- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
This paediatric venepuncture guide provides a step-by-step approach to performing venepuncture in children and young people.
Preparation
If intravenous access is likely to be required, it is preferable to insert a cannula and take blood samples at the same time (to avoid performing a second procedure). However, vascular access devices should not be left in situ if they are not required to minimise infection risk.
Children should be offered a topical anaesthetic where time allows (e.g. Ametop™, EMLA™ or LMX-4™).
Check the minimum age the product is licensed for and the minimum and maximum durations the anaesthetic should be left on the skin, as this differs between products.
Apply a blob of cream over the vein and cover it with a clear film dressing. It can be helpful to wrap it with a bandage to prevent the child from removing the cream.
Older children can be offered a vapocoolant spray (‘cold spray’), used at the time of cannulation.1 It is reasonable to show them what it feels like first, as the spray can startle some children.
Babies can be given oral sucrose to minimise pain. The majority of evidence of effectiveness is in infants <3 months, but there may be an analgesic effect in infants up to 12 months.2 It can also help if they are held by a parent.
Once the topical anaesthetic has been applied for the recommended time, and you are ready to perform venepuncture, take the child to a treatment room away from their bedspace if possible. This aims to keep the child’s bed space as a safe space which they do not associate with traumatic procedures.
Gather equipment
Collect all equipment needed for the procedure and place it within reach on a tray or trolley, ensuring that all the items are clearly visible.
The equipment you need will differ depending on the age of the child.
- Clean procedure tray
- Non-sterile gloves and apron
- Tourniquet (if appropriate)
- Vapocoolant spray (‘cold spray’), if required
- Alcohol swab (2% chlorhexidine gluconate in 70% isopropyl)
- Blood sampling device (e.g. butterfly needle, cannula or flag needle)
- Blood specimen bottles
- Sharps container
- Gauze or cotton wool
- Sterile plaster
- Laboratory forms, labels and transportation bag
Ask a play specialist to accompany you to distract and reassure the child.
In older children, a tourniquet can be used. In younger children, a colleague should act as the tourniquet by holding around the arm and squeezing. This will also help minimise movement from the child.
In babies, you should be able to hold the limb tightly enough to act as a tourniquet, but an assistant can help if required.
Introduction
Wash your hands using alcohol gel. If your hands are visibly soiled, wash them with soap and water.
Don PPE if appropriate.
Introduce yourself to the child and parent/caregiver, including your name and role.
Confirm the patient’s name and date of birth with either the patient or parent (depending on age).
Briefly explain what the procedure will involve using age-appropriate language.
For example, with younger children: “I need to take some of your blood to look at to help find out why you are poorly.”
Older children, or children who have previously had blood taken, may have a better understanding of what is going to happen and so the explanation should be tailored to this. For example: “I’m going to take a blood sample using a small needle/cannula, so we can try to find out why you are poorly. Once I have taken the sample, I will take the needle out again.”
Managing fear
Some children become particularly frightened when you approach them with a tray of unfamiliar objects. It can help to ask, “would you like me to talk about what we are going to do first and show you all the equipment so you know what it does?”.
They may decide they don’t want to see anything, so you should ensure the parent knows what will happen. However, most are much less frightened once they know what the equipment does.
Gain consent (from the parent(s) and the child, if appropriate) to proceed with venepuncture.
Check if the patient has any allergies (e.g. latex).
Expose the site
Remove any local anaesthetic cream with a paper towel or gauze, if used.
Identify and expose the site. Make sure you take your time looking for a vein you feel most likely to be successful in taking blood from.
When choosing a vein:
- Do not take blood from an arm with IV fluids running through it as the results can be altered by the fluids.
- Avoid areas of skin damage or bruises.
- In children, veins are less likely to be palpable and ‘spongy’ compared to adults, and you may have to aim for those you can see, rather than feel.
Preparation
1. Don gloves (gloves don’t need to be worn for cleaning the site, but they should always be donned prior to performing venepuncture itself).
2. Clean the site with an alcohol swab for 30 seconds and then allow to dry completely for 30 seconds:
- You should start cleaning from the centre of the venepuncture site and work outwards to cover an area of 5cm or more.
- DO NOT touch the cleaned site afterwards at any point, otherwise, the cleaning procedure will need to be repeated prior to venepuncture.
General venepuncture procedure
1. Prepare the needle device you are using (see below for different types of devices)
2. Make sure everyone is ready to start, including the parent, play specialist, and the person holding the child’s arm.
3. Apply the tourniquet/squeeze.
4. Anchor the vein with your non-dominant hand from below by gently pulling on the skin distal to the insertion site. If someone is acting as your tourniquet, they can provide slight upward traction on the skin.
5. If you are using vapocoolant spray, ask your assistant to spray from a distance of 15-20cm from the skin, in either 2-3 short bursts or for a couple of seconds. The skin should turn slightly white (avoid ‘frosting’ the skin as this can be painful).
6. Insert the needle with the bevel facing upwards within 15 seconds of applying the vapocoolant spray. In children, the entry angle is less than in adult venepuncture and can sometimes be almost parallel to the skin.
7. If you have entered the vein, blood should start dripping or you should see flashback, depending on the device used.
8. Collect blood samples, then remove the tourniquet
9. Withdraw the needle and then apply gentle pressure to the site with some gauze or cotton wool.
10. Apply a dressing to the patient’s arm (e.g. cotton wool, gauze, plaster).
11. Let go of the child’s limb and congratulate them for being brave! Many children will respond well to rewards, such as stickers, after a painful procedure.
Number of attempts
Children can quickly become distressed with repeated attempts to take blood. As a general rule of thumb, a single practitioner should have no more than two attempts before seeking senior support.
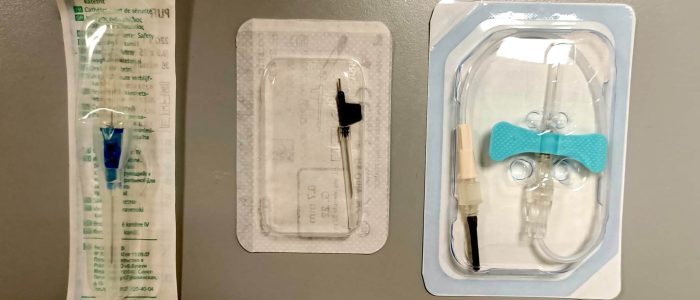
Venepuncture devices
There are several methods to collect blood from a child, using various different pieces of equipment. The most common methods are using a cannula or a butterfly needle, but you may also see flag needles used in practice.
There is no single ‘best’ method, different devices are better for different patients, and everyone develops their own preferences over time.
Cannula
Intravenous cannulation is a common method of collecting blood from children, and any sized cannula can be used in any size of child.
The procedure for paediatric cannulation should be followed. However, the cannula is removed after blood has been collected (if ongoing IV access is not required).
Blood can either be allowed to drip out of the end of the cannula, collected with a blunt fill needle and syringe if taking a blood culture, or collected with a small syringe.
Butterfly needle
This technique is similar to venepuncture using a butterfly needle in adults.
Follow the initial steps described above: identify a site, use an appropriate anaesthetic, clean and appropriately position the patient.
1. Attach a small syringe to the end of the butterfly tubing. The smaller the syringe, the less negative pressure is generated, and you are less likely to collapse the vein.
2. Insert the needle into the skin with the bevel upwards. Veins in children are more superficial than in adults, so the angle of entry is less (sometimes almost parallel with the skin).
3. Observe for flashback into the butterfly tubing, indicating you have entered the vein.
4. Gently pull back on the syringe to aspirate blood. If larger volumes are needed, the syringe can be changed during the procedure.
5. Once you have obtained the appropriate volume of blood, remove the tourniquet, then remove the needle and apply pressure.
Flag needle
These needles are not typically encountered in adult medicine but can be found on paediatric wards. The needle is a small metal tube with a plastic handle attached, which looks like a flag on a pole.
Follow the initial steps described above: identify a site, use an appropriate anaesthetic, clean and appropriately position the patient.
1. Insert the needle into the skin with the bevel upwards. Veins in children are more superficial than in adults, so the angle of entry is less (sometimes almost parallel with the skin).
2. Once you have entered the vein, blood should immediately start dripping out of the back of the needle. This happens rapidly, so make sure you have the blood bottles ready.
3. Allow the blood to drip from the flag needle into the desired blood bottles.
4. Once you have obtained the samples you require, release the tourniquet, then remove the needle and apply pressure.
This method is not suitable for collecting sterile samples required for blood cultures.
Paediatric blood bottles
For most patients, samples will be collected into specific paediatric-sized blood bottles. In teenage patients who are ‘adult-sized’, blood can be collected into standard-sized bottles, as you would in an adult.
The bottles have the same colour coding as full-sized bottles. However, check local guidelines where there is any uncertainty.
Generally, most paediatric-sized blood bottles will need 0.25 – 1ml of blood, depending on the type of bottle and tests required. A couple of exceptions to this rule:
- Coagulation profile: there is a paediatric-sized ‘blue bottle’, but this needs filling to the fill line to be processed.
- ESR: in most laboratories, this requires a standard-sized ‘purple bottle’ as approximately 2ml of blood is required.
Paediatric blood cultures
When taking a paediatric blood culture, only one bottle is generally used. This is a specific paediatric blood culture bottle, but it creates an aerobic environment for the culture.
There is no clear guidance on the optimum amount of blood to put into a blood culture bottle, and manufacturer advice differs greatly from usual clinical practice. As a rule of thumb, you should be putting as many millilitres of blood as their age in years (i.e. 5ml for a 5-year-old). Blood cultures with insufficient volumes of blood can lead to false negative results.
To complete the procedure…
Explain to the patient and parent that the procedure is now complete.
Document the patient’s details on the blood sample bottles at the bedside (using either pre-printed or handwritten labels).
Dispose of PPE appropriately and wash your hands.
Send the blood samples to the lab for analysis in an appropriate plastic leak-proof bag with the completed laboratory request form.
Reviewer
Dr Matt Fox
Editor
Dr Chris Jefferies
References
- Griffith RJ et al. Vapocoolants (cold spray) for pain treatment during intravenous cannulation. Published 2016. Available from: [LINK]
- Thyr M et al. Oral glucose as an analgesic to reduce infant distress following immunization at the age of 3, 5 and 12 months. Published January 2007. Available from: [LINK]
- Royal Children’s Hospital Melbourne. Intravenous access – peripheral. Updated in September 2019. Available from: [LINK]
- World Health Organisation. WHO guidelines on drawing blood: best practices in phlebotomy. Published 2010. Available from: [LINK]