- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
The paediatric cardiovascular exam can be a logistical minefield, requiring a good understanding of cardiac anatomy and possible congenital anomalies. With babies especially, it’s important to be opportunistic with your examination – doing the three ‘quiet things’ first: auscultation of heart sounds, auscultation of breath sounds and palpation of femoral pulses.
With all children, don’t expect to follow a pre-defined order. Be creative and playful, making the examination into a game involving parents, siblings and the toys available to you.
Introduction
Wash your hands and don PPE if appropriate.
Introduce yourself to the parents and the child, including your name and role.
Confirm the child’s name and date of birth.
Briefly explain what the examination will involve using patient-friendly language: “Today I’d like to perform an examination of your child’s heart, which will involve first watching your child, then feeling their pulse and listening to their chest with my stethoscope.”
Gain consent from the parents/carers and/or child before proceeding: “Are you happy for me to carry out the examination?”
General inspection
Appearance and behaviour
Observe the child in their environment (e.g. waiting room, hospital bed) and take note of their appearance and behaviour:
- Activity/alertness: note if the child appears alert and engaged, or quiet and listless.
- Cyanosis: bluish discolouration of the skin due to poor circulation (e.g. peripheral vasoconstriction secondary to hypovolaemia) or inadequate oxygenation of the blood (e.g. right-to-left cardiac shunting).
- Shortness of breath: may indicate underlying cardiovascular (e.g. congenital heart disease) or respiratory disease (e.g. asthma).
- Pallor: a pale colour of the skin that can suggest underlying anaemia (e.g. blood dyscrasia, chronic disease) or poor perfusion (e.g. congestive cardiac failure).
- Oedema: typically presents with swelling of the limbs (e.g. pedal oedema) or abdomen (i.e. ascites). There are many causes of oedema including cardiac failure and nephrotic syndrome.
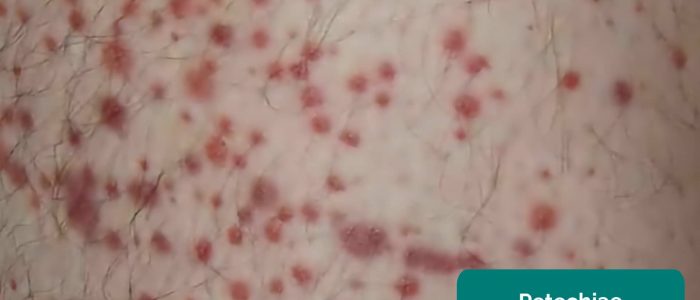
- Rashes: note the characteristics and distribution of any skin rashes (e.g. petechiae suggesting clotting disorder).
- Weight: note if the child appears a healthy weight for their age and height.
Syndromic features
Pay attention to features that may indicate the presence of an underlying genetic condition:
- Stature (e.g. tall/short)
- Syndromic facial features
See the end of this guide for a non-exhaustive list of clinical syndromes which can be associated with cardiovascular system pathology.
Equipment
Observe for any equipment in the child’s immediate surroundings and consider why this might be relevant to the cardiovascular system:
- Oxygen: saturation probe, mask, nasal prongs, oxygen tank and other breathing support.
- Mobility equipment: wheelchair, crutches and walking frame.
Medications
Note any medications by the bedside or in the child’s room and consider what underlying diagnoses they may indicate:
- Anticoagulants (e.g. warfarin/heparin): commonly prescribed for children with artificial heart valves.
- Antihypertensives (e.g. ACE inhibitors)
- Diuretics (e.g. furosemide): often used in the management of heart failure.
Hands
The hands can provide lots of clinically relevant information and therefore a focused, structured assessment is essential.
Inspect the hands
General observations
Inspect the hands for clinical signs relevant to the cardiovascular system:
- Colour: pallor suggests poor peripheral perfusion (e.g. congestive heart failure) and cyanosis may indicate underlying hypoxaemia.
- Xanthomata: raised yellow cholesterol-rich deposits that are often noted on the palm, tendons of the wrist and elbow. Xanthomata are associated with hyperlipidaemia (typically familial hypercholesterolaemia), another important risk factor for cardiovascular disease (e.g. coronary artery disease, hypertension).
- Arachnodactyly (‘spider fingers’): fingers and toes are abnormally long and slender, in comparison to the palm of the hand and arch of the foot. Arachnodactyly is a feature of Marfan’s syndrome, which is associated with mitral/aortic valve prolapse and aortic dissection.
- Absent thumbs: associated with Holt-Oram syndrome, an autosomal dominant genetic condition which causes abnormalities in the bones of the arms and hands as well as the heart (atrial septal defect, heart block).
Finger clubbing
Finger clubbing involves uniform soft tissue swelling of the terminal phalanx of a digit with subsequent loss of the normal angle between the nail and the nail bed. Finger clubbing is associated with several underlying disease processes, but those most likely to appear in a cardiovascular OSCE station include congenital cyanotic heart disease and infective endocarditis.
To assess for finger clubbing:
- Ask the child to copy you in placing the nails of their index fingers back to back.
- In a healthy individual, you should be able to observe a small diamond-shaped window (known as Schamroth’s window).
- When finger clubbing develops, this window is lost.
- If the child is too young for this to be possible, you can simply inspect the fingers, looking for soft tissue swelling of the terminal phalanx of the digits.
Signs in the hands associated with endocarditis
There are several other signs in the hands that are associated with endocarditis including:
- Splinter haemorrhages: a longitudinal, red-brown haemorrhage under a nail that looks like a wood splinter. Causes include local trauma, infective endocarditis, sepsis, vasculitis and psoriatic nail disease.
- Janeway lesions: non-tender, haemorrhagic lesions that occur on the thenar and hypothenar eminences of the palms (and soles). Janeway lesions are typically associated with infective endocarditis.
- Osler’s nodes: red-purple, slightly raised, tender lumps, often with a pale centre, typically found on the fingers or toes. They are typically associated with infective endocarditis.
Palpation
Temperature
Place the dorsal aspect of your hand onto the child’s to assess temperature:
- In healthy individuals, the hands should be symmetrically warm, suggesting adequate perfusion.
- Cool hands may suggest poor peripheral perfusion (e.g. congestive cardiac failure, cardiac shunting).
Capillary refill time (CRT)
Measuring capillary refill time (CRT) in the hands is a useful way of assessing peripheral perfusion:
- Apply five seconds of pressure to the distal phalanx of one of a child’s fingers and then release.
- In healthy individuals, the initial pallor of the area you compressed should return to its normal colour in less than two seconds.
- A CRT that is greater than two seconds suggests poor peripheral perfusion (e.g. hypovolaemia, congestive heart failure) and the need to assess central capillary refill time.
Pulses
Radial pulse
Palpate the child’s radial pulse, located at the radial side of the wrist, with the tips of your index and middle fingers aligned longitudinally over the course of the artery.
Once you have located the radial pulse, assess the rate and rhythm.
In babies, assess the femoral pulse instead.
Heart rate
Assessing heart rate:
- You can calculate the heart rate in a number of ways, including measuring for 60 seconds, measuring for 30 seconds and multiplying by 2 or measuring for 15 seconds and multiplying by 4.
- For irregular rhythms, you should measure the pulse for a full 60 seconds to improve accuracy.
Radio-radial delay
Radio-radial delay describes a loss of synchronicity between the radial pulse on each arm, resulting in the pulses occurring at different times.
To assess for radio-radial delay:
- Palpate both radial pulses simultaneously.
- In healthy individuals, the pulses should occur at the same time.
- If the radial pulses are out of sync, this would be described as radio-radial delay.
Causes of radio-radial delay
Causes of radio-radial delay include:
- Subclavian artery stenosis (e.g. compression by a cervical rib)
- Aortic dissection
- Aortic coarctation
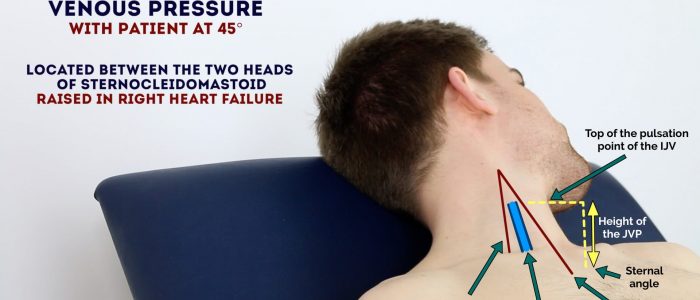
Jugular venous pressure (JVP)
Jugular venous pressure (JVP) provides an indirect measure of central venous pressure. This is possible because the internal jugular vein (IJV) connects to the right atrium without any intervening valves, resulting in a continuous column of blood. The presence of this continuous column of blood means that changes in right atrial pressure are reflected in the IJV (e.g. raised right atrial pressure results in distension of the IJV).
The IJV runs between the medial end of the clavicle and the ear lobe, under the medial aspect of the sternocleidomastoid, making it difficult to visualise (its double waveform pulsation is, however, sometimes visible due to transmission through the sternocleidomastoid muscle).
Because of the inability to easily visualise the IJV, it’s tempting to use the external jugular vein (EJV) as a proxy for assessment of central venous pressure during clinical assessment. However, because the EJV typically branches at a right angle from the subclavian vein (unlike the IJV which sits in a straight line above the right atrium) it is a less reliable indicator of central venous pressure.
See our guide to jugular venous pressure (JVP) for more details.
Measure the JVP
Assessment of the JVP is only performed in children older than 8 years old:
1. Position the child in a semi-recumbent position (at 45°).
2. Ask the child to turn their head slightly to the left.
3. Inspect for evidence of the IJV, running between the medial end of the clavicle and the ear lobe, under the medial aspect of the sternocleidomastoid (it may be visible between just above the clavicle between the sternal and clavicular heads of the sternocleidomastoid. The IJV has a double waveform pulsation, which helps to differentiate it from the pulsation of the external carotid artery.
4. Measure the JVP by assessing the vertical distance between the sternal angle and the top of the pulsation point of the IJV (in healthy individuals, this should be no greater than 3 cm).
Causes of a raised JVP
A raised JVP indicates the presence of venous hypertension. Cardiac causes of a raised JVP include:
- Right-sided heart failure: commonly caused by left-sided heart failure. Pulmonary hypertension is another cause of right-sided heart failure.
- Tricuspid regurgitation: causes include infective endocarditis and rheumatic heart disease.
- Constrictive pericarditis: often idiopathic, but rheumatoid arthritis and tuberculosis are also possible underlying causes.
Face
Observe the child’s facial complexion and features, including their eyes, ears, nose, mouth and throat.
General appearance
Inspect the general appearance of the child’s face for signs relevant to the cardiovascular system:
- Malar flush: plum-red discolouration of the cheeks associated with mitral stenosis.
- Nasal flaring/grunting: may be associated with congenital cyanotic heart disease or heart failure.
Eyes
Inspect the eyes for signs relevant to the cardiovascular system:
- Conjunctival pallor: suggestive of underlying anaemia. Gently pull down their lower eyelid to inspect the conjunctiva.
- Xanthelasma: yellow, raised cholesterol-rich deposits around the eyes associated with hypercholesterolaemia.
- Kayser-Fleischer rings: dark rings that encircle the iris associated with Wilson’s disease. The disease involves abnormal copper processing by the liver, resulting in accumulation and deposition in various tissues (including the heart where it can cause cardiomyopathy).
Mouth
Inspect the mouth for signs relevant to the cardiovascular system (tip – ask the child to see how long their tongue is or how big their mouth is):
- Central cyanosis: bluish discolouration of the lips and/or the tongue associated with hypoxaemia (e.g. a right to left cardiac shunt).
- Angular stomatitis: a common inflammatory condition affecting the corners of the mouth. It has a wide range of causes including iron deficiency.
- High arched palate: a feature of Marfan syndrome which is associated with mitral/aortic valve prolapse and aortic dissection.
- Dental hygiene: poor dental hygiene is a risk factor for infective endocarditis.
Close inspection of the chest
Ask the parent or child (if appropriate) to expose the child’s chest.
Tip: If you ask a child to show you their tummy they’ll almost always lift their top up to expose their chest as well.
Closely inspect the anterior chest
Look for clinical signs that may provide clues as to the child’s past medical/surgical history:
- Scars suggestive of previous thoracic surgery: see the thoracic scars section below.
- Pectus excavatum: a caved-in or sunken appearance of the chest (e.g. Marfan syndrome).
- Pectus carniatum: protrusion of the sternum and ribs (e.g. Noonan syndrome).
- Visible ventricular impulse: normal in thin children, can be associated with left ventricular hypertrophy.
Thoracic scars
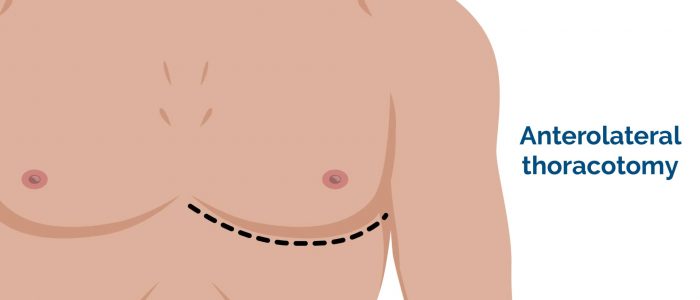
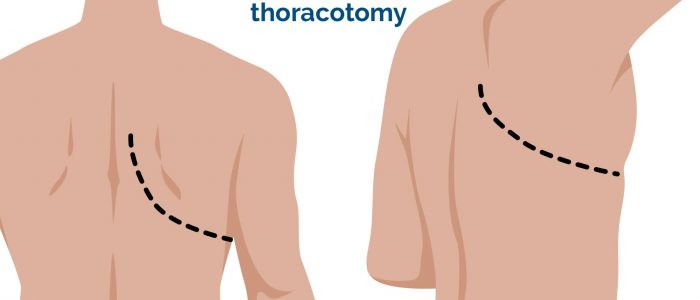
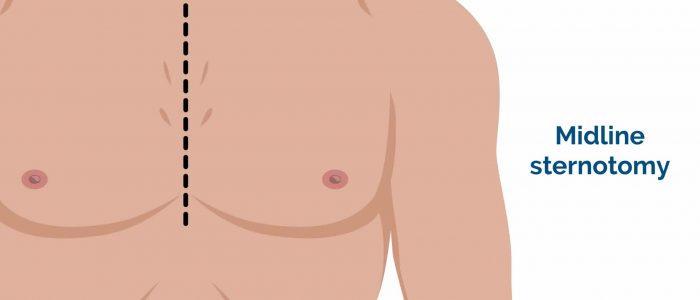
- Median sternotomy scar: located in the midline of the thorax. This surgical approach is used for cardiac valve replacement and pulmonary artery banding.
- Right thoracotomy scar: located between the lateral border of the sternum and the mid-axillary line at the 4th or 5th intercostal space on the right. This surgical approach is used to perform pulmonary artery banding and a Blalock–Taussig shunt.
- Left thoracotomy scar: located between the lateral border of the sternum and the mid-axillary line at the 4th or 5th intercostal space on the left. This surgical approach is used to perform pulmonary artery banding, patent ductus arteriosus ligation, a Blalock–Taussig shunt and coarctation of the aorta repair.
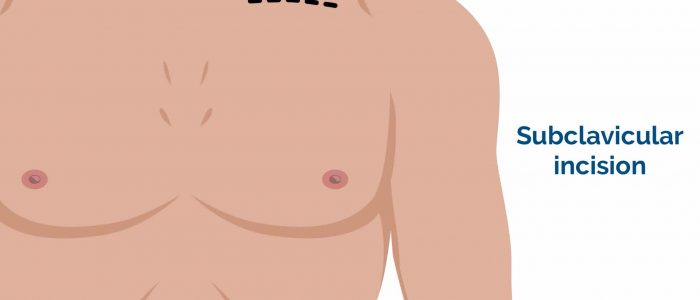
- Infraclavicular scar: located in the infraclavicular region (on either side). This surgical approach is used for pacemaker insertion.
- Left mid-axillary scar: this surgical approach is used for the insertion of a subcutaneous implantable cardioverter-defibrillator (ICD).
Palpation
Start with the abdomen and then work up to the chest. If appropriate, ask the child what they ate for their last meal and try to ‘find it’. If you can’t ‘find it’, you’ll have to listen – leading you to auscultation (sneaky right?)
Abdomen
Before beginning abdominal palpation:
- The child should already be positioned lying flat on the bed if possible.
- Kneel beside the child to carry out palpation and observe their face throughout the examination for signs of discomfort.
Liver palpation
In a healthy child, the liver edge may be palpated up to 2cm below the costal margin. If the liver edge is more prominent, it would suggest the presence of hepatomegaly. Heart failure is a potential cause of hepatomegaly.
1. Begin palpation in the right iliac fossa, starting at the edge of the superior iliac spine, using the flat edge of your hand (the radial side of your right index finger).
2. Ask the child to take a deep breath and as they begin to do this palpate the abdomen. Feel for a step as the liver edge passes below your hand during inspiration (a palpable liver edge this low in the abdomen suggests gross hepatomegaly).
3. Repeat this process of palpation moving 1-2 cm superiorly from the right iliac fossa each time towards the right costal margin.
4. As you get close to the costal margin (typically 1-2 cm below it) the liver edge may become palpable in healthy individuals.
If you are able to identify the liver edge, assess the following characteristics:
- Degree of extension below the costal margin: if greater than 2 cm this suggests hepatomegaly.
- Consistency of the liver edge: a nodular consistency is suggestive of cirrhosis.
- Tenderness: hepatic tenderness may suggest hepatitis or cholecystitis (as you may be palpating the gallbladder).
- Pulsatility: pulsatile hepatomegaly is associated with tricuspid regurgitation.
Splenic palpation
If hepatomegaly is present, you should also assess for splenomegaly. See the paediatric abdominal examination guide for details on how to perform splenic palpation.
Chest
Palpate the apex beat
Palpate the apex beat with your fingers placed horizontally across the chest, noting its position.
Normal position:
- <7 years old: 4th intercostal space to the left of the midclavicular line.
- >7 years old: 5th intercostal space in the midclavicular line.
Abnormal position:
- Left displacement: causes include cardiomegaly, pectus excavatum and scoliosis.
- Right displacement: causes include dextrocardia, left diaphragmatic hernia, collapsed right lung, left pleural effusion and left tension pneumothorax.
Assess for heaves and thrills
Heaves:
- A parasternal heave is a precordial impulse that can be palpated.
- Place the heel of your hand parallel to the left sternal edge (fingers vertical) to palpate for heaves.
- Tip: Instead of the heel of your hand, use your fingertips with babies and younger children.
- If heaves are present you should feel the heel of your hand being lifted with each systole.
- Parasternal heaves are typically associated with right ventricular hypertrophy.
Thrills:
- A thrill is a palpable vibration caused by turbulent blood flow through a heart valve (a thrill is a palpable murmur).
- You should assess for a thrill across each of the heart valves in turn (see valve locations below).
- To do this place your hand horizontally across the chest wall, with the flats of your fingers and palm over the valve to be assessed.
Valve locations
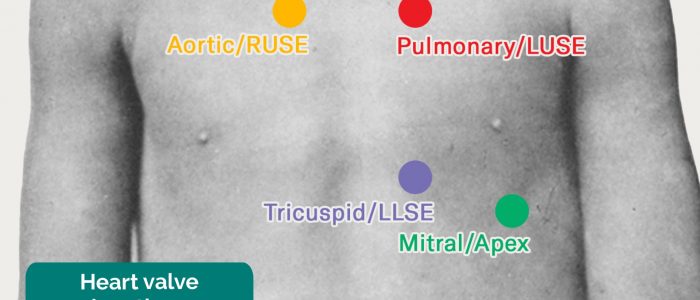
- Mitral valve: 5th intercostal space in the midclavicular line.
- Tricuspid valve: 4th or 5th intercostal space at the lower left sternal edge.
- Pulmonary valve: 2nd intercostal space at the left sternal edge.
- Aortic valve: 2nd intercostal space at the right sternal edge.
Auscultation
Auscultate the heart
Start by showing the child your stethoscope and demonstrate it on your own chest and/or on one of their toys to familiarise them with this piece of equipment.
Suggest listening to their chest, making sure the stethoscope diaphragm isn’t cold prior to it making contact with the child.
Tip: Play a game to see who can stay quiet the longest – involve the parents!
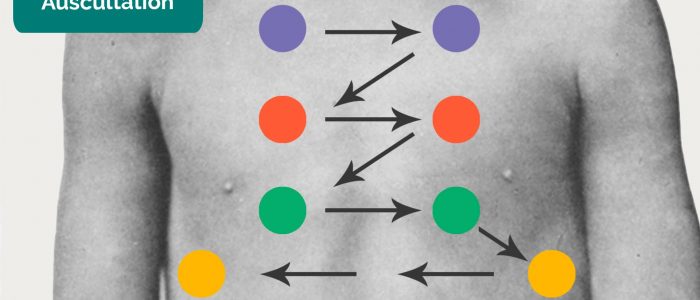
Areas of the heart to auscultate
Auscultate ‘upwards’ through the valve areas using the diaphragm of the stethoscope:
- Mitral valve: 5th intercostal space in the midclavicular line.
- Tricuspid valve: 4th or 5th intercostal space at the lower left sternal edge.
- Pulmonary valve: 2nd intercostal space at the left sternal edge.
- Aortic valve: 2nd intercostal space at the right sternal edge.
Repeat auscultation across the four valves with the bell of the stethoscope.
Bell vs diaphragm
The bell of the stethoscope is more effective at detecting low-frequency sounds, including the mid-diastolic murmur of mitral stenosis. The diaphragm of the stethoscope is more effective at detecting high-frequency sounds, including the ejection systolic murmur of aortic stenosis, the early diastolic murmur of aortic regurgitation and the pansystolic murmur of mitral regurgitation.Tip: Complex cardiac anomalies may cause you to hear multiple dynamic murmurs (e.g. Tetralogy of Fallot).
Auscultate the lungs
Auscultate the lung fields on the anterior and posterior aspect of the chest:
- Ask the child to take ‘big breaths’ – some abnormal sounds may be inaudible if the child is taking shallow breaths.
- Auscultate each side of the chest in a symmetrical pattern, comparing side to side.
- Pay attention to the inspiratory and expiratory sounds at each placement.
- Note the quality and volume of breath sounds and note any additional sounds.
- Coarse bibasal crackles may be a late sign of pulmonary congestion secondary to congestive heart failure.
Final steps
Assess for evidence of oedema:
- Ask the parents if the child looks puffy or swollen.
- Inspect the limbs, sacral area and face: affected areas will depend on the age of the child and mobility status.
- Peripheral oedema often occurs in right-sided heart failure.
To complete the examination…
Explain to the child and parents that the examination is now finished.
Ensure the child is re-dressed after the examination.
Thank the child and parents for their time.
Explain your findings to the parents.
Ask if the parents and child (if appropriate) have any questions.
Dispose of PPE appropriately and wash your hands.
Summarise your findings to the examiner.
Further assessments and investigations
Suggest further assessments and investigations to the examiner:
- Abdominal examination: if hepatomegaly was noted.
- Respiratory examination: if abnormalities noted during inspection and auscultation of the chest.
- Peripheral vascular examination: if poor peripheral perfusion or oedema were identified.
- Vital signs
- ECG: if concerned about cardiac pathology.
- Measure and plot height and weight on a growth chart.
- Urinalysis: if oedema present.
Murmurs
More than 50% of children will have a murmur at some point while congenital heart disease is present in less than 1% of children. The table below includes a non-exhaustive list of murmur characteristics and underlying causes.
| Syndrome | Clinical features |
| LOCATION | Aortic area: aortic stenosis Pulmonary area:
Subclavian, holosystolic: patent ductus arteriosus Lower right sternal edge: tricuspid regurgitation Tricuspid area:
Apex: mitral regurgitation – increases on lying on left, radiates to the axilla |
| TIMING |
|
| DURATION |
|
| LOUDNESS (systolic murmur grade) |
|
| SITE OF MAXIMAL INTENSITY |
|
| RADIATION |
|
Syndromes that may impact the cardiovascular system
Below is a table containing a non-exhaustive list of syndromes that can impact the cardiovascular system.
The features of each syndrome relevant to the cardiovascular system are shown in bold.
| Syndrome | Clinical features |
| Alagille syndrome In 90 percent of cases, caused by mutations in the JAG1 gene. |
Broad forehead Small chin Flat face |
|
CHARGE syndrome CHARGE syndrome is a genetic syndrome with a characteristic set of features. |
Coloboma (of the eye) Choanal atresia Heart anomalies (see below) Tetralogy of Fallot Patent ductus arteriosus Ventricular septal defect Atrial septal defect Atrioventricular septal defect |
| DiGeorge syndrome A constellation of signs and symptoms associated with defective development of the pharyngeal pouch system. Most cases are caused by a heterozygous chromosomal deletion at 22q11.2. |
Hearing loss Cleft palate Micrognathia Hypoplastic malar |
| Down’s syndrome A genetic disorder caused by the presence of all or part of a third copy of chromosome 21. |
Epicanthic folds Brushfield spots Protruding tongue Low set ears |
| Fetal alcohol spectrum disorder A range of effects that can occur in an individual who was prenatally exposed to alcohol. |
Microcephaly Intrauterine growth restriction Smooth philtrum Joint abnormality |
| Fragile X syndrome An X-linked disorder and the most common inherited cause of intellectual disability: Both males and females can be affected. |
Macrocephaly Prominent ears and jaw Hypermobility Macroorchidism |
| Marfan syndrome An autosomal dominant connective tissue disorder. |
Marfanoid habitus (tall, long limbs) Hypermobility Arachnodactyly Chest wall deformities |
| Noonan syndrome An autosomal dominant condition. 50% of children have a pathogenic variant in protein tyrosine phosphatase, nonreceptor type 11 (PTPN11). |
Turner phenotype Pulmonary stenosis Hypertrophic cardiomyopathy |
| Turner syndrome Caused by loss of part or all of an X chromosome – affecting only females. |
Short stature Delayed puberty Webbed neck Shield chest |
| William’s syndrome Caused by the deletion of genetic material from a specific region of chromosome 7. |
Short palpebral fissures Upturned nose Cupid bow lip |
Reviewer
Dr Sunil Bhopal
Senior Paediatric Registrar
References
Text references
- Bishop (2011). Cardiac Examination. Learnpediatrics.com Narration. The University of British Columbia. [LINK] (Accessed 18 Mar 2019)
- Lissauer, T., Clayden, G., & Craft, A. (2012). Illustrated textbook of paediatrics. Edinburgh: Mosby.
- Miin Lee (2013). Cardiovascular Examination Guide. MRCPCH Clinical Revision. Trainees Committee, London School of Paediatrics. [LINK] (Accessed 18 Mar 2019)
- Tasker, R. C., McClure, R. J. & Acerini, C. L. (2013). Oxford handbook of paediatrics. Oxford: Oxford University Press.
- Towers, A (2015). Examination: cardiovascular, Don’t Forget the Bubbles. [LINK](Accessed 18 Mar 2019)
Image references
- Cornelia Csuk. Adapted by Geeky Medics. Cyanosis. Licence: CC BY-SA.
- Nephrotic syndrome. Adapted by Geeky Medics. Licence: CC BY-SA.
- Hektor. Adapted by Geeky Medics. Purpura. Licence: CC BY-SA.
- Adapted by Geeky Medics. Min.neel. Xanthoma in a child. Licence: CC BY-SA.
- Adapted by Geeky Medics. Desherinka. Finger clubbing. Licence: CC BY-SA.
- Adapted by Geeky Medics. Warfieldian. Janeway lesions. Licence: CC BY-SA.
- Adapted by Geeky Medics. Roberto J. Galindo. Osler’s nodes. Licence CC BY-SA.
- Adapted by Geeky Medics. Klaus D. Peter, Gummersbach, Germany. Xanthelasma. Licence: CC BY 3.0 DE.
- Adapted by Geeky Medics. Herbert L. Fred, MD, Hendrik A. van Dijk. Kayser-Fleischer ring. Licence: CC BY 3.0.
- Adapted by Geeky Medics. Ankit Jain, MBBS, corresponding author Anuradha Patel, MD, FRCA and Ian C. Hoppe, MD. Central cyanosis. Licence: CC BY-SA.
- Adapted by Geeky Medics. Matthew Ferguson. Angular stomatitis. Licence: CC BY-SA.
- Adapted by Geeky Medics. Jprealini. Pectus carinatum. Licence: CC BY-SA.
- Adapted by Geeky Medics. Aurora Bakalli, Tefik Bekteshi, Merita Basha, Afrim Gashi, Afërdita Bakalli and Petrit Ademaj. Pectus excavatum. Licence: CC BY-SA.
- Ragesoss, Physical exam of a child with stethoscope on the chest, Colour, CC BY-SA 3.0.
- Adapted by Geeky Medics. James Heilman, MD. Pedal oedema. Licence: CC BY-SA.