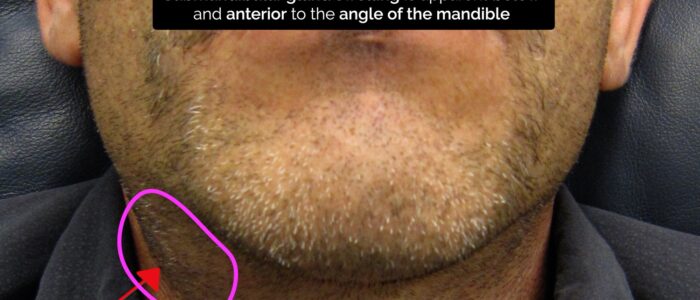
- Submandibular gland swelling: apparent below and anterior to the angle of the mandible.
Closer inspection
Ask the patient to open their mouth and inspect the oral cavity using your light source. Note if the patient has difficulty opening their mouth due to pain, suggesting the presence of trismus.
Lips
With the patient’s mouth open, use your light source to inspect the lips for abnormalities such as:
- Angular stomatitis: a common inflammatory condition affecting the corners of the mouth. It has a wide range of causes, including iron deficiency (e.g. gastrointestinal malignancy, malabsorption).
- Hyperpigmented macules: pathognomonic for Peutz-Jeghers syndrome, an autosomal dominant genetic disorder that results in the development of polyps in the gastrointestinal tract.
- Ulceration: may be secondary to trauma, infections (e.g. herpes simplex) or rarely malignancy.
Tongue
Ask the patient to stick out their tongue and inspect for abnormalities such as:
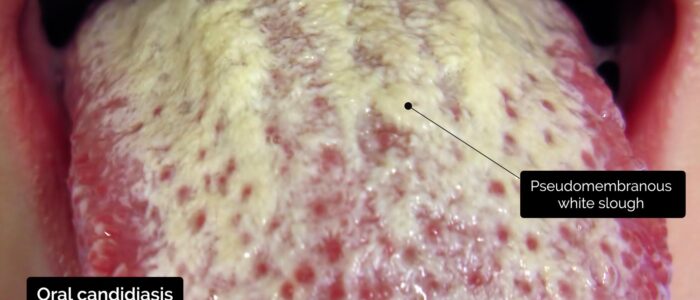
- Oral candidiasis: a fungal infection commonly associated with immunosuppression. It is characterised by pseudomembranous white slough which can be easily wiped away to reveal underlying erythematous mucosa.
- Glossitis: smooth erythematous enlargement of the tongue associated with iron, B12 and folate deficiency (e.g. malabsorption secondary to inflammatory bowel disease).
- Ulceration: may be secondary to trauma, infections (e.g. herpes simplex) or rarely malignancy.
- Hairy leukoplakia: a white patch on the side of the tongue with a hairy appearance associated with Epstein-Barr virus infection in immunocompromised patients.
Teeth and gums
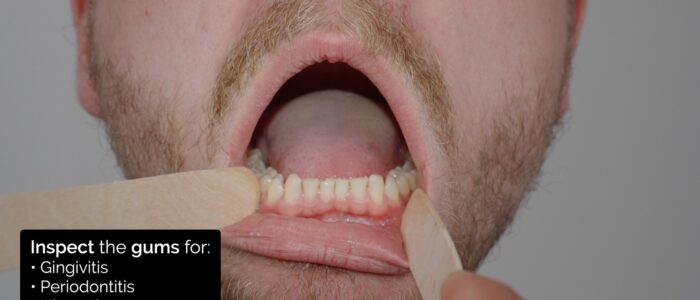
Using two tongue depressors inspect the teeth and gums.
Teeth
Inspect the teeth for abnormalities:
- Missing teeth: may be secondary to infection or trauma.
- Nicotine staining: present in patients who smoke (a significant risk factor for oral malignancy).
- Tooth decay: indicative of poor oral hygiene.
Gums
Inspect the gums for abnormalities:
- Gingivitis: inflammation of the gums that has a variety of causes include excess plaque, vitamin C deficiency, HIV and leukaemia.
- Periodontitis: can develop if gingivitis is left untreated and involves inflammation of the periodontal ligament. The condition can ultimately lead to the formation of peridontal abscesses and tooth loss.
- Ulceration: may be secondary to trauma, infections (e.g. herpes simplex) or rarely malignancy.
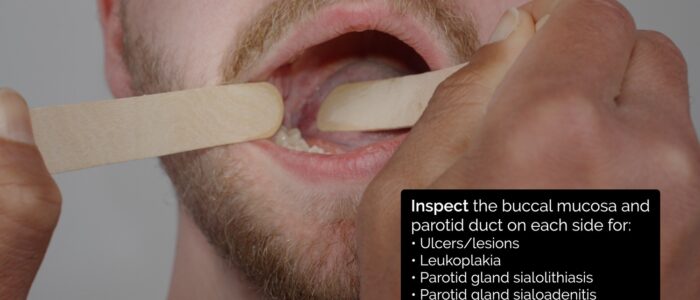
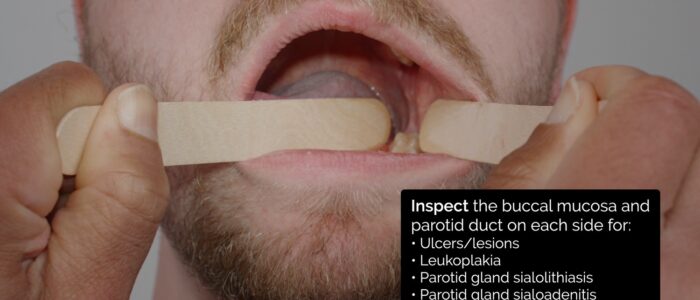
Buccal mucosa and parotid duct
Using one tongue depressor move the tongue to either side and inspect the buccal mucosa and parotid duct.
Buccal mucosa
Inspect the buccal mucosa for abnormalities:
- Aphthous ulcers: benign, non-contagious, erythematous, painful small, round oral ulcers with circumscribed margins. Their aetiology is unclear and likely multifactorial.
- Other ulcers: if an ulcer has been present for more than 7-10 days, malignancy should be considered.
- Leukoplakia: non-painful white patch or plaque on the oral mucosa. Leukoplakia can undergo malignant transformation and is strongly associated with smoking.
Parotid duct
Inspect the parotid duct for abnormalities:
- Parotid gland sialolithiasis: a calcified stone blocking excretion of the parotid gland resulting in swelling and increased prominence of the duct.
- Parotid gland sialoadenitis: infection of the parotid gland, typically secondary to sialolithiasis but other causes include viral infections (e.g. mumps). There may be erythema around the duct and visible discharge.
- Pleomorphic adenoma: the most common type of tumour affecting the parotid gland. Typical presenting features include a solitary, slow-growing, painless, firm single nodular mass.
Parotid gland
The parotid glands are the largest salivary glands and are located posterolaterally to the mandibular ramus (bilaterally). On each side of the face, the parotid duct pierces the buccinator muscle and opens into the oral cavity through the buccal mucosa, opposite the maxillary second molar.
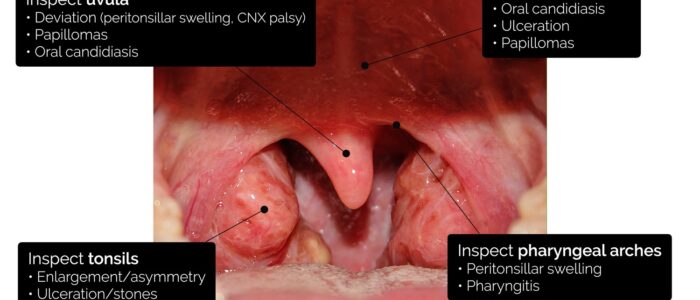
Back of the mouth
Ask the patient to relax their tongue and cheeks to remove muscular tension.
Using one tongue depressor, gently depress the tongue and inspect the back of the mouth.
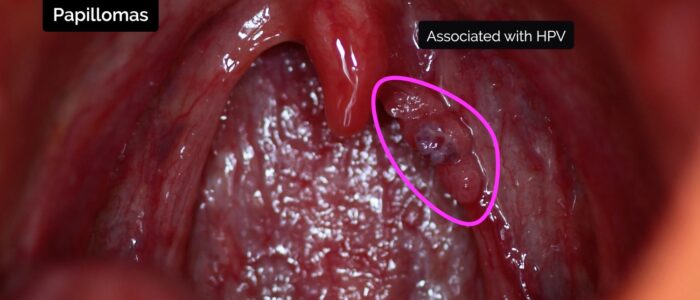
Palate and uvula
Inspect the palate and uvula for abnormalities such as:
- Oral candidiasis: a fungal infection commonly associated with immunosuppression. It is characterised by pseudomembranous white slough which can be easily wiped away to reveal underlying erythematous mucosa.
- Ulceration: may be secondary to trauma, infections (e.g. herpes simplex) or rarely malignancy.
- Papillomas: tumours derived from epithelium, that appear as cauliflower-like projections arising from the surface of the palate and uvula. They are associated with human papillomavirus (HPV) infection.
Palate and uvula anatomy
The palate forms the roof of the mouth and separates the nasal cavity from the oral cavity. It can be further sub-divided into the:
- Hard palate: the immobile portion of the palate comprised of bone.
- Soft palate: the mobile portion of the palate comprised of muscle fibres covered by a mucous membrane. The soft palate elevates during swallowing to prevent a food bolus from entering the nasopharynx.
The uvula is a fleshy extension that projects from the back edge of the soft palate. In healthy individuals, it should be positioned in the midline of the palate.
Tonsils, pharyngeal arches and uvula
Inspect the tonsils for abnormalities:
- Enlargement: most often due to infection (tonsilitis), in which case there is also erythema and often exudate. Tonsillar enlargement may also be a chronic condition (e.g. tonsillar hypertrophy).
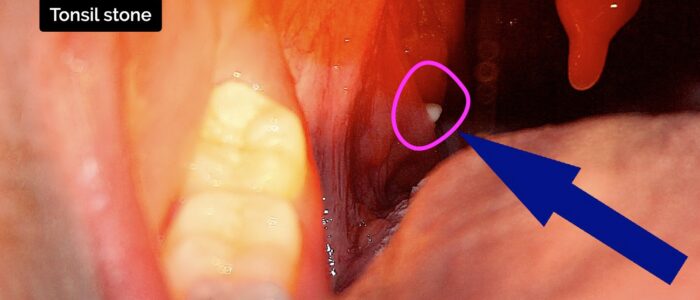
- Asymmetry: tonsilitis can cause asymmetrical tonsillar swelling, however other causes of unilateral tonsillar swelling include tonsillar stones and malignancy.
- Tonsillar ulceration: may be caused by viral infections (e.g. herpes simplex), however, malignancy should also be considered.
- Tonsillar stones: caused by mineralisation of debris trapped within the tonsils. The stones may be visible on inspection of the tonsils and are usually asymptomatic.
Inspect the pharyngeal arches for abnormalities:
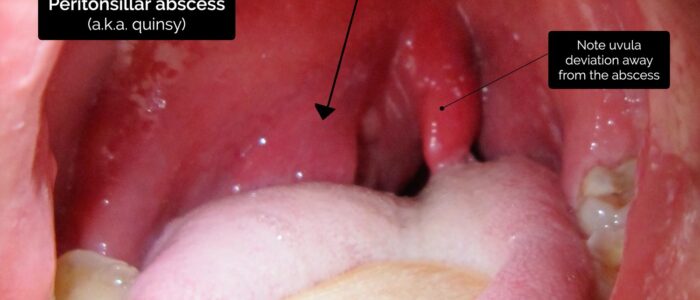
- Peritonsillar swelling: typically caused by a peritonsillar abscess (quinsy), in which pus is trapped between the tonsillar capsule and the lateral pharyngeal wall.
- Pharyngitis: inflammation of the pharynx with several potential causes, including viral and bacterial infections.
Inspect the uvula for abnormalities:
- Uvula deviation: may be caused by a peritonsillar abscess, with the uvula deviating away from the abscess. A vagus nerve lesion can also cause uvula deviation away from the side of the lesion. If there are no other symptoms or signs, uvula deviation is likely a normal finding.
Tonsilar anatomy
The palatine tonsils are located at the right and left sides of the back of the throat between the palatoglossal and palatopharyngeal arches of the soft palate. The palatoglossal arch is also known as the anterior tonsillar pillar and the palatopharyngeal arch is also known as the posterior tonsillar pillar. The tonsils appear as pinkish lumps and play an important role in immunity.
Floor of the mouth
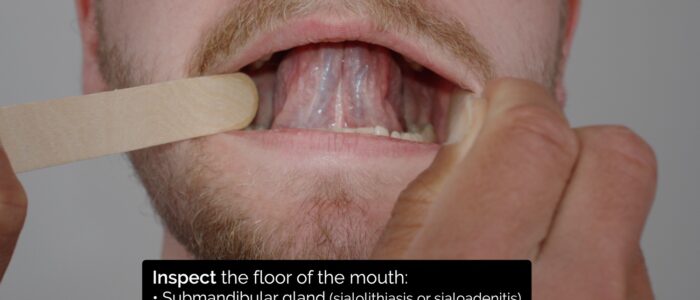
Ask the patient to lift their tongue to the roof of their mouth and assess the floor of the mouth for pathology such as:
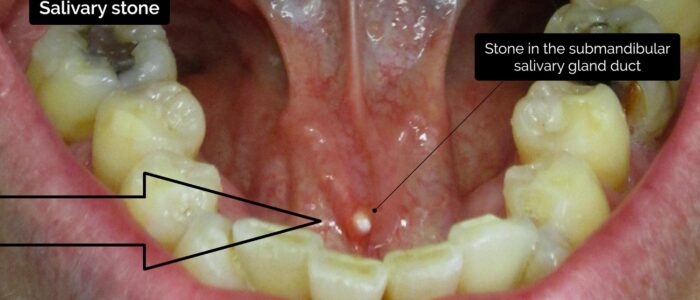
- Submandibular gland sialolithiasis: a calcified stone blocking excretion of the submandibular gland resulting in swelling and increased prominence of the duct. There may be erythema around the duct and visible discharge.
- Submandibular gland sialoadenitis: infection of the submandibular gland, typically secondary to sialolithiasis but other causes include viral infections (e.g. mumps). There may be erythema around the duct and visible discharge.
- Ulceration: may be secondary to trauma, infections (e.g. herpes simplex) or rarely malignancy.
Submandibular and sublingual glands
The paired submandibular glands are located on the floor of the mouth and are responsible for producing saliva. These glands are responsible for the majority of salivary duct calculi, possibly due to the torturous uphill course of the submandibular gland’s duct. The submandibular gland’s ducts open out on either side of the lingual frenulum as small prominences known as sublingual caruncles.
The paired sublingual glands are also located on the floor of the mouth, behind the mandibular canines, and are responsible for producing saliva. The glands are drained by 8-20 ducts known as the ducts of Rivinus. The largest sublingual duct joins the submandibular duct to drain through the same sublingual caruncle. The rest of the ducts open into the mouth on an elevated region of mucous membrane known as the plica sublingualis.
Palpation
If permitted by the patient and examiner, proceed to bimanual palpation of the mouth.
Don some non-sterile gloves (if not already wearing some).
Bimanual palpation of the mouth
1. With one finger palpating the neck externally and the other gloved finger in the oral cavity, gently palpate any identified lumps from both sides.
2. Palpate the lateral walls of the mouth to assess the parotid gland and duct.
3. Palpate the floor of the mouth to assess the submandibular gland and sublingual gland.
Any intraoral swelling should be described according to its site, size, thickness, colour, texture, consistency and tenderness.
To complete the examination…
Explain to the patient that the examination is now finished.
Thank the patient for their time.
Dispose of PPE appropriately and wash your hands.
Summarise your findings.
Example summary
“Today I performed an examination of the oral cavity on Mr Smith, a 30-year-old male who presented with a submandibular swelling.”
“On inspection, dentition was normal and a small, erythematous swelling was noted on the floor of the mouth, beside the lingual frenulum. On bimanual palpation, the lump was hard and non-tender. These findings are consistent with a salivary duct stone.”
“For completeness, I would like to perform the following further assessments and investigations.”
Further assessments and investigations
- Examination of the neck, ears and temporomandibular joint.
- Flexible nasal endoscopy: to visualise the oropharynx.
- Orthopantomogram: to further assess dental pathology.
- Ultrasound neck +/- fine-needle aspiration: to assess neck or salivary gland lumps (if required).
- CT and MRI: to image the oral cavity and neck +/- chest if cancer is suspected (according to local guidelines)
Reviewer
Mr Ben Cosway
ENT Consultant
References
- Blausen.com staff (2014). WikiJournal of Medicine. Adapted by Geeky Medics. Anatomy of the oral cavity. Licence: CC BY 3.0.
- James Heilman, MD. Adapted by Geeky Medics. Submandibular gland. Licence: CC BY-SA.
- n.raveender. Adapted by Geeky Medics. Parotid tumour.
- Yeanold Viskersenn. Adapted by Geeky Medics. Mumps. Licence: CC BY-SA.
- Adapted by Geeky Medics. Matthew Ferguson. Angular stomatitis. Licence: CC BY-SA.
- Adapted by Geeky Medics. Abdullah Sarhan. Peutz-Jager syndrome. Licence: CC BY-SA.
- Adapted by Geeky Medics. James Heilman, MD. Oral candidiasis. Licence: CC BY-SA.
- Adapted by Geeky Medics. Klaus D. Peter, Gummersbach. Glossitis. Licence: Klaus D. Peter, Gummersbach, Germany. Licence: CC BY 3.0 DE.
- Aitor. Adapted by Geeky Medics. Leukoplakia.
- Onetimeuseaccount. Adapted by Geeky Medics. Gingivitis. Licence: CC BY-SA.
- DRosenbach. Adapted by Geeky Medics. Stenson’s duct. Licence: CC BY-SA.
- Ryanfransen. Adapted by Geeky Medics. Aphthous ulcer.
- GalliasM. Adapted by Geeky Medics. HPV warts in the throat. Licence: CC BY-SA.
- Klem. Adapted by Geeky Medics. Oral cavity anatomy. Licence: CC BY.
- Dake. Adapted by Geeky Medics. Pharyngitis. Licence: CC BY-SA.
- Michaelbladon. Adapted by Geeky Medics. Tonsillitis.
- James Heilman, MD. Adapted by Geeky Medics. Peritonsillar abscess. Licence: CC BY-SA.
- Phreezinc. Adapted by Geeky Medics. Tonsil stone.
- James Heilman, MD. Adapted by Geeky Medics. Salivary stone. Licence: CC BY-SA.