- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
This pre-hospital advanced life support (ALS) OSCE guide aims to provide an overview of performing ALS in a pre-hospital environment for an out-of-hospital cardiac arrest (OOHCA). This guide is based on the Resuscitation Council (UK) guidance and is intended only for students preparing for their OSCEs and not for patient care.
Advanced life support
Advanced life support (ALS) builds on basic life support (BLS) to provide patients with a higher level of care, increasing the likelihood of survival in the event of a cardiac arrest.
To achieve this, ALS involves defibrillation, intravenous or intraosseous access, drugs, and advanced airway management. ALS is a team effort, and all parties must work together to provide the best possible outcome.
ALS can be performed by anyone with the appropriate training such as doctors, nurses, paramedics, and other allied health professionals.
Initial assessment
The role of the initial assessment is first to confirm the scene is safe to work in, then to identify the patient and their condition. It needs to be careful and quick to give the patient the best chance of survival.
Safety
Initial patient assessment should always begin with ensuring both personal and scene safety.
Scene safety includes ensuring the environment is safe: there needs to be a clear area around the patient to allow medical staff to work, and that environment needs to be free from hazards. If appropriate, the patient should be moved to an open and safe area to allow 360° access, and patients on chairs or beds should be moved onto the floor to allow for effective compressions.
Personal safety must also be maintained through personal protective equipment (PPE). This will normally include gloves and a type IIR facemask as a minimum, but may also include aprons, gowns, eye protection, an FFP3 mask, a respirator hood and a high-visibility jacket.
Patient assessment
Once the scene is declared safe, approach the patient and begin the assessment:
1. Assessing their level of consciousness. Are they alert or responsive to a verbal or painful stimulus? If they are unresponsive to pain they can be deemed to be unconscious
2. Open and assess the patient’s airway by using either a head-tilt chin-lift or jaw thrust
3. Look, listen, and feel for breathing and a carotid pulse for ten seconds
4. If there is ineffective breathing or no palpable pulse, confirm cardiac arrest and request additional resources/staff to assist
5. Start basic life support at a ratio of 30 compressions to 2 ventilations until a defibrillator arrives
Defibrillation
Once cardiac arrest has been confirmed, the initial priority is defibrillation.
Defibrillation
1. Continue basic life support at a ratio of 30:2
2. Attach defibrillator pads to the patient’s chest (as labelled)
3. Assess the rhythm and shock the patient if appropriate before continuing the ALS algorithm (see below)
4. Rhythm checks should be performed every two minutes, and rescuers performing CPR should be frequently swapped to prevent fatigue and maintain high-quality CPR
Defibrillator safety
When applying defibrillator pads, defibrillation safety should always be considered. To do this, consider the “6Ps“:
- Perspiration: excessive perspiration should be dried to allow pad adhesion
- Pacemakers: defibrillation pads should not be placed over pacemakers
- Patches: defibrillation pads should not be placed over transdermal drug patches. The patches can be removed or pad placement altered
- Piercings: defibrillation pads should not be placed directly over body piercings
- Puddles: patients should be moved into a dry environment before defibrillation
- Explosive environments: for the safety of the patient and rescuers, defibrillation should not occur in a potentially explosive environment
Considering these factors when defibrillating a patient will prevent patient harm and maintain the safety of clinicians and bystanders.
Before defibrillation, no staff or equipment must be touching the patient. CPR should be continued as the defibrillator is charged, and then, a full top-to-toe sweep should be completed. Eyes should be kept on the patient as the shock is delivered to ensure no one accidentally touches the patient. As soon as the shock is delivered, CPR should be restarted, minimising time off the chest.
The ALS algorithm
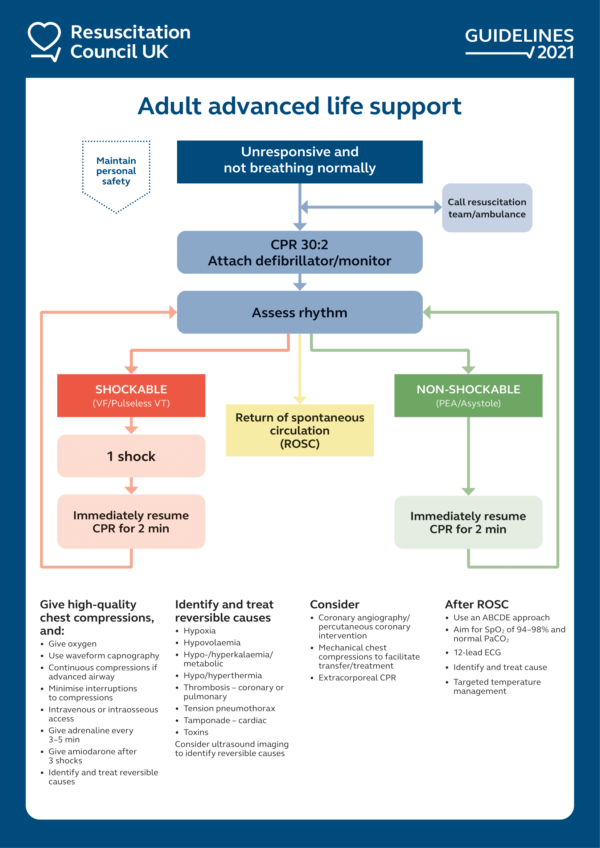
ALS uses an algorithm with two distinct pathways to provide a systematic approach to managing cardiac arrest.
When following the ALS algorithm it is important to remember the basics, with high-quality CPR and early defibrillation being the top priorities, quickly followed by gaining intravenous/intraosseous access and upgrading to an advanced airway.
Actions such as gaining IV/IO access, upgrading the airway, administering drugs and considering reversible causes should be completed during the two minutes of CPR.
There are two sides to the ALS algorithm: shockable and non-shockable.
Shockable rhythms
If the patient is in pulseless ventricular tachycardia (pVT) or ventricular fibrillation (VF) then the shockable algorithm should be used.
1. If the initial rhythm is shockable, provide one shock (at the recommended joules for your equipment)
2. Immediately resume CPR for 2 minutes before performing another rhythm check
3. Increase the joules with each shock in-line with your organisational guidance
4. After the third shock, give 300mg amiodarone and 1mg adrenaline IV/IO
5. Continue adrenaline every 3-5min
6. After the fifth shock, administer amiodarone 150mg
7. Repeat until return of spontaneous circulation (ROSC) is achieved, or the patient moves into the non-shockable side of the algorithm
Tip: always check for a pulse if the monitor shows VT as this rhythm may be a pulsed, perfusing rhythm
Non-shockable rhythms
If the patient is in pulseless electrical activity (PEA), or asystole then the non-shockable algorithm should be used.
1. Immediately resume CPR for 2 minutes before performing another rhythm check
2. Give adrenaline 1mg IV/IO every 3 – 5 minutes
If the patient moves between shockable and non-shockable rhythms, then once the adrenaline has been administered, it should be given every 3-5 minutes, regardless of the rhythm, until ROSC is achieved.
Reversible causes of cardiac arrest
There are eight reversible causes of cardiac arrest, the four Hs and four Ts:
- Hypoxia
- Hypokalaemia/hyperkalaemia
- Hypothermia/hyperthermia
- Hypovolaemia
- Tension pneumothorax
- Tamponade (cardiac)
- Thrombosis
- Toxins
It is important to quickly identify and manage reversible causes during a cardiac arrest scenario. Successful management and reversal of these causes will increase the likelihood of ROSC.
Airway management
Airway management and protection are vital in cardiac arrest to enable appropriate ventilation and oxygenation.
A stepwise approach should be taken towards airway management, with manual techniques being used first, and more advanced equipment being utilised when appropriately trained staff arrive.
For more information on airway management devices, see the Geeky Medics guide to airway equipment.
Oropharyngeal airway (OPA)
An oropharyngeal airway (OPA) should be used during the initial phases of a cardiac arrest as they are quick and easy to insert and work well with a bag valve mask for ventilation.
Nasopharyngeal airway
Nasopharyngeal airways can be used in place of an OPA in the event of trismus or an obstruction in the mouth.
Supraglottic airway / i-gel®
Supraglottic airways are inserted into the pharynx and enable higher-pressure ventilation and expiratory gas monitoring.
There are various supraglottic airways, including laryngeal mask airways (with either inflatable or silicone/rubber cuffs) and the i-gel® with a thermoplastic elastomer used to create a seal around the larynx.
The use of supraglottic airways is common in cardiac arrests due to their relatively simple insertion technique.
Endotracheal intubation
Endotracheal intubation is a specialist skill and should only be attempted by rescuers with a high success rate – 95% achievement within two intubations.
An endotracheal tube is guided through the larynx and into the trachea before an inflatable cuff seals the tube in its place. This allows for high-pressure ventilation as well as significantly reducing the risk of aspiration of stomach contents.
When an advanced airway is in place, the correct placement must be confirmed by auscultation and measurement of end-tidal CO₂ via waveform capnography.
Pit-stop model
When managing a cardiac arrest in a prehospital environment, the location of equipment and identification of team roles is vital to enable well-organised management and mitigate the negative impact of human factors.
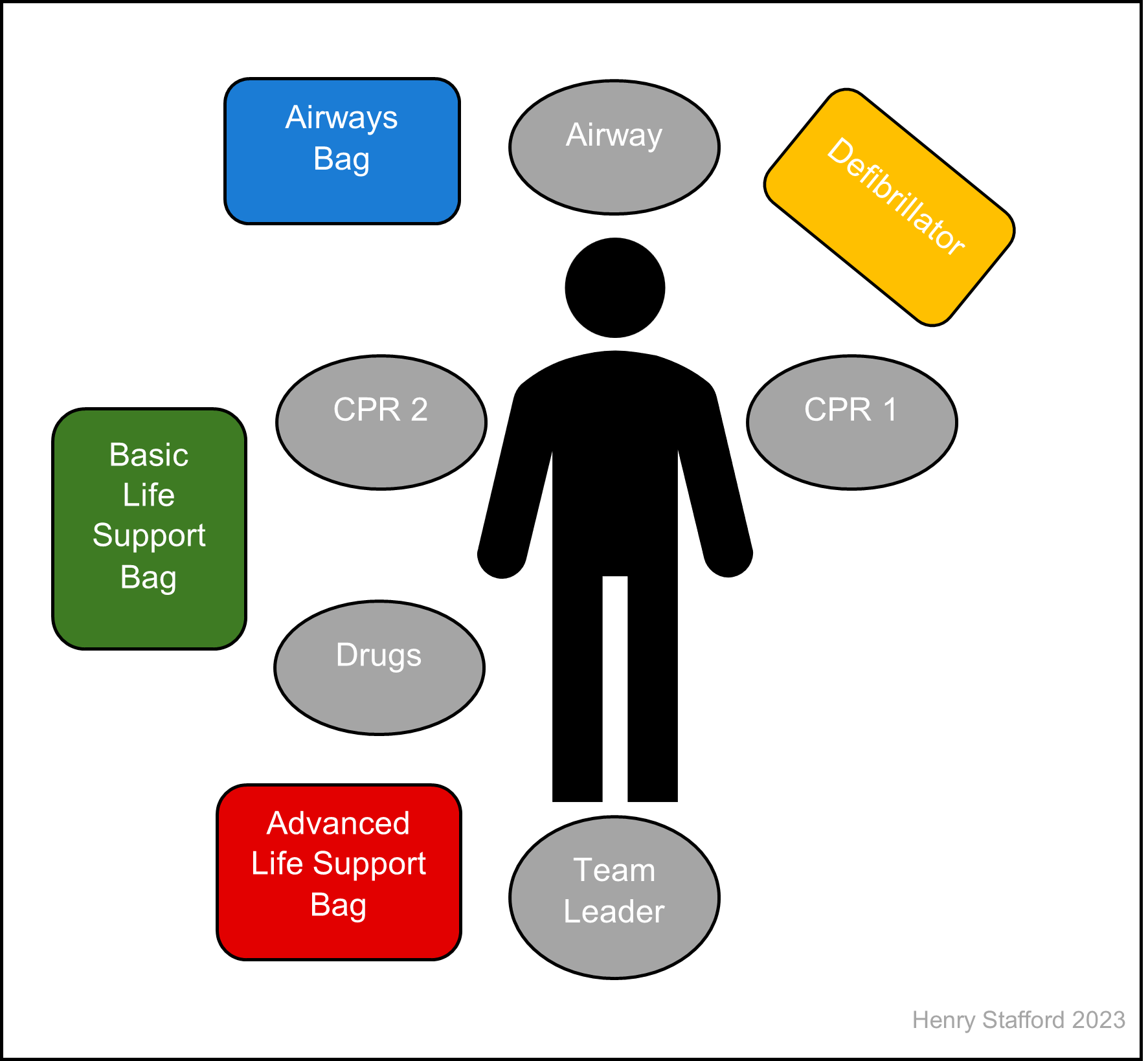
The 360° or pit stop model has been developed so that there is a standardised approach to each cardiac arrest. It enables each member of the resuscitation team to have sufficient space to not interfere with one another, whilst giving them adequate access to the equipment they need.
Defined roles in the 360°/pit stop model include:
- Airway: the person at the very head of the patient with access to basic and advanced airway equipment. They are primarily responsible for airway management but can provide CPR from their position if required.
- CPR 1/defibrillation: positioned on the patient’s left, they are in a good position to provide CPR, whilst having the defibrillator close by. They are in charge of defibrillation if required. The defibrillator should be angled so that it is visible to all members of the team.
- CPR 2: this role depends on the number of clinicians present. They are located to the patient’s right and can alternate chest compressions with CPR 1 or be the airway assistant.
- Drugs: positioned to the patient’s lower right, they are responsible for gaining IV/IO access and administering medications when necessary. They need access to equipment from the basic life support bag, IV/IO equipment and drugs.
- Team leader: should be positioned at the patient’s feet and have a good view of the resuscitation. They should not become directly involved with any particular aspect, but rather direct the team to complete tasks as appropriate. The team leader is responsible for timing the arrest, as well as addressing any reversible causes. If available, the team leader should use a checklist to ensure a systematic and standardised approach.
Should resourcing allow, two more team roles can be created – family liaison and runner. Family liaison works to gain as thorough a history as possible whilst updating family members on what is occurring with the resuscitative efforts. The runner will be in charge of collecting/replacing equipment (e.g. oxygen cylinders) from the site of the arrest to the ambulance.
Special circumstances
In some cardiac arrests, the ALS algorithm is adapted to provide more specific treatment and increase the likelihood of survival.
Anaphylaxis
Anaphylaxis is a severe and life-threatening reaction to an antigen, presenting with rapid onset ABC problems or significant skin/mucosal changes. It can cause global oedema resulting in hypovolemia, as well as swelling to the airway causing significant occlusion.
Early intramuscular adrenaline should be administered in a patient with suspected anaphylaxis. This will significantly reduce the likelihood of cardiac arrest.
Anaphylaxis leads to airway closure due to rapid swelling causing hypoxia, and hypovolemia due to anaphylactic shock. These should be managed as reversible causes in an arrest.
Early intubation should be considered in the anaphylactic patient, as the rapid airway swelling will make management increasingly difficult. Surgical airway intervention may be required in the event of complete airway occlusion.
For more information, see the Geeky Medics guide to the emergency management of anaphylaxis.
Asthma and COPD
COPD and asthma are extremely common in the UK, with 1 in 5 people having lung disease. These conditions can become acutely exacerbated causing hypoxia, potentially leading to cardiac arrest.
The primary cause of cardiac arrest in COPD and asthma patients is hypoxia. Consider early tracheal intubation due to increased intrathoracic pressure.
Provide manual ventilation over mechanical ventilation to reduce the risk of hyperinflation and barotrauma.
Monitor constantly for signs of tension pneumothorax, and treat with thoracostomy as appropriate.
For more information, see the Geeky Medics guides to the emergency management of asthma and the emergency management of COPD.
Drowning
In the UK, around 600 people die by drowning each year. Correctly managing a drowned patient is critical, as early intervention can increase the chances of survival.
Drowning causes respiratory failure through immersion or submersion. As such, the leading cause of cardiac arrest is hypoxia. However, hypothermia and arrhythmias should also be considered.
In water <5°C, hypothermia is likely to be the primary cause, providing some protection against hypoxia.
Palpation of a pulse is unreliable in cold and wet patients. Therefore, ECG and waveform capnography should be utilised to confirm cardiac arrest.
Give five rescue breaths, before continuing standard ALS procedures. Consider early intubation, as high-pressure ventilation may be required due to pulmonary oedema.
Hypothermia
Hypothermia occurs when the environment is too cold for a person’s body to regulate, and the core temperature drops. This decreases cerebral outflow and reduces cardiac output, resulting in cardiac arrest.
To confirm cardiac arrest, look listen and feel for a pulse, ECG activity or breathing for up to one minute.
If the patient’s temperature is below 30°C and VF persists after three defibrillation attempts, withhold further shocks until their temperature rises above 30°C.
No cardiac arrest drugs should be given if the patient’s body temperature is below 30°C.
If the body temperature is 30-34°C, the timing of adrenaline intervals should be doubled to every 6-10 minutes.
All efforts should be made to rewarm the patient, via conventional blankets, heat lamps and warming air blankets.
Where possible, patients should be warmed via extracorporeal life support (ECLS) and extracorporeal membrane oxygenation (ECMO).
Maternal cardiac arrests
Pregnant women experience physiological changes and their bodies are placed under additional stress. Whilst maternal cardiac arrests are relatively infrequent, the correct management is vital for patient survival. There are two patients, both of whom need to be rescued.
Maternal arrests are commonly caused by hypoxia or hypovolaemia. Consider the likelihood of concealed intrauterine bleeding.
Call for specialist help immediately, including obstetrics and neonatology. Consider early intubation to help manage the potentially oedematous airway.
If the patient is more than 20 weeks pregnant, the uterus should be displaced to the patient’s left side. This will reduce aortocaval compression, potentially improving cardiac output.
If possible, apply left lateral tilt to the patient, either by angling the patient’s bed or by placing them on an angled scoop stretcher.
If a ROSC is not achieved within four minutes of cardiac arrest, prepare for the emergency delivery of the foetus.
Obesity
With an increasingly obese population, it is important to recognise how to manage these patients in cardiac arrest situations.
The normal ALS algorithm should be followed. Chest compressions will be increasingly difficult, and rescuers should be swapped more frequently to prevent fatigue. Anticipate difficult intubation and airway management.
Overdose
Intentional or accidental overdoses are becoming increasingly common, with potentially devastating effects.
Always maintain personal safety, especially if the cause is unknown or likely to be part of a CBRNE incident.
Use specific antidotes as appropriate (e.g. naloxone).
Prolonged CPR may be appropriate for this cohort of patients, and a good neurological outcome is possible. Extracorporeal cardiopulmonary resuscitation (ECPR) may be appropriate.
For more information, view our guides on benzodiazepine, opioid, salicylate, and tricyclic antidepressant overdose.
Opioid overdose
Of all drugs taken in overdose, opioids have been consistently shown to be the most likely to cause death. Respiratory arrest usually leads to cardiac arrest, with hypoxia as the primary reversible cause.
In opiate overdoses, naloxone can be administered:
- Provide an initial dose of 400mcg IV/IO
- Subsequent doses should be 800mcg IV/IO, every 60 seconds
- Doses should be titrated until the patient can maintain their own airway
- If there has been no response after 10mg of naloxone, another cause for the arrest should be considered
- Naloxone administration should not compromise good quality CPR, early defibrillation, or airway management
For more information, see the Geeky Medics guide to the emergency management of an opioid overdose.
Sepsis
Infection and sepsis are one of the leading causes of hospital admission, with patients being at high risk of deterioration into septic shock. When this occurs, blood pressure drops and body systems fail to receive sufficient oxygen, potentially causing cardiac arrest.
When managing a cardiac arrest due to sepsis, follow the standard ALS algorithm and provide a 500ml fluid bolus as soon as possible.
For more information, see the Geeky Medics guide to the emergency management of sepsis.
Return of spontaneous circulation (ROSC)
Return of spontaneous circulation (ROSC) is when the heart sustains an electrical rhythm compatible with life and cardiac output, following a cardiac arrest.
If ROSC is achieved, a full ABCDE assessment and basic observations (vital signs) should be undertaken. It is important to remember the high likelihood of the patient re-arresting and prepare to intervene if necessary.
Airway
The patency of the airway should be re-assessed. Consider upgrading to an advanced airway if suitably trained. If the patient no longer tolerates an advanced airway, it can be removed.
Breathing
Oxygen saturations should be maintained at 94 – 98% to prevent hypoxia or hyperoxia.
If the patient is breathing at a sustainable rate (above 10 breaths per minute) allow them to self-ventilate. Assistance may be required if they are hypoventilating, which can be via bag-valve-mask or preferably a mechanical ventilator.
Measure end-tidal CO₂ and aim for a capnography reading of 4.6-6.0kPa (35-40mmHg), with a good waveform.
Circulation
Following a cardiac arrest, repeat 12-lead ECGs should be performed to highlight any significant changes (e.g. ST-segment elevation).
Aim to maintain systolic blood pressure >100mmHg.
Disability
Most patients will have a significantly reduced level of consciousness post-ROSC.
However, in some cases, they may become agitated and combative. In these situations, senior clinicians should be consulted to consider sedation or anaesthesia.
Exposure
The patient’s temperature should be measured and appropriately managed, and they should be covered to maintain their dignity.
Extrication
The decision to transport a cardiac arrest patient is complex, and decision-making should be based on clinical factors, including:
- Presenting rhythm
- Time without CPR
- Response to treatment
- Likelihood of a reversible cause that is unable to be identified/treated prehospital (such as hyperkalemia)
- Travel time to hospital
- If the cardiac arrest occurred in a public location
The following patient groups should be conveyed to hospital:
- ROSC patients
- Children
- Pregnant women
- Refractory/recurrent VF or pVT
- Patients potentially suitable for primary percutaneous coronary intervention (PPCI)
Extrication method
Extrication of patients is a key skill for paramedics. Each situation will present challenges, such as tight corners, multiple flights of stairs, or the inability to park close to the patient. Extricating patients is a skill which is developed over time and through experience.
If possible, the patient should be lifted onto the stretcher and wheeled to the ambulance. If this is not possible the stretcher should be placed by the door to the property, and the patient should be extricated on a scoop stretcher and/or carry sheet before being loaded onto the stretcher.
Consider using a mechanical ventilator or mechanical CPR device during extrication and conveyance to maximise free resources and minimise the potential for falls and injury.
Termination of resuscitation
In some cases of out-of-hospital cardiac arrest, patients will either be unresponsive to ALS or be in such a critical state that resuscitation would be futile. Identifying these factors is essential for all clinicians to prevent unnecessary resuscitation efforts and maintain patient dignity.
Recognition of life extinct (ROLE)
There are seven main criteria unequivocally associated with death commonly used by ambulance services. These are called the Recognition of life extinct (ROLE) criteria:
- Incineration: >95% full-thickness burns
- Massive cranial destruction
- Decapitation
- Hemicorporectomy or similar massive injury
- Rigor Mortis
- Decomposition
- Hypostasis
Outside of the above criteria, there are other circumstances where resuscitation would be futile or inappropriate to offer. These include:
- The presence of a valid DNACPR/ReSPECT form
- The presence of an advanced decision to refuse treatment
- If a patient is deemed to be in the final stages of an advanced irreversible condition such as cancer, chronic organ failure, neurological conditions and advanced frailty.
- Submersion for over 90 minutes
- >15 minutes since the start of the cardiac arrest with no evidence of bystander and 30 seconds of asystole on the ECG monitor
Termination of resuscitation
Termination of resuscitation in the prehospital environment is a very complex decision balancing factors such as proximity to hospital, availability of enhanced care teams, and the patient’s condition.
There is varying guidance depending on the local ambulance service and presenting rhythm. It is essential to check and follow any local guidelines.
Asystole
The Joint Royal Colleges Ambulance Liaison Committee (JRCALC) advises that termination of resuscitation can occur after 30 minutes of ALS, provided all reversible causes have been addressed, and the patient has been asystolic throughout.
Low amplitude, irregular or wide QRS complexes with a rate under 10 beats per minute are not associated with effective cardiac output. If it has persisted for 30 minutes it can be treated as asystole.
Pulseless electrical activity (PEA)
Policy on termination of pulseless electrical activity varies across the UK and depends on local guidelines.
An increasing number of services utilise remote clinical support to aid crews in making these decisions, allowing discussions between paramedics on scene and advanced paramedics or doctors. Factors that influence terminating a PEA cardiac arrest in the community include:
- Time without CPR
- Overall time in cardiac arrest
- Absence of reversible causes
- Comorbidities
- Changes in presenting rhythm
- The trend and value of ETCO2
- Rate and width of QRS complex
Shockable rhythms
Patients who present in a shockable rhythm will receive defibrillation and anti-arrhythmic drugs. If persistent or refractory VF is present this can indicate myocardial infarction, a potentially reversible cause requiring hospital intervention. As such it is not in routine paramedic practice to terminate the resuscitation of this cohort of patients.
Handover
Ambulance pre-alerts follow a set structure to ensure accurate information is passed to the receiving area. Pre-alerts are passed direct from the prehospital clinician or via the emergency operations centre (EOC).
Information passed will normally follow an ATMIST or SBAR structure. For more information, see our guide to pre-hospital communication.
For an out-of-hospital cardiac arrest, the following information will normally be provided:
- Approximate age
- Presenting rhythm of the arrest and current rhythm
- Suspected aetiology of the arrest
- Any ROSC and length of time maintained
- Any requests for patient care on arrival (e.g sedation or advanced airway management)
- Estimated time of arrival
Information may be limited depending on the circumstances and location of the out-of-hospital cardiac arrest.
Reviewer
Ashley Price
Editor
Dr Chris Jefferies
References
- National Water Safety Forum, 2015. A future without drowning: The UK Drowning Prevention Strategy 2016-2026. [Online]. Available from: [LINK]
- Resuscitation Council UK, 2021. Adult advanced life support Guidelines. [Online]. Available from: [LINK]
- Resuscitation Council UK, 2021. Post-resuscitation care Guidelines. [Online]. Available from: [LINK]
- Resuscitation Council UK, 2021. Special Circumstances Guidelines. [Online]. Available from: [LINK]
- The Sepsis Trust, 2022. Yellow Manual – 6th Edition. [Online]. Available from: [LINK]
- Hopkins, C., Burk, C., Moser, S., Meersman, J., Baldwin, C., & Youngquist, S. (2016). Implementation of Pit Crew Approach and Cardiopulmonary Resuscitation Metrics for Out-of-Hospital Cardiac Arrest Improves Patient Survival and Neurological Outcome. Journal of the American Heart Association, 5(1). doi:10.1161/JAHA.115.002892




