- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Pulmonary hypertension (PH) is a pathophysiological disorder occurring when mean pulmonary artery pressure is >25mmHg at rest when assessed with right heart catheterisation.
Pulmonary hypertension is an umbrella term for many different diseases which lead to increased pressure in the pulmonary arteries.1
Pulmonary arterial hypertension (PAH) is a subtype of PH, characterised by pre-capillary pulmonary hypertension in the absence of other causes (e.g. lung disease or other systemic diseases).1
In the United Kingdom, the prevalence of PH has been reported as 97 cases per million. Left heart disease has been reported as the most common cause.1
Aetiology
There are many causes of pulmonary hypertension and therefore pathophysiology depends on the underlying aetiology.
In general, pulmonary hypertension occurs when the pulmonary arteries become narrowed (due to hypoxic pulmonary vasoconstriction or thrombosis), thickened or damaged causing increased pressure in the vessels.
In addition, left heart disease can reduce flow from the right side of the heart, and in turn increase the pulmonary artery pressure.2
Table 1. An overview of the subtypes of pulmonary hypertension.1
| Subtype | Description |
|
Pulmonary arterial hypertension (PAH) |
Can be idiopathic (IPAH), inherited, associated with other systemic diseases (e.g. HIV or connective tissue disordered) or medication-related (e.g. selective serotonin reuptake inhibitors) |
|
Pulmonary hypertension due to left heart disease |
Left heart disease includes left ventricular dysfunction (both systolic and diastolic), valve disease, inflow/outflow tract obstruction and congenital cardiomyopathies. |
|
Pulmonary hypertension due to lung disease |
Causes include chronic obstructive pulmonary disease, interstitial lung disease, obstructive sleep apnoea and chronic high-altitude exposure. |
|
Chronic thromboembolic pulmonary hypertension (CTEPH) and other pulmonary artery obstructions |
Caused by obstruction of the vascular bed (e.g. due to chronic pulmonary embolism). Rarer causes include intravascular tumours and arteritis. |
|
Pulmonary hypertension with unclear/multifactorial mechanisms |
Can be associated with conditions including:
|
Risk factors
Risk factors are related to the subtype of PH (Table 1) and may include:
- Pre-existing diseases: lung disease, left heart disease, congenital heart disease, connective tissue disorders
- Obesity and sleep apnoea
- Altitude: prolonged exposure to high altitude
Risk factors for pulmonary arterial hypertension include family history and female gender.5
Clinical features
History
Symptoms of PH are related to gradually worsening right ventricular function. Initially, symptoms are worse on exertion but can occur at rest in severe cases.1
Typical symptoms of PH include:
- Shortness of breath
- Weakness and fatigue
- Chest pain
- Syncope
- Haemoptysis (uncommon but may be present in chronic thromboembolic disease or due to abnormal distribution of blood flow leading bronchial artery rupture)
It is also important to ask about family history of PAH and medication history (including SSRIs and weight loss medication).
Clinical examination
In the context of PH, a thorough cardiovascular examination is required.
Typical clinical findings may include:1
- Loud pulmonary component of S2
- Third heart sound
- Pansystolic murmur (tricuspid regurgitation) and diastolic murmur (pulmonary regurgitation)
In later stages of PH, clinical findings may include:
- Ascites and peripheral oedema
- Parasternal heave
- Elevated jugular venous pressure
- Hepatomegaly
There may be clinical features specific to the disease responsible for pulmonary hypertension (e.g. connective tissue disease or interstitial lung disease).
Investigations
The most useful initial investigation in suspected cases of pulmonary hypertension is an echocardiogram to estimate pulmonary pressure. In cases of suspected pulmonary arterial hypertension, right heart catheterisation is usually performed.
Bedside investigations
Relevant bedside investigations include:
- ECG: to look for evidence of right ventricular strain including right ventricular hypertrophy, right axis deviation, right bundle branch block, and arrhythmias (atrial flutter and fibrillation may be present in later stages). A normal ECG does not exclude PH.1
Laboratory investigations
Relevant laboratory investigations include:
- Liver function tests: to assess for liver disease
- Serology: to look for HIV and hepatitis
- Autoimmune screen: to look for evidence of connective tissue disease (e.g. anti-centromere antibodies and U3-RNP in scleroderma)
- Arterial blood gas: to look for evidence of respiratory disease
Imaging
Relevant imaging investigations include:
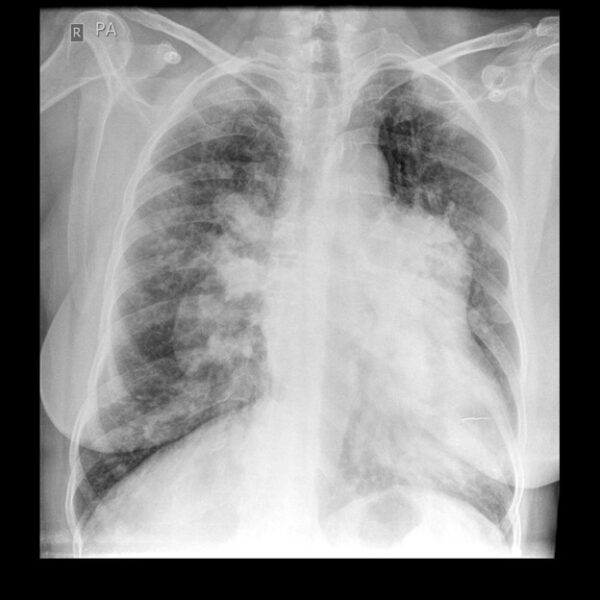
- Chest X-ray: to assess for signs of underlying lung disease or left ventricular dysfunction (pulmonary venous congestion). PAH may present with central pulmonary arterial dilatation, ‘pruning’ of peripheral vessels, right atrial and ventricular enlargement (later stages). A normal chest X-ray does not exclude PH.1
- Echocardiography: to assess right ventricular function and estimate pulmonary arterial pressure.
- Ventilation/perfusion (V/Q) scan and/or CT chest: to look for chronic thromboembolic disease or other underlying lung diseases. A CT may also be helpful for prognostication.
- Cardiac MRI: to help assess cardiac structure and function, and assist with prognostication.
Other investigations
Other relevant investigations include:
- Pulmonary function tests and overnight oximetry: to look for signs of underlying lung disease as an aetiology. PAH can lead to mild/moderate reduction in lung volumes.
- Right heart catheterisation: used to diagnose PAH, assess severity and guide treatment.
- Genetic testing: in specific patients with PAH.
Management
Management varies depending on the underlying cause of PH.
It is important to treat the underlying cause and refer to specialist services for PAH or severe PH.1
Conservative management
All patients should be advised on the following conservative measures:1
- Exercise (within symptom limits) and rehabilitation
- Influenza and pneumococcal vaccination
- Contraceptive advice (pregnancy is associated with 30-50% mortality in PAH patients)
- Psychosocial support
Medical management
Medical management differs depending on the underly cause of pulmonary hypertension.
For patients with PAH, medical management has uncertain long-term outcomes. Options that may be considered under specialist guidance include:1
- Diuretics: for symptomatic benefits in decompensated right heart failure.
- Long term oxygen therapy including ambulatory oxygen.
- Digoxin: improves cardiac output acutely but has unknown efficacy in the long term.
- Oral anticoagulation: there is thought to be increased risk of thrombosis intrinsically as part of the disease process and through comorbid factors including immobility and heart failure.
- Specific drug therapy: calcium channel blockers, endothelin receptor antagonists (i.e. bosentan), phosphodiesterase inhibitors (e.g. sildenafil), prostanoids and prostacyclin analogues.
Cardiopulmonary transplantation
Cardiopulmonary transplant is used in selected cases. There is a good prognosis with long term immunosuppressive therapy.7
Complications
Complications relate to worsening right heart failure and include:
- Peripheral oedema
- Severe exertional dyspnoea
Pneumonia and sudden cardiac death (including during childbirth) can also occur.3
Prognosis
Prognosis in untreated idiopathic PAH has been reported recently as at least 5 years and has a better prognosis than PAH associated with systemic sclerosis.
PH has a varying prognosis depending on the underlying disorder.3
Key points
- Pulmonary hypertension (PH) is defined as a mean pulmonary arterial pressure >25mmHg.
- Pulmonary arterial hypertension (PAH) is a subtype of PH, characterised by pre-capillary PH in the absence of other causes (such as lung disease or other rare diseases).
- Clinical features include worsening breathlessness and signs of right heart failure.
- Important investigations include echocardiography to estimate pulmonary pressures and right heart catheterisation in suspected PAH.
- Management in PH comprises treating the underlying aetiology and the involvement of specialist centres for patients with PAH and severe PH.
- Various medical treatments are used in PAH with limited evidence for their benefit. Cardiopulmonary transplant has been used with success in certain cases.
- Complications include worsening right heart failure, pneumonia and sudden cardiac death.
Reviewer
Dr Alison Moody
Respiratory Consultant
North Devon District Hospital
Editor
Dr Chris Jefferies
References
- European Society of Cardiology/European Respiratory Society. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Published in 2015. Available from: [LINK].
- British Lung Foundation. What causes pulmonary hypertension? Published in 2019. Available from: [LINK].
- Tidy C. Pulmonary Hypertension. Patient.info. Published in 2015. Available from: [LINK].
- Galiè N et al. Pulmonary arterial hypertension associated to connective tissue diseases. Published in 2005. Available from: [LINK].
- Pulmonary Hypertension Association. Risk factors. Published in 2017. Available from: [LINK].
- Dr Bernardo Jose Meza / Radiopaedia.org. ‘Pulmonary hypertension’. License: [CC-BY-NC-SA]. Available from: [LINK].
- Toyoda Y et al. Long-term outcome of lung and heart-lung transplantation for idiopathic pulmonary arterial hypertension. The Annals of Thoracic Surgery. Published in 2008. Available from: [LINK].