- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
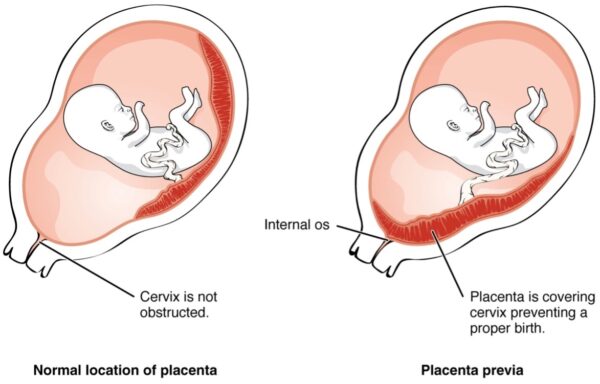
Placenta praevia is a cause of antepartum haemorrhage (defined as bleeding > 24 weeks gestation) which occurs when the placenta overlies the lower uterine segment.
Five percent of women have a low-lying placenta at their 20-week scan, but only 0.5% at delivery because the placenta migrates during pregnancy.
The incidence of placenta praevia is rising due to increasing caesarean section and assisted reproduction (IVF) rates, it has an overall incidence of 1/200 births.1
Aetiology
The exact cause of placenta previa is unknown. Potential causes include abnormal vascularisation of the endometrium due to atrophy or scarring from previous surgery, trauma, or infection.
Grades of placenta praevia
There are four grades of placenta praevia:
- Grade 1 (minor): placenta does not cover internal cervical os but is low lying
- Grade 2 (marginal): lower edge reaching the internal os
- Grade 3 (partial): lower edge partially covering the internal cervical os
- Grade 4 (complete): lies over the internal cervical os
Risk factors
Risk factors for placenta praevia include:3
- Previous history of placenta praevia
- Previous caesarean section (CS): one CS increases risk by 2.2, two CS by 4.1 and three CS by 22.4
- Increasing maternal age
- Increasing parity
- Smoking
- Cocaine use during pregnancy
- Previous spontaneous or induced abortion
- Deficient endometrium (e.g. history of endometriosis)
- Assisted conception (IVF)
Clinical features
Most cases of placenta praevia are asymptomatic and are detected on routine ultrasound at the 20-week scan.
History
Typical symptoms of placenta praevia include:
- Antepartum haemorrhage: painless bright red vaginal bleeding (>24 weeks gestation)
- Light contractions may be present
Other important areas to cover in the history:
- Fetal movements
- Obstetric history: previous pregnancies, delivery mode, gestation and complications (previous caesarean sections increase risk)
- Past medical history: endometriosis
- Assisted contraception (IVF)
- Risk factors (e.g. smoking and drug use)
- Provoking factors: post-coital
Clinical examination
A digital vaginal examination should not be performed, as this may trigger heavy bleeding in unconfirmed placenta praevia.
A careful speculum examination can be performed to check that membranes have not ruptured and that the cervix is closed.
Typical clinical findings in placenta praevia include:
- Non-tender uterus
- Vaginal bleeding
- Signs of shock (pallor, distress, capillary refill, cool peripheries): if significant bleeding has occurred
Differential diagnoses
Possible differential diagnoses in the context of placenta praevia include:
- Placental abruption: usually painful, dark red blood, bleeding may be concealed. The uterus may feel ‘woody’ or ‘tense’ on examination.
- Uterine rupture: usually occurs in labour with a history of previous caesarean section
- Vasa praevia: where fetal blood vessels run near the internal cervical os (associated with the characteristic triad of vaginal bleeding, rupture of membranes and fetal deterioration).
- Benign lesions (e.g. cervical ectropion – common)
- Malignant lesions (e.g. carcinoma)
- Infections (e.g. chlamydia)
For more information on other causes of antepartum haemorrhage, see the Geeky Medics guide to antepartum haemorrhage.
Investigations
Bedside investigations
Relevant bedside investigations include:
- Cardiotocograph (CTG): in women above 26 weeks gestation
Laboratory investigations
Relevant laboratory investigations for placenta praevia include:
- FBC, U&Es, LFTs: useful to rule out hypertensive conditions such as HELLP or pre-eclampsia
- Group and save/crossmatch: if large volumes of blood loss patient may require transfusion
- Clotting profile: important in the context of bleeding
- Kleihauer test: required if the woman is resus negative
Imaging
Ultrasound is used to establish a definitive diagnosis of placenta praevia.
The Royal College of Obstetricians and Gynaecologists (RCOG) recommend the use of transvaginal ultrasound as it improves the accuracy of placental localisation and is considered safe.
Management
Asymptomatic placenta praevia
If a low-lying placenta is seen at the 20-week scan and the patient is asymptomatic, the patient should be rescanned at 32 or 36 weeks depending on whether placenta praevia is major or minor.
If placenta praevia is still present at the following scan, serial scans should be performed every two weeks from that point onward.
A final ultrasound is performed at 36-37 weeks to determine the method of delivery:
- Elective caesarean section for major placenta praevia at 38 weeks.
- If minor, then a trial of vaginal delivery may be offered. RCOG recommends that the placenta should be at least 2 cm away from the internal os for attempted vaginal delivery.
Placenta praevia carries an increased risk of obstetric haemorrhage and hysterectomy. All women with placenta praevia and their partners should have a discussion regarding complications and mode of delivery. Any decisions to decline blood or blood products should be discussed openly and documented.
Placenta praevia with bleeding (antepartum haemorrhage)
Management of an antepartum haemorrhage due to placenta praevia includes a rapid ABCDE assessment and resuscitation. Maternal resuscitation should not be delayed to determine fetal viability.
If the patient is unable to be stabilised or is in labour an emergency caesarean section is recommended.
Complications
Maternal complications of placenta praevia include:
- Haemorrhage: bleeding can occur from simple trauma (e.g. intercourse) or as the cervix opens during labour due to the low-lying placenta. Additionally, there is a risk of abruption when the fetus moves into the lower uterine segment.
- Hypovolemic shock secondary to bleeding
- Death is rare (a major cause of death in women with placenta praevia is now postpartum haemorrhage)
Fetal complications of placenta praevia include:
- Fetal haemorrhage
- Intrauterine growth restriction (IUGR)
- Premature birth
Key points
- Placenta praevia is a cause of antepartum haemorrhage (defined as bleeding > 24 weeks gestation) which occurs when the placenta overlies the lower uterine segment.
- Placenta praevia can be defined as minor or major depending on placental proximity to the internal cervical os.
- Risk factors include past caesarean section, previous placenta praevia, advanced age or parity, smoking, cocaine and endometriosis.
- Patients can be asymptomatic or present with an antepartum haemorrhage (painless bright red vaginal bleeding >24 weeks gestation).
- Ultrasound is the definitive diagnostic investigation.
- Management in asymptomatic placenta praevia includes serial ultrasound scans and planning the mode of delivery (elective caesarean section) repeat ultrasound scanning and making plans for safe delivery.
- Management for symptomatic placenta praevia (antepartum haemorrhage) includes a rapid ABCDE assessment and resuscitation. If unable able to stabilise or if in labour an emergency caesarean section should be performed.
- Maternal complications include haemorrhage, hypovolemic shock and death.
- Fetal complications include fetal haemorrhage, IUGR and premature birth.
Reviewer
Dr Rachel Greenwood
Obstetrics & Gynaecology Registrar
Editor
Dr Chris Jefferies
References
- Neilson JP. Interventions for suspected placenta praevia. Cochrane Database Systematic Review. 2003(2):CD001998.
- OpenStax College. Placenta Praveia. Licence: [CC BY 3.0]
- Faiz AS, Ananth CV. Etiology and risk factors for placenta praevia: an overview and meta-analysis of observational studies. Journal of Maternal, Fetal and Neonatal Medicine. 2003 Mar13(3):175-90




