- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Orbital and peri-orbital cellulitis reflect a spectrum of disease which are differentiated by the anatomy of the orbital septum.
Peri-orbital cellulitis refers to infection occurring anterior to the orbital septum (pre-septal) and orbital cellulitis refers to infection occurring posterior to the orbital septum (post-septal).
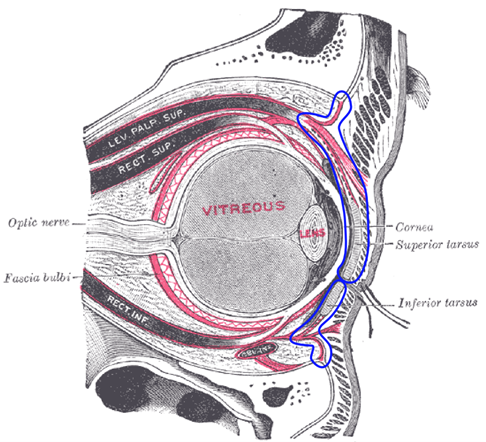
The orbital septum is a membranous sheet that forms the anterior boundary of the orbit and separates the pre-septal and post-septal spaces (Figure 1). The septum acts as a barrier to infection. It originates both superiorly and inferiorly from the orbital periosteum. Superiorly, it is continuous with levator palpebrae superioris. Inferiorly, it is continuous with the inferior tarsal plate.1
Orbital cellulitis
Orbital cellulitis involves infection of the muscle and fat within the orbit, posterior to the orbital septum.
It is more common in children, with the incidence reported to be 16-fold higher in children compared to adults.3
Differentiation between peri-orbital and orbital cellulitis can be difficult in the initial stages of infection.
Orbital cellulitis is a serious sight-threatening condition. Approximately 11% of patients will have visual loss following orbital cellulitis.4
Aetiology
Orbital cellulitis is commonly caused by a local spreading infection from acute bacterial sinusitis, typically from the paranasal sinuses.
Less common causes of orbital cellulitis include the extension of peri-orbital cellulitis, haematogenous spread, orbit trauma (e.g. dog bite), or contiguous spread from the face or teeth from recent surgery or dental infection.5
Clinical features
History
Typical symptoms of orbital cellulitis include:
- Erythema and swelling around the eye
- Blurred vision
- Painful eye movements
- Change in colour vision
- Fever
Other important areas to cover in the history include:
- Past medical history: previous episodes of eye disease including any previous episodes of peri-orbital/orbital cellulitis
- History of precipitating cause: for example orbital trauma, sinusitis, or dental infection
- Duration of symptoms
- Laterality (unilateral or bilateral)
- Severity of symptoms (worsening, stable or improvement in symptoms since start)
Clinical examination
In the context of suspected orbital cellulitis, the following clinical examinations should be performed:6
- Nasal examination: looking for ipsilateral nasal discharge/mucus
- Oral cavity examination: assessing oral hygiene, any evidence of dental disease, and any recent dental treatment of the upper molars
- Examination of the eyes and vision: including assessment of visual fields, visual acuity, colour vision, relevant afferent pupillary defect (RAPD), light reflexes, proptosis measurement of intraocular pressure and slit lamp examination.
- Neurological examination: cranial nerve examination including assessment for meningism
Typical clinical findings in orbital cellulitis include:
- Severe eye redness and swelling
- Fever
- Painful eye movements*
- Reduced visual acuity and/or visual fields *
- Proptosis *
- Relevant afferent pupillary defect (RAPD): Marcus-Gunn pupil *
- Chemosis *
- Altered colour vision *(red-green tends to be the first colours lost)
Bilateral eye signs may indicate cavernous sinus thrombosis. Nausea, vomiting, headache, neck stiffness may indicate intracranial involvement.
* The clinical findings marked with an asterisk are red flag features and should prompt clinicians to consider severe post-septal disease. These ‘grave eye signs’ are positive predictors of advanced disease, which includes abscess formation and cavernous sinus thrombosis.8
These patients will need cross-sectional imaging and multidisciplinary involvement.

Investigations
Laboratory investigations
Relevant laboratory investigations include:
- Full blood count: may show elevated white cell count, particularly neutrophilia
- C-reactive protein (CRP): may be elevated
- Lactate: may be raised if the patient is septic
- Blood cultures: the most common isolated organisms include Staphylococcus, Streptomyces species and Haemophilus
- Microscopy, culture and sensitivity swabs: including swabs of the conjunctiva and nasopharynx
Imaging
Contrast-enhanced CT orbit, sinuses and brain is the imaging modality of choice.
Imaging is required to assess for complications of orbital cellulitis (including abscess formation or intracranial involvement) and to guide ongoing management.
Imaging is indicated if clinical examination of the eye is not possible, there are any red flag eye signs, or there is a failure to improve (e.g. ongoing pyrexia) after 36-48 hours of intravenous antibiotics.9
MR venogram may be required to aid the diagnosis of cavernous sinus thrombosis. If meningeal signs develop, lumbar puncture is indicated. A CT head should be considered to exclude raised intracranial pressure prior to lumbar puncture.
Management
Patients with suspected orbital cellulitis require emergency referral to ophthalmology and ENT.10
Medical management
Patients with orbital cellulitis require intravenous antibiotics, for seven to ten days. Antibiotic choice depends on local guidelines and results from microbiological investigations.
The patient will require multidisciplinary care (ophthalmology, ENT and paediatrics) and re-imaging if necessary.
Surgical management
If an orbital collection is seen on imaging, evacuation of orbital pus or drainage of paranasal sinus pus may be required.
Chandlers classification
Chandler’s classification anatomically categorises orbital complications of acute rhinosinusitis (the most common cause of orbital cellulitis).
Although this is not a continuum of disease it is useful in diagnosis (especially as the difference in signs can be subtle). It also provides a useful aid in guiding management of peri-orbital and orbital cellulitis.11
- Group 1: Pre-septal cellulitis (infection anterior to orbital septum)
- Group 2: Orbital cellulitis (infection posterior to orbital septum)
- Group 3: Subperiosteal abscess (pus collection between bone and periosteum)
- Group 4: Intraorbital abscess (pus collection within the orbit)
- Group 5: Cavernous sinus thrombosis (mural thrombus which may propagate centrally)
Broadly speaking, grade 1 can be treated medically with antibiotics. Grade 2 can also be treated medically however if there is no improvement surgical drainage should be considered. Grade 3 and 4 can be treated surgically (drainage endoscopically or externally). Grade 5 should be treated with anticoagulation as well as surgical drainage.
Complications
Complications of orbital cellulitis include:12
- Cavernous sinus thrombosis
- Loss of vision
- Intracerebral abscess
- Meningitis
- Death (rarely)
Key points
- Orbital cellulitis is a sight-threatening infection in the muscle and fat within the orbit, posterior to the orbital septum.
- Orbital cellulitis is commonly caused by contiguous spread of paranasal sinusitis.
- Clinical features include a painful red eye with proptosis, chemosis, painful eye movements, and decreased acuity.
- Initial investigations include an endonasal swab and FBC, CRP, and lactate. Imaging may include CT orbit, sinuses and brain.
- Medical management includes treatment with intravenous antibiotics, with surgery reserved for more complicated orbital cellulitis.
- If not recognised and treated promptly there is a risk of visual loss, intracranial spread and rarely death.
Peri-orbital cellulitis
Peri-orbital cellulitis (also called pre-septal cellulitis) is an infection in the eyelid tissues anterior to the orbital septum.
Peri-orbital cellulitis is a much more common and less serious than orbital cellulitis.13
Aetiology
Peri-orbital cellulitis is usually caused by superficial injury (e.g. insect bite, chalazion, conjunctivitis) or it can be secondary to upper respiratory tract infections or sinusitis.14
Clinical features
History
Typical symptoms of peri-orbital cellulitis include:
- Pain, redness and swelling of the eyelid
Other important areas to cover in the history include:
- Recent insect bites, styes/chalazions, recent upper respiratory tract infections
Clinical features
A thorough clinical examination is required to exclude orbital cellulitis and red flag features. See the orbital cellulitis section for the examinations that should be performed.
Typical clinical features of peri-orbital cellulitis include:
- Eyelid redness, mild tenderness and swelling
- Fever
Unlike orbital cellulitis, patients with peri-orbital cellulitis are unlikely to experience significant pain.
Visual acuity and visual fields are normal, and there is no pain on eye movement. The patients colour vision will be intact and there will be no sign of chemosis or proptosis. A fever may or may not be present in peri-orbital cellulitis.
Patients with peri-orbital cellulitis are systemically well and symptoms are less severe. If there is severe eyelid swelling it may be difficult to rule out underlying orbital involvement and imaging may be required.
Table 1. Differentiating between orbital and peri-orbital cellulitis.
|
|
Peri-orbital cellulitis | Orbital cellulitis |
|
Proptosis |
No |
Yes |
|
Eye movements |
Normal |
Painful and restricted |
|
Visual acuity |
Normal |
May be reduced |
|
Colour vision |
Normal |
May be reduced |
|
RAPD |
No |
Yes, in severe cases |

Investigations
There are no specific investigations for peri-orbital cellulitis.
If there is any suspicion of orbital cellulitis or the diagnosis is unclear, referral to secondary care for further investigation is required (see orbital cellulitis section).
Management
Consider emergency referral to ophthalmology/ENT if there is any suspicion of orbital cellulitis, the patient is systemically unwell, or not responding to treatment.
Paediatric patients should be urgently referred as they require empirical intravenous antibiotic treatment and daily review due to the difficulty in differentiating between orbital and peri-orbital cellulitis. Paediatric patients are often unable to give a history and can be challenging to examine.
For adult patients, oral co-amoxiclav is usually prescribed first-line (clindamycin if penicillin-allergic). Consider a follow-up review in 24-48 hours and safety netting advice should be provided to the patient.
As for orbital cellulitis, if a sinogenic cause is suspected then patients require intranasal treatment.
Complications
Peri-orbital cellulitis can spread to cause orbital cellulitis and its subsequent sequelae. As a result, it is important to provide adequate safety netting advice to patients with peri-orbital cellulitis.
Key points
- Peri-orbital cellulitis is an infection anterior to the orbital septum. It is less severe than orbital cellulitis.
- Peri-orbital cellulitis is usually caused by contiguous spread from facial or eyelid injury, a chalazion, insect bite, or conjunctivitis but can be caused by sinusitis.
- The patient usually complains of a tender red, swollen eyelid. They are systemically well, have no eye signs but may have a fever.
- If there is any uncertainty regarding the diagnosis or it is a paediatric patient, urgent referral to secondary care should be made. Otherwise, oral antibiotics can be used in the community with follow up in 1-2 days.
- Peri-orbital cellulitis can spread and cause orbital cellulitis, so follow up of these patients in the community is necessary.
Final summary
Peri-orbital and orbital cellulitis are dependent on whether the infection is anterior or posterior to the orbital septum.
Patients with either of these conditions may present with a red swollen, tender eye and a fever. Differentiating between orbital cellulitis (sight-threatening) and peri-orbital cellulitis (less severe) is challenging. If there is diagnostic uncertainty, early referral to ophthalmology/ENT for assessment and consideration of imaging is required.
Reviewer
Mr Rakesh Mistry
ENT Registrar
Editor
Dr Chris Jefferies
References
- Patient.info. Orbital and preseptal cellulitis. Published in 2020. Available from: [LINK]
- Häggström, Mikael (2014). The right eye in sagittal section, with structures of the orbital septum within blue markings. Licence: Public domain. . Available from: [LINK]
- Paediatric Pearls. Periorbital and orbital cellulitis in children. Published in 2016. Available from: [LINK]
- American Journal of Ophthalmology. Bilateral blindness from orbital cellulitis caused by community acquire methicillin-resistant Staphylococcus aureus. Published in 2005. Available from: [LINK]
- Middle East African Journal of Ophthalmology. The Hot Orbit: Orbital Cellulitis. Published 2012. Available from: [LINK]
- American Academy of Ophthalmology. Orbital Cellulitis. Published in 2020. Available from: [LINK]
- Jonathan Trobe. Photograph showing orbital cellulitis. Licence: [CC-BY], Available from: [LINK]
- Journal of Paediatrics and Child Health. Paediatric periortbial cellulitis: A 10-year retrospective case series review. Published in 2020. Available from: [LINK]
- ENT UK. Guideline for the child presenting to hospital with pre-septal or postseptal (orbital) cellulitis. 2021. Available from: [LINK]
- MSD Manuals. Preseptal and orbital cellulitis. Published in 2020. Available from: [LINK]
- International Journal of Pediatric Otorhinolaryngology. Management of pediatric orbital cellulitis: A systematic review. Published in 2018. Available from: [LINK]
- BMJ Best Practice. Peri-orbital and orbital cellulitis. Published 2020. Available from: [LINK]
- Survey of Ophthalmology. Orbital cellulitis. Published in 2018. Available from: [LINK]
- Paediatrics and Child Health. Preseptal and orbital cellulitis in children. Published in 2016. Available from: [LINK]
- Afrodriguezg. Periorbital cellulitis. License: [CC-BY-SA]. Available from: [LINK]




