- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
This article discusses possible underlying causes of a painless red eye, including dry eye, acute conjunctivitis, episcleritis and subconjunctival haemorrhage.
Significant ocular pain and/or changes in visual acuity are red flags for more serious diagnoses, which will be discussed in our painful red eye article.
Dry eye and blepharitis
‘Dry eye‘ is a syndrome of bilateral ocular surface inflammation and tear film instability.
Typical symptoms include ocular discomfort (burning, grittiness, foreign body sensation) and fluctuating visual acuity. Paradoxical watering may occur secondary to reflex tear secretion.
Causes
Dry eye can be classified into two broad categories:
- Evaporative: the most common cause is blepharitis (meibomian gland dysfunction). Inflammation of the eyelid margins results in obstruction of lipid-producing meibomian glands, which leads to unstable tears that evaporate easily.
- Tear deficiency: Sjogren’s syndrome (involves damage to the aqueous secreting lacrimal glands).
Clinical features
On clinical examination, blepharitis appears as erythematous and thickened eyelid margins. The base of eyelashes may reveal crusting and matting. Immediately posterior to the eyelashes, yellow ‘capping’ of meibomian gland orifices may be seen.
Blepharitis is a risk factor for the development of styes (hordeola) and chalazia which appear as lumps on the eyelid resulting from the accumulation of secretions in the meibomian glands.
For more information, see the Geeky Medics guide to eyelid disorders.
Management
Management options for blepharitis and dry eye include:
- Lifestyle modifications: reducing contact lens wear, regular breaks when using a screen, and increasing the level of humidity in the environment.
- Regular lid hygiene to remove the build-up of debris. Warm compresses followed by lid massage to express meibomian gland secretions.
- Preservative-free ocular lubricants (thin daily preparations and thicker ointments before bed).
- An extended course of low-dose oral tetracyclines and regular omega-3 fatty acid supplements may have a useful anti-inflammatory effect.
Symptoms not controlled with these measures should be referred to ophthalmology for specialist management. Options include topical immunosuppression and punctal occlusion.

Conjunctivitis
Conjunctivitis involves inflammation of the conjunctiva over the sclera (bulbar conjunctiva) and inner eyelids (tarsal conjunctiva).
Conjunctivitis has varying causes with slightly differing clinical presentations. Most cases are bilateral to some extent due to symmetrical pathologies (allergy, eye drop toxicity and other chemical exposure) or cross-infection from one eye to the other.
Most cases of conjunctivitis can be diagnosed from clinical features however swabs are helpful for diagnosis if symptoms persist or chlamydial/gonococcal disease is suspected.
Clinical features
Clinical features associated with all forms of conjunctivitis include:
- General discomfort, watering, and grittiness, with variable amounts of discharge
- It is typical for the eyelids to be crusted shut in the morning (not aetiologically specific)
- Diffuse conjunctival injection, possibly with swollen conjunctiva (chemosis) and debris
Viral conjunctivitis
Viral conjunctivitis is caused by adenovirus and other common viruses.
Patients present with a clear, watery discharge with associated coryzal symptoms and pre-auricular lymphadenopathy. Corneal involvement may result in photophobia.
Management is generally conservative. Lubricants and cool compresses can provide symptomatic relief.
Patients should be advised that symptoms may take weeks to resolve and that this condition is very contagious. Patients should wash their hands regularly and not share towels with others.
Some patients may have persistent photophobia secondary to inflammation within the cornea and require referral to an ophthalmologist for topical steroids. Non-specialists should never initiate topical steroids.
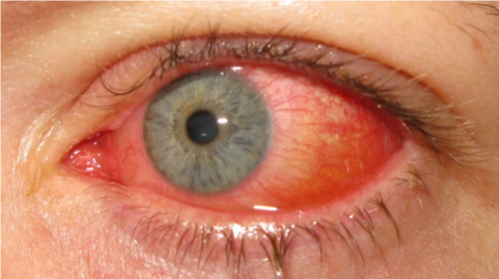
Bacterial conjunctivitis
Bacterial conjunctivitis is less common than viral conjunctivitis and caused by the same pathogens as respiratory infections (commonly pneumococcus, staphylococcus or haemophilus).
Differentiating features from viral conjunctivitis include more extensive conjunctival injection and mucopurulent discharge.
Most cases are self-limiting. However, topical antibiotic drops (e.g. chloramphenicol) can quicken the resolution of symptoms.
Sexually transmitted infections
Bacterial conjunctivitis associated with sexually transmitted infections (chlamydia, gonorrhoea) presents as unilateral, non-resolving conjunctivitis. Severe discharge is seen in gonococcal disease.
These patients require systemic antibiotic treatment and referral to genitourinary medicine for evaluation of genital disease and contact tracing.
Allergic conjunctivitis
Allergic conjunctivitis is common, especially in individuals with a history of atopy. The precipitating allergen may be known or unknown. There are variants which can occur year-round with unclear precipitants.
Itching is the hallmark feature of allergic conjunctivitis with associated swelling of the eyelids and conjunctiva (chemosis).
Management includes identifying and reducing the causative allergen along with topical lubricants, topical anti-histamines and mast cell stabilisers. Cold compresses and oral antihistamines are also useful.
Severe cases may require topical immunosuppression initiated by a specialist.
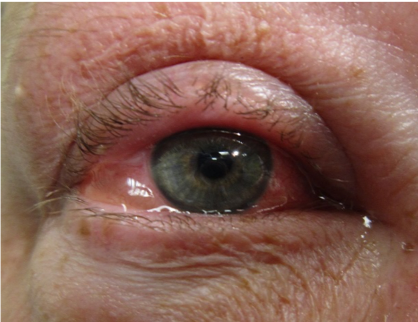
Episcleritis
Episcleritis is inflammation of the episclera, a thin vascular layer sandwiched between the superficial conjunctiva and deeper sclera.
Aetiology
Usually, there are no obvious precipitants for episcleritis, though symptoms tend to recur, and the disease is associated with some systemic autoimmune conditions (30% of cases), such as ulcerative colitis.
Clinical features
Episcleritis presents with a sectoral area of hyperaemia, with obvious red dilated superficial vessels.
The subconjunctival injection in episcleritis is superficial and, as a result, moveable with a swab pressed gently on the conjunctiva following topical anaesthetic drops. The subconjunctival injection of episcleritis also blanches with topical phenylephrine (a vasoconstrictor).
Episcleritis vs scleritis
The important differential diagnosis to exclude is scleritis, which does not obey the rules above (e.g. doesn’t move with a swab or blanch with phenylephrine).
Scleritis is usually painful and features violaceous dull red areas of underlying inflammation. Discharge or significant watering indicates an alternative diagnosis, such as conjunctivitis.
For more information on scleritis, see the Geeky Medics guide to a painful red eye.
Management
There is no specific treatment for episcleritis, and the condition is self-limiting, with simple analgesia and topical lubricants used to manage symptoms. Occasionally, topical steroids or oral/topical NSAIDs may be required.
Non-resolution of symptoms within 2-3 weeks should prompt referral to an ophthalmologist.

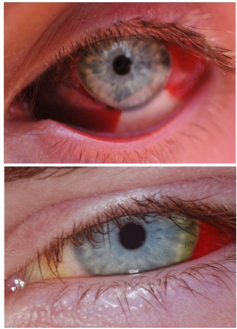
Subconjunctival haemorrhage
A subconjunctival haemorrhage is a common presentation, and patients are often concerned because of its striking appearance.
Aetiology
Subconjunctival haemorrhages can be precipitated by trauma, a sudden rise in intrathoracic pressure (e.g. lifting heavy weights) or eye rubbing.
Risk factors include hypertension and anticoagulants/antiplatelets. The development of subconjunctival haemorrhage can, therefore, be an indicator of underlying issues such as uncontrolled hypertension or deranged coagulation (e.g. raised INR).
Clinical features
Subconjunctival haemorrhage is usually asymptomatic, though it can be slightly irritating and produce a gritty feeling in some cases. On examination, the haemorrhage can be small and localised or diffuse. The haemorrhage stops at the limbus (junction between the cornea and conjunctiva).
Management
No management is required unless an underlying factor has caused the haemorrhage (e.g. warfarin may need to be reversed if INR is dangerously raised). Lubricants should be provided for symptomatic relief if the eye feels gritty.
Patients should be advised the subconjunctival haemorrhage will resolve over a few weeks (typically fading from a deep red to a faint yellow before fully resolving).
If the patient has developed a subconjunctival haemorrhage secondary to trauma, serious underlying injuries such as lacerations or globe rupture should be excluded. This is discussed in more detail in the guide to eye trauma.
Key points
- A painless red eye, without visual disturbance, is unlikely to have a sinister underlying cause.
- Common causes of a relatively painless red eye include dry eye, acute conjunctivitis, episcleritis and subconjunctival haemorrhage.
- A thorough history and clinical assessment should help you exclude concerning features and narrow the differential diagnosis.
Reviewer
Dr Ashley Simpson
Ophthalmology Registrar
Editors
Fiona Kirkham
Dr Chris Jefferies
References
Text references
- Salmon, J. F. (2019). Kanski’s Clinical Ophthalmology: A Systematic Approach (9th ed.). Elsevier.
Image references
- Figure 1. Imrankabirhossain. License: [CC BY-SA 4.0]
- Figure 2. Marco Mayer. License: [CC BY-SA 4.0]
- Figure 3. James Heilman, MD. License: [CC BY-SA 4.0]
- Figure 4. Asagan. License: [CC BY-SA 3.0]
- Figure 5. Therealbs2002. License: [CC BY-SA 3.0]




