- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
The aim of radiotherapy is to deliver carefully calculated doses of radiation to cancer cells, whilst minimising the radiation exposure to surrounding tissues. Radiotherapy, therefore, aims to achieve a high rate of local tumour control with a low risk of complications.2
In comparison to other treatments used in cancer management such as chemotherapy or immunotherapy, radiotherapy is a local treatment. It can be used alone or in conjunction with other treatment modalities (e.g chemotherapy, surgery, immunotherapy).1
Approximately 50% of cancer patients will receive radiotherapy at some point during the management of their illness.3 Radiotherapy is thought to contribute to approximately 40% of the curative treatment of cancers.4
Radiotherapy is an image-guided intervention and involves imaging at all stages of the process including staging, simulation, treatment planning and follow-up.5
The past few decades have seen rapid developments in the field of radiotherapy. There have been significant developments in imaging, treatment planning systems, and understanding of tumour biology and cell growth.4 These advances have enabled higher doses of radiation to be safely delivered to tumours with minimal damage to adjacent normal tissue.1
How radiotherapy is used in the treatment of cancer
Radiotherapy (RT) can be used as the sole radical treatment for cancer (e.g. prostate cancer).1
Radiotherapy can also be used alongside surgical management:
- Prior to surgery (neoadjuvant RT to shrink a tumour before surgical resection)
- During surgery (intraoperative RT)
- After surgical resection (adjuvant RT)
Radiotherapy can also be administered alongside systemic therapies such as chemotherapy and immunotherapy.6
Palliative treatment
Radiotherapy can play an important role in the palliation of symptoms for cancer patients.1
Examples include:
- Radiotherapy to a tumour causing spinal cord compression (thus reducing neuropathic symptoms)
- Radiotherapy to bony metastasis to reduce pain
How radiotherapy works
Radiotherapy uses high energy radiation to eliminate cancer cells.
The radiation used is ionising, meaning it forms ions (charged particles) which then deposit energy into the cells of the tissues they pass through.8
Radiation causes cell death in one of two ways:
- Triggering direct cell apoptosis by causing significant DNA damage
- Preventing cancer cell proliferation, by causing single and double-stranded breaks in DNA (known as mitotic cell death)2
In comparison to healthy cells, cancer cells have a reduced capacity to repair their DNA.3
Radiotherapy dosage
Radiotherapy is delivered in fractions (i.e. sessions) until the total prescribed cumulative dose has been delivered.
The amount of energy absorbed is measured in Grays (commonly abbreviated as Gy).2
Fractionation helps to reduce the risk of acute tissue reactions and minimises damage to normal cells (which are better able to undergo repair between fractions).7
Radiotherapy planning and simulation
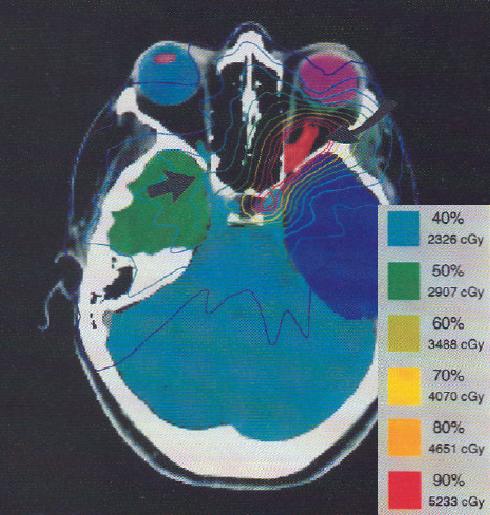
The process of radiotherapy planning involves using imaging to determine where the radiation is to be aimed, using the principle of maximising the radiation dose to abnormal cancer cells while minimising exposure to normal cells.2
Margins are placed around the gross tumour volume to encompass microscopic disease spread. The aim is to deliver higher dosing to the tumour volumes, and comparably lower dosing to vulnerable anatomical structures such as the bladder, small bowel, rectum, and femoral head.9
Simulation is a custom radiation planning appointment, which places the patient in a reproducible position for their radiotherapy.7
The CT allows the relevant anatomy to be viewed from the direction of the radiation beam. Once enough information is obtained, small tattoos or markers may be placed on the patient to line up with laser beams in the treatment room. Immobilisers and moulds are also used to maintain the patient in the same position so that the exact position can be recreated in each radiation treatment session.4
Methods of radiotherapy
There are two primary methods of delivering radiation to tumours:
- External beam radiation: delivered from outside the body by aiming high-energy rays (e.g. protons, photons, particle radiation) towards the cancer’s location (this is the most common radiation delivery method).7
- Internal radiation (brachytherapy): uses radioactive sources in catheters or seeds to deliver radiation from inside the body directly into the tumour site.4 As the radioactive sources tend to be placed directly next to the tumour, a high dose of radiation is delivered to the tumour whilst surrounding healthy tissue is exposed to a relatively small dose.1 Brachytherapy is often used in the management of cervical and prostate cancers.4
Side effects of radiotherapy
The side effects of radiotherapy significantly impact patient quality of life and can limit the dose of radiation able to be delivered.3
Side effects of radiotherapy are usually local, unlike chemotherapy or immunotherapy which tend to produce systemic side effects.7
Early side effects
The early side effects of radiotherapy manifest within a few weeks of completing a course of radiotherapy and include:7
- Skin reactions (erythema, desquamation)
- Fatigue
- Mucositis
- Diarrhoea
- Nausea
Early side effects tend to resolve within a few weeks of onset.7
Late side effects
Late side effects of radiotherapy typically occur months to years after a course of radiation.7
Excessive extracellular matrix, deposition of collagen and fibrinogenesis play key roles in the aetiology of several later stage radiotherapy side effects.6
Late side effects include:11
- Radiation-induced fibrosis
- Atrophy
- Neural or vascular damage
- A range of endocrine effects (e.g. diabetes, hypothyroidism)
Later side effects tend to be irreversible and may be progressive.7
Site-specific side effects
Side effects of head and neck radiotherapy include:
- Dysphagia
- Jaw stiffness
- Dry mouth
- Mouth and gum sores
- Hair loss
- Lymphoedema
- Tooth decay
Side effects of chest radiotherapy include:11,12
- Dysphagia
- Dyspnoea
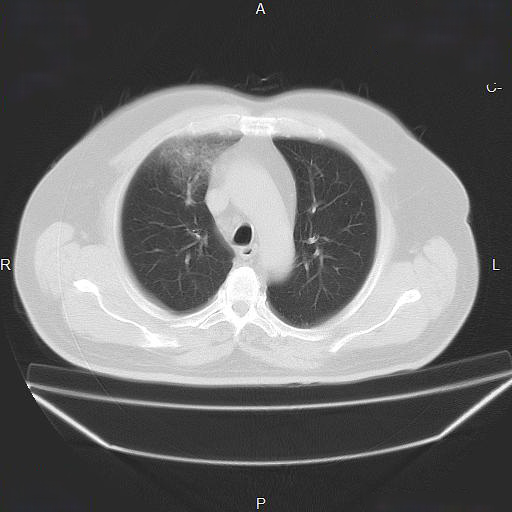
- Radiation pneumonitis (Figure 2): can manifest as cough, chest pain and fevers
- Radiation fibrosis: the result of permanent lung scarring as a result of untreated radiation pneumonitis
Side effects of abdominal radiotherapy include:11
- Nausea and vomiting
- Diarrhoea
- Loss of appetite
- Abdominal cramping
Radiotherapy carries a small risk of inducing a secondary malignancy due to radiation-associated DNA damage.6
More recent radiotherapy techniques such as conformal therapy, intensity-modulated radiotherapy and stereotactic radiosurgery use the advances in diagnostic medical imaging to minimise the dose of radiation delivered to healthy tissues, reducing associated side effects.1
Key points
- Radiotherapy involves the use of ionising radiation to treat cancers.
- The goal of radiotherapy is to maximise the dose of radiation delivered to cancer cells whilst minimising exposure to healthy cells.
- Radiotherapy is typically delivered in fractions and the amount of radiation administered is measured in Grays.
- Radiotherapy causes side effects associated with the tissues the ionising radiation passes through.
- Accurate and precise transmission of radiation to the tumour site minimises the side effects associated with radiotherapy.
Reviewer
Dr Chellaraj Benjamin
Consultant Radiation Oncologist
Auckland City Hospital
Editor
Dr Chris Jefferies
References
- Bernier J, Hall EJ, Giaccia A. Radiation oncology: a century of achievements. Published in 2004. Available from: [LINK]
- Garibaldi C, Jereczek-Fossa BA, Marvaso G, Dicuonzo S, Rojas DP, Cattani F, Ricotti R. Recent advances in radiation oncology. Published in 2017. Available from: [LINK]
- Martin OA, Martin RF. Cancer Radiotherapy: Understanding the Price of Tumor Eradication. Published in 2020. Available from: [LINK]
- Baskar R, Lee KA, Yeo R, Yeoh KW. Cancer and radiotherapy: current advances and future directions. Published in 2012. Available from: [LINK]
- Xing L, Thorndyke B, Schreibmann E, Yang Y, Li TF, Kim GY, Luxton G, Koong A. Overview of image-guided radiotherapy. Published in 2006. Available from: [LINK]
- Bentzen, SM. Preventing or reducing late side effects of radiotherapy: radiobiology meets molecular pathology. Published in 2006. Available from: [LINK]
- Camporeale J. Basics of radiation treatment. Published in 2008. Available from: [LINK]
- Bortfeld T, Jeraj R. The physical basis and future of radiotherapy. Published in 2011. Available from: [LINK]
- Walls G M, Hanna GG , McAleer JJ. Learning radiotherapy: the state of the art. Published in 2020. Available from: [LINK]
- Topperdoc. Treatment plan for an Optic nerve sheath meningioma. License: [Public domain]
- Cancer Research UK. Radiotherapy side effects. Published in 2020. Available from: [LINK]
- Galan N. What are the side effects of radiation for breast cancer?. Published in 2018. Available from: [LINK]
- Asadov R / Radiopaedia. Radiation pneumonitis. License: [CC-BY-NC-SA]




